7. Overall, this delivery system has been highly effective in providing appropriate analgesia for postoperative patients.
a. PCA, when compared to nurse-administered opioids, whether IV or IM, provides better analgesia and patient satisfaction (10).
b. It is very effective for peripheral and lower abdominal surgery, but neuraxial opioids appear superior for upper abdominal and thoracic procedures (see Section IV).
B. The PCA modality has been adapted to subcutaneous, perineural, and epidural catheters, and has been highly effective with the targeted delivery systems discussed in the subsequent text.
III. Local and peripheral nerve analgesic techniques. Several local and peripheral regional techniques are used to provide ongoing analgesia. The advantages of specifically targeting analgesia to one area include minimal limitations of mobility and reduction of systemic side effects such as sedation and nausea. Peripheral infusions usually employ low concentrations of local anesthetics, but opioids and α2-agonists are also useful in some situations. The efficacy and popularity of continuous peripheral techniques have been enhanced by the introduction of new continuous catheter delivery systems and smaller portable pumps.
A. Surgical wound infiltration
1. Simple infiltration of the wound with dilute local anesthetic can provide 4 to 8 hours of analgesia, depending on the location.
a. This technique is particularly useful in the pediatric patient, especially with penile or groin blocks following urologic surgery.
b. Local infiltration is also effective for adult outpatients, allowing them to be discharged without the side effects of systemic opioids.
2. For inpatients, the analgesia in smaller wounds can be extended by the insertion of a multiorifice catheter and provision of a continuous infusion of solutions such as 0.1% bupivacaine or ropivacaine at 6 to 12 mL/h. Orthopaedic surgeons have used this technology with disposable pumps to provide 24 hours of analgesia after shoulder surgery for outpatients.
3. Another variation of this is injection of the knee joint following arthroscopic surgery. Bupivacaine will provide several hours of analgesia, and there is a suggestion that the addition of opioids such as morphine may prolong the analgesia considerably (11), although this remains controversial.
B. Intrapleural Catheters
1. Injection of local anesthetics through intrapleural catheters has been used to relieve postoperative pain. The technique is described in Chapter 10.
2. For postoperative analgesia, 20 mL 0.5% bupivacaine can be injected every 6 to 12 hours, or a continuous infusion can be instituted. Satisfactory results have been reported in some patients with subcostal incisions for cholecystectomy as well as with thoracotomy patients. Other authors have found variable analgesia and a significant potential for systemic toxicity with the doses required.
3. This technique is not as effective as epidural opiates for thoracotomy procedures (12).
C. Repeated intercostal blockade
1. Injection of the 6th to the 11th intercostal nerves with 3 to 5 mL 0.25% bupivacaine with 1:200,000 epinephrine at 12-hour intervals will provide excellent continuous analgesia (12). It is utilized infrequently because of the personnel and time required to provide reinjections every 12 hours, compared to the ease and efficacy of epidural infusions.
2. Insertion of a continuous catheter will reduce some of the technical and time problems. Its use is usually limited to the occasional frail patient requiring special attention, or the trauma patient suffering from multiple rib fractures in whom respiratory depression from systemic opioids is undesirable and epidural analgesia is contraindicated.
D. Peripheral nerve catheters. Peripheral nerve blocks provide excellent postoperative analgesia for both inpatients and outpatients, which can be prolonged with continuous catheters (13,14). Interest in this technique has rapidly increased over the last decade as a result of new technology that aids in the placement (stimulating catheters, ultrasound guidance) and management (reliable, portable, and disposable pumps) of these blocks.
1. See previous chapters for an in-depth discussion of the placement of peripheral nerve catheters (Chapters 15 and 16 for lower extremity and Chapter 12 for upper extremity).
2. Delivery systems
a. Pumps designed for PCA, such as inpatient epidural analgesia, can be used to deliver local anesthetic (with or without adjuncts) to the peripheral nerve catheter.
b. Portable pumps are available that can allow patients to be discharged home with the catheter in place (see Chapter 5).
(1) Early generation included elastomeric spheres that delivered solutions at a specific continuous rate, without bolus capabilities, until empty or discontinued.
(2) Newer models are disposable battery-operated pumps with light emitting diode (LED) display/controls that allow a set continuous rate and intermittent patient-controlled boluses. These pumps are filled with 2 to 3 days of local anesthetic solution and once empty are discarded. Patients can remove their own catheters at home, under their anesthesia provider’s direction.
3. Drugs
a. Dilute local anesthetic solutions are the most commonly used, especially long-acting amides. Ropivacaine 0.2% offers similar analgesic profile as 0.15% bupivacaine with potentially less motor blockade and lower cardiotoxicity risk.
b. Adjuncts such as clonidine and opioids have been advocated by some (15), whereas others have failed to show a clinically relevant benefit.
4. Outcomes
a. Interscalene catheters, used for 2 days postoperatively, can decrease pain and opioid use (along with such adverse effects as nausea and sleep disturbance) in patients undergoing moderately painful ambulatory shoulder surgery (14).
b. Femoral nerve catheters provide better pain relief, improve the recovery time, and shorten the rehabilitation time following total knee replacement after inpatient surgery, compared to conventional opioids or epidural infusions (16). However, long-term functional outcomes, such as mobility, are likely no different between continuous and single-shot femoral nerve blocks in these patients (16).
c. Feasibility studies have demonstrated that with the use of portable delivery systems, total joint replacements (including knees, hips, and shoulders) can be done in a subset of patients as overnight-stay or outpatient procedures (17,18).
5. Complications and adverse effects are rare. Local inflammation and infection rates are less than 1% even when catheters remain in place for 4 to 7 days (19). Even outpatient use of continuous techniques has been associated with few major complications (20). Knotting of catheters around anatomic structures, including nerves, has been reported (21).
IV. Neuraxial opioid analgesia
A. The use of neuraxial administration of opioids has been the major advancement in acute analgesic therapy (22,23).
1. Opioids applied to the spinal cord are effective in blocking pain perception at the dorsal root entry zone in doses that are substantially smaller than those required to produce systemic analgesia.
2. The direct application of opioids to the specific receptor site reduces the systemic side effects of respiratory depression and sedation usually associated with IM and IV injection.
3. This effect is seen with both subarachnoid and epidural injection, although epidural application requires higher doses (by a factor of 10) to produce penetration of the membranes.
4. This route has been demonstrated to produce superior analgesia for thoracotomy and abdominal procedures (12,24–26).
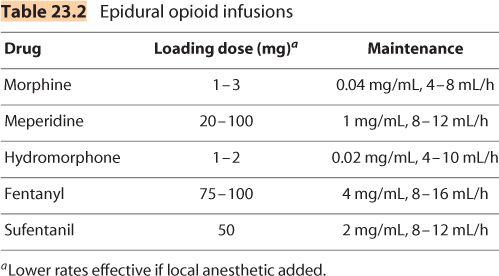
B. Choice of opioids. Virtually all of the opioids have been employed in both the subarachnoid and epidural space (Table 23.2).
1. Epidural delivery
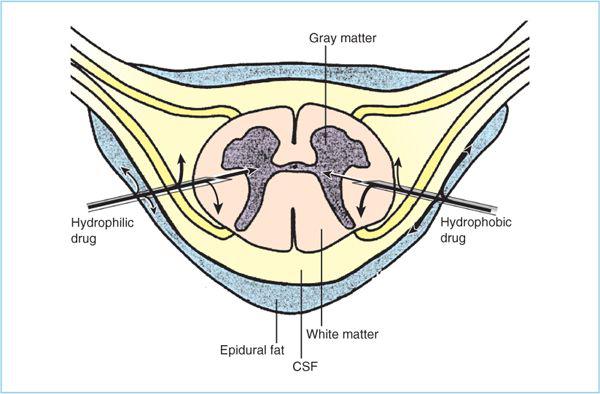
a. Morphine. Because of its poor lipid solubility, morphine has a relatively slow penetration into the lipid layers of the spinal column (22). Although early investigators found that they could overcome this by using higher doses, it was quickly discovered that these doses were also associated with a higher incidence of side effects, specifically the production of central sedation and respiratory depression as the water-soluble morphine diffused cephalad in the cerebrospinal fluid (CSF) (Figure 23.1).
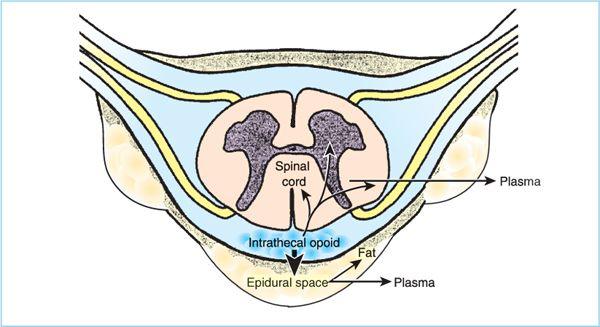
Figure 23.1. Any drug placed in the epidural space will distribute among local tissues based on its physicochemical properties. For example, relative to hydrophilic drugs, hydrophobic drugs will be taken up into epidural fat to a greater degree, cleared into plasma to a greater extent as they diffuse through the rich capillary network in the dura mater, reside in cerebrospinal fluid (CSF) for a much shorter period of time and be sequestered in the rich lipid environment of the spinal cord white matter to a greater degree. As a result, relative to hydrophilic drugs, a much smaller percentage of the administered dose of a hydrophobic drug reaches the spinal cord dorsal horn. If the drug is a local anesthetic this is not a significant problem because the site of action is the relatively hydrophobic environment (i.e., myelinated axons) of the nerve rootlets suspended in CSF. However, for drugs that target receptors in the spinal cord dorsal horn (e.g., opioids, α2-agonists, etc.), a significant amount of the drug administered epidurally is taken up into other tissues, thereby reducing the bioavailability of the drug in the dorsal horn.
(1) Appropriate low bolus doses [1–5 mg for most patients, based primarily on patient age (27)] will produce adequate pain relief with minimal side effects if a single dose is administered early enough to allow 60 minutes for the onset of action.
(2) Use of a continuous infusion of morphine avoids the peak and valley phenomenon of intermittent injections, and also appears to be associated with a lower incidence of side effects (28).
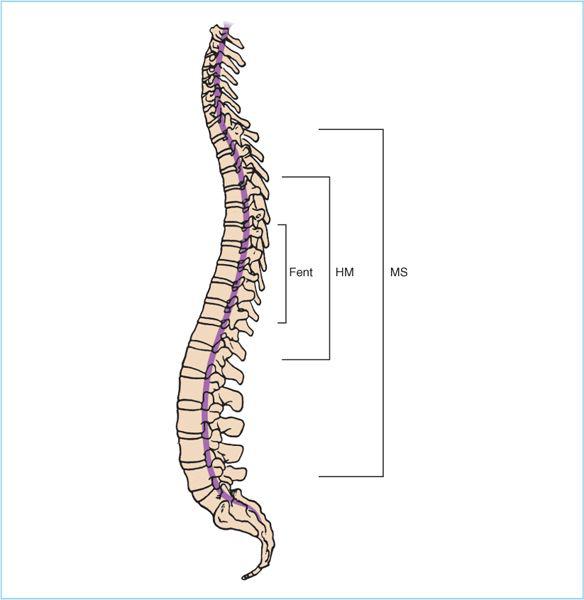
b. Fentanyl. Because this drug has higher lipid solubility, it diffuses less readily in the CSF (Figure 23.2). Historically, it was thought that fentanyl (as the prototypical highly lipid-soluble opioid) would produce a more localized segmental band of analgesia with less likelihood of centrally mediated respiratory depression and other side effects. Currently, many disagree on whether epidural fentanyl provides a significant effect at the spinal cord versus largely systemic effect from plasma absorption (see Chapter 7).
Figure 23.2. The extent of spread of epidurally administered opioids is related to the degree of water solubility. Less water-soluble drugs such as fentanyl (Fent) will produce a narrow band of segmental analgesia surrounding the insertion site, while hydromorphone (HM) and morphine (MS) will produce wider bands of analgesia.
(1) Epidural fentanyl has been shown to produce localized segmental anesthesia as required for post-thoracotomy pain (12,23), with some suggestion of a lower side effect profile (29).
(2) There is significant uptake into the blood stream (30), and in several studies the blood levels attained with epidural infusion have equaled the blood levels with IV administration. Some have questioned whether there is really a direct spinal action at all, and whether these drugs have any use in neuraxial analgesia (31,32).
(3) Other data suggest that with bolus doses, rather than by infusion, there is a local effect in the spinal cord, but only near the immediate area of injection (33).
(4) Despite the laboratory studies suggesting only systemic effects, there are large clinical studies demonstrating a high degree of effectiveness with epidural fentanyl infusions (29,34). These series demonstrate that the location of the catheter tip is critical; it must be located near the dermatomal source of pain. They also demonstrate that the combination with a local anesthetic is important for adequate analgesia with this opioid. If a large number of spinal segments are to be provided analgesia, higher doses (and systemic effects) may be required, and alternative opioids with a wider spread may be more desirable.
c. Sufentanil. Because of its higher lipid solubility, even larger doses are required. For effective analgesia, doses of sufentanil equivalent to the fentanyl dose are required. Although sufentanil may be an effective analgesic, there is nevertheless concern that its effects are also simply due to systemic blood levels. As with fentanyl, this has been confirmed when higher doses are used. The use of higher volumes of a more dilute solution for sufentanil infusions will improve its analgesic effects, but advantages of this drug over fentanyl are unclear.
d. Meperidine, hydromorphone. The use of intermediate-solubility opioids such as meperidine or hydromorphone provides a spinal cord action with wider spread and duration than seen with fentanyl, and perhaps less frequent side effects (35–37). This class may represent an ideal balance of good spread with lower side effects.
e. Optimizing epidural opioid delivery. Generally, there appears to be a relationship that suggests that drugs producing sufficient spread to provide excellent analgesia (morphine) do so at the price of side effects. The lower frequency of side effects of the lipid-soluble drugs is associated with lower efficacy, unless such high infusion rates are used that systemic levels are attained. This has led many to believe that the use of the lipid-soluble drugs should be limited to cases where the catheter is at or near the “epicenter” of a narrow band of painful dermatomes, such as thoracotomy incisions (and therefore pain can be relieved with small doses). The more water-soluble opioids appear to be more appropriate for distant catheters (lumbar placement for thoracotomy pain) or wider incisions (abdominal cases). Unfortunately, there are insufficient comparative studies between the various opioids to support the personal choice of drug.
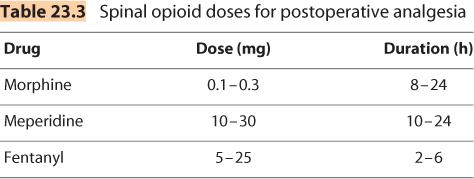
2. Intrathecal delivery
a. All of the opioids have also been administered as subarachnoid injections. The doses required are significantly less than the epidural route, but the efficacy of this route is limited by the (usually) single injection. (Table 23.3)
b. After administration, intrathecal opioids not only bind to receptors in the dorsal horn of the spinal cord but also traverse the dura mater into the epidural space, travel in the CSF to more cephalad binding sites, and enter the plasma. As with epidural opioids, the degree of binding is related to the drug’s lipophilicity (38).
(1) Lipophilic opioids like fentanyl and sufentanil rapidly cross the dura into the epidural space and rapidly bind to spinal cord receptors and are cleared into the plasma. Such pharmacodynamics limits the analgesic duration but also the degree of side effects, including respiratory depression (Figure 23.3).
(2) Morphine, as a hydrophilic compound, remains in the CSF for a longer duration. While this prolongs the analgesia (24 hours or more), it also significantly increases the risk of cephalad spread of the drug, which may lead to respiratory depression. There is a narrow dose–response relationship, and a relatively high incidence of side effects (39). Although respiratory depression is the greatest concern, it is fortunately rare (less than 0.5%). Decreased level of consciousness is a more reliable indicator of respiratory depression than pulse oximetry or respiratory rates. Nausea and urinary retention can also occur, each with an incidence of approximately 30%. Most common is pruritus, disturbing more than half of the patients.
Figure 23.3. Disposition of opioid after intrathecal administration. After intrathecal administration, the disposition of opioids is complex and multicompartmental. Simultaneously, intrathecal opioids (i) travel cephalad within the cerebrospinal fluid (CSF), (ii) enter the spinal cord, and (iii) traverse the dura mater to enter the epidural space. The clinical properties of each opioid (speed of onset, duration of action) and degree of rostral spread result from the sum of effects for each route. Lipophilic opioids (fentanyl/sufentanil) display rapid onset, limited and brief rostral spread and a narrow band of analgesia surrounding the site of injection, and a relatively short duration of action. In contrast, the hydrophilic opioid morphine traverses the dura slowly to the epidural space, demonstrating slow onset, extensive and prolonged rostral spread and a broad band of analgesia surrounding the site of injection, and a relatively long duration of action. (Adapted from Rathmell JP, Lair TR, Nauman B. The role of intrathecal drugs in the treatment of acute pain. Anesth Analg 2005;101(Suppl 5):S30–S43.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree