Initial Assessment and Management
In all cases, approach the patient without condemnation. If the patient has a reduced level of consciousness or immediately appears unwell:
- Protect the airway.
- Administer a high concentration of oxygen by mask.
- Obtain venous access.
- Control fits with intravenous (IV) diazepam.
- Connect the patient to monitoring devices – ECG, BP (blood pressure) and SaO2 (arterial O2 saturation); measurement of core temperature is also important.
- Measure the blood glucose.
- Request an urgent ECG.
- Seek senior/anaesthetic advice.
Further Assessment and Management
Ask About
- Nature of substance taken
- Type of preparation taken.
- Other substances (e.g. alcohol) also taken. Ask specifically about paracetamol and aspirin. Poisoning with these two drugs is common, dangerous and treatable
- Route of poisoning (e.g. oral, IV)
- Time taken
- Intended result of poisoning
- Previous episodes of poisoning.
Look For
- Dyspnoea, bronchospasm and pulmonary oedema
- Tachycardia and hypotension
- Dysrhythmias and widening of the QRS complex
- Depressed level of consciousness
- Agitation, restlessness and hallucinations
- Pupillary changes
- Extensor plantar reflexes
- Lowered or raised core temperature.
Specific Actions
- Measure the plasma urea and electrolytes (U&ES) and glucose.
- Consider the need to measure the blood gases, plasma osmolality and plasma chloride. The osmolar gap and the anion gap can then be calculated → p. 221.
- Measure or screen for plasma aspirin and paracetamol levels 4 h after the estimated time of ingestion.
- Obtain a 12-lead ECG.
- Seek specific poisons advice (Sources of advice → p. 271).
- Consider the need for gastric decontamination (→ later).
- Consider the need for specific supportive measures (→ p. 271).
- Consider requesting toxicology levels (e.g. lithium, iron, theophylline, methanol, ethylene glycol, digoxin, paraquat and carboxyhaemoglobin).
- Consider the need for specific therapies (→ below).
In patients with a reduced level of consciousness, consider the need to:
- give IV saline (at least 10 mL/kg) unless there is a specific contraindication
- catheterise the bladder and measure the urine output.
Metabolic Acidosis, Anion Gap and Osmolar Gap in Poisoning
A metabolic acidosis with an increased anion gap (and a normal chloride concentration) indicates retention of non-volatile organic acids such as may be present in renal failure, ketoacidosis and lactic acidosis, or following the ingestion of substances such as methanol, ethylene glycol, salicylate and iron. In the absence of circulatory failure, diabetes, alcoholism or uraemia, an increased anion gap clearly indicates poisoning with one or more of these substances.
An increased osmolar gap indicates that one or more substances are present in high molar concentrations. Most drugs, including salicylates, are not identified this way because they are dissociated or do not attain high enough serum concentrations on a molar basis. The ingested substances best able to increase the osmolar gap are those that have a low molecular weight and are present in high mass units – such as the lower alcohols and glycols. Poisoning with methanol or ethylene glycol commonly causes severe metabolic acidosis and elevation of both the anion and osmolar gaps → p. 221.
Gastric Decontamination
Controversy still surrounds the efficacy of the different modes of gastric decontamination although none is a mainstay of modern treatment. All methods aim to reduce the absorption of residual toxins from the gastrointestinal (GI) tract. The risks must be carefully weighed against the likely benefits. Any form of gastric decontamination is of doubtful value if more than 1 hour has passed since the ingestion of poisons, except in specific cases:
Gastric Lavage
Gastric lavage is effective only if the substance ingested is still in the stomach → above. It should be reserved for intubated patients with a depressed level of consciousness from unknown substances or specific indications such as highly toxic drugs. It may be useful to remove large quantities of alcohol in patients with acute poisoning. A general anaesthetic may sometimes be necessary, especially in children. Gastric lavage is contraindicated in the following circumstances:
- There are not adequate facilities and skills available to protect the airway or deal with any complications that might arise.
- The substance taken is relatively safe (e.g. benzodiazepines).
- The substance ingested is safer in the stomach than anywhere else. This applies to the following:
- Oily or petroleum-based substances: relatively harmless in the stomach, but accidental spillage into the lungs during lavage will cause a life-threatening pneumonitis.
- Corrosives and caustics: may cause oesophageal perforation, especially with the help of a lavage tube.
- Oily or petroleum-based substances: relatively harmless in the stomach, but accidental spillage into the lungs during lavage will cause a life-threatening pneumonitis.
Technique of gastric lavage → Box 15.1.
 Box 15.1 Procedure for Gastric Lavage
Box 15.1 Procedure for Gastric Lavage- Move the patient to the resuscitation area
- Secure the airway; request anaesthetic help if required
- Put the patient in the recovery position on a tiltable trolley The stomach is easier to drain in the right lateral position
- Monitor the patient’s SaO2 throughout the procedure
- Have a high-volume suction pump switched on
- Carefully insert a lubricated lavage tube
- Siphon the gastric contents into a bucket, checking for tablet material; gentle pressure over the stomach may facilitate drainage
- Lavage the stomach with warm water or saline until the drainage fluid is clear; in small children isotonic fluids in aliquots of 10 mL/kg should be used
- Instil activated charcoal if indicated → later
- Remove the lavage tube
Emesis and Whole Bowel Irrigation
Emesis removes at least as much material from the stomach as gastric lavage. It also has the same contraindications as lavage → before. It is possible to vomit up tablets, which would not fit through the small Murphy’s eye of a lavage tube. However, emesis is dangerous in obtunded patients and activated charcoal cannot be subsequently given. For this reason, emesis is no longer routinely recommended in the UK. For those situations or in places where there is no alternative, syrup of ipecacuanha is usually used to induce vomiting (30 mL in an adult and 15 mL in a child). It should be followed by a reasonable volume of fluid and can be repeated after 20 min if necessary.
Whole bowel irrigation is also of doubtful value and has not been shown to improve outcomes.
Milk
Milk is often advocated to assuage the effects of ingested substances that are:
- irritant
- of low toxicity
- dangerous to remove by lavage or emesis.
Activated Charcoal
Heating of charcoal with chemical activators increases its surface area to between 1000 and 2000 m2/g and thus enhances its ability to reversibly absorb small molecules. (A standard 50-g dose has an internal surface area that is larger than 20 football pitches!)
Activated charcoal will not absorb:
- iron, lithium and other metallic compounds
- cyanides
- strong acids and alkalis
- alcohols
- petroleum distillates
- malathion and DDT.
Repeated administration of charcoal
absorbs drugs re-excreted into the bowel via the enteroenteral and enterohepatic circulations. This ‘gastrointestinal dialysis’ is indicated for:
- theophyllines
- carbamazepine
- phenobarbital
- quinine
- dapsone
and may be useful for:
- tricyclic and related antidepressants
- barbiturates
- salicylates
- sotalol
- phenytoin
- paraquat
- digoxin and other cardiac glycosides
- ciclosporin.
Activated charcoal should be administered in a dose equal to 10 times that of the poison to be absorbed. An initial dose of 50–100 g (or 1 g/kg for children) will usually ensure that this ratio is met. Paracetamol and aspirin are taken in gram rather than milligram quantities and so a second dose of charcoal may be needed after a few hours. For repeated dosing 50 g (1 g/kg) should be given every 4 h or smaller doses more frequently. Large doses of charcoal may form concretions in the bowel and so lactulose (or sorbitol) should be given with each repeated dose.
Treatment of Respiratory Depression
There are four main factors:
Specific respiratory stimulants (e.g. doxapram) have little place in the treatment of drug-induced respiratory depression.
Treatment of Circulatory Depression
This involves the following:
- Maintenance of adequate oxygen supply to the heart → before
- Maintenance of normovolaemia – IV fluids; vasoconstrictors (e.g. ephedrine) are sometimes used in specific treatment situations
- Correction of cardiac dysrhythmias – may need specialist advice to avoid dangerous interactions (e.g. prolongation of the Q–T interval → p. 174)
- Correction of bradycardia – atropine initially; may need an adrenaline infusion or cardiac pacing (→ p. 164)
- Maintenance of cardiac contractility – inotropes such as dobutamine (→ p. 238). Specialist monitoring is necessary to optimise cardiac output in this situation.
Treatment of Hyperthermia
Hyperthermia may result from the following:
Treatment must be promptly instituted to prevent the development of multiorgan failure. Cooling measures include:
- removal of clothing
- cool sponging and promotion of evaporation with an electric fan
- placement of ice-packs in the axillae and groins
- infusion of cooled IV fluids
- gastric lavage with cool fluids in the unresponsive (intubated) patient
- administration of oral or rectal paracetamol.
Exotic lavages of cool fluids into the peritoneal and pleural cavities, colon and bladder are often advocated but are usually impractical in the ED. Drugs that may be used in some situations by the specialist to promote cooling include the following:
- Chlorpromazine: vasodilator, sedative, hypothermic effect
- Diazepam: muscle relaxant and sedative
- Dantrolene: muscle relaxant. Dantrolene is used for the treatment of malignant hyperthermia and as such is kept in all operating theatres. Its use should usually be discussed with an intensivist. An initial dose of 1 mg/kg is given intravenously over 10 min, repeated if necessary every 15 min to a maximum of 10 mg/kg in 24 h.
Poisons Information Services
Specific poisons information may be obtained from the following:
Management of Poisoning with Unknown Substance(s)
- Obtain as much history and background information as possible; consider alternative diagnoses.
- Examine the patient and his or her clothing and possessions for further clues. Beware of needles in the pockets.
- Consider trauma or coexistent disease.
- Monitor the patient.
- Check the blood sugar.
- Send off blood for full blood count (FBC), blood chemistry, and aspirin and paracetamol screen.
- Consider the need for ECG and blood gases. Plasma osmolality can be a useful test to establish the presence of extraneous substances in the blood (→ p. 221).
- Consider the administration of activated charcoal.
- Administer IV fluids and measure urine output.
- Admit for observation.
POISONING WITH COMMON MEDICINES
The frequency with which poisoning with a drug occurs usually reflects its availability in a society.
Paracetamol (Acetaminophen)
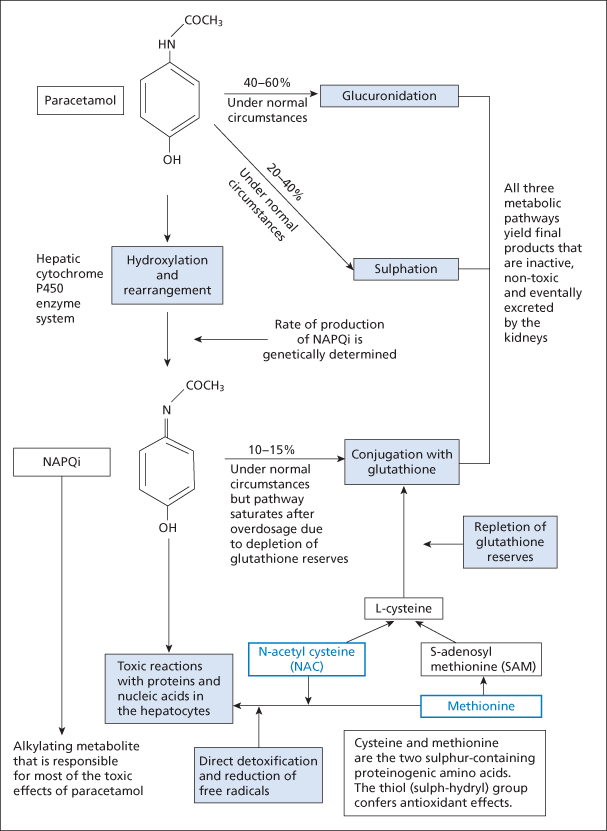
Paracetamol is the most common drug involved in self-poisoning in the UK. This reflects its widespread usage and over-the-counter availability. It is also a common ingredient in compound tablets, combined with opiates, caffeine and many other drugs. The only early features of isolated paracetamol poisoning are nausea and vomiting, which usually settle within 24 h. Malaise beyond this time, especially if accompanied by right subcostal pain and tenderness, usually indicates the development of hepatocellular necrosis, the major toxic effect of paracetamol poisoning. There may also sometimes be delayed renal tubular necrosis, usually in association with liver damage. These serious problems occur 3–4 days after ingestion, although patients may sometimes present even later with:
- hypoglycaemia
- bleeding
- encephalopathy and cerebral oedema.
The fatal dose of paracetamol may be as low as 10–15 g (20–30 tablets). Fortunately, the specific antidotes, N-acetylcysteine and methionine, are very effective if given early enough. Children rarely ingest large quantities of paracetamol and so deaths attributable to this drug before the teenage years (and especially age <6 years) are extremely unusual.
TX
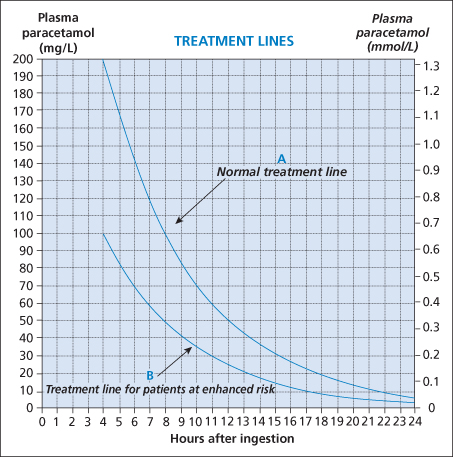
All patients should have their plasma paracetamol concentration measured as soon as 4 h have passed since the ingestion (measurements before 4 h have passed are unreliable because of continuing absorption and distribution). The plasma salicylate should be simultaneously measured because patients are not always able to differentiate between the two drugs. The need for specific treatment can usually be determined from this single measurement when it is plotted on a reference treatment curve (→ Figure 15.1). If the time of ingestion is in doubt, the worst case option should be assumed to have occurred. After 15 h, the estimates of risk are less reliable and clinical judgement is more important.
The usual antidote is IV N-acetylcysteine (NAC) (→ Box 15.2), but up to 10% of patients treated with this drug may have an allergic response to it, with 3–6% having a severe reaction (→ Box 15.3). Patients who are given IV NAC despite having plasma paracetamol levels that are not in the toxic range are more likely to have these reactions. Oral methionine is an alternative to IV NAC that is widely used in some countries (→ Box 15.4). Some patients have an increased risk of liver damage after paracetamol ingestion (→ Box 15.5). Antidote treatment should be instituted for these patients if their plasma paracetamol concentration is 50% or more of the normal reference treatment value (→ Figure 15.1).
- For very obese patients (i.e. body weight >110 kg), the dose of NAC should be calculated on a maximum weight of 110 kg.
- For children >20 kg, use the same dose of NAC in half the volume of 5% glucose. For children <20 kg, the same dose can be used in a still smaller volume of fluid (e.g. aliquot 1 = 3 mL/kg, aliquot 2 = 7 mL/kg and aliquot 3 = 14 mL/kg).
- Physiological (0.9%) saline may be substituted for 5% glucose.
- In exceptional circumstances without IV access, NAC may be administered by mouth. (But it is poorly tolerated because of the high doses required due to its low oral bioavailability. It also has a very unpleasant taste and odour and causes nausea and vomiting.)
- nausea
- flushing
- itching, urticaria and other erythematous rashes
- angio-oedema
- bronchospasm
- hypotension or (rarely) hypertension
 Box 15.4 Treatment with Oral Methionine
Box 15.4 Treatment with Oral Methionine- past or present allergic reaction to N-acetylcysteine
- difficulty obtaining, or maintaining, IV access
- patient refuses other treatment
- patient is going to take own discharge
- awaiting plasma paracetamol concentration
- patient is nauseous or vomiting
- activated charcoal has been given (it will absorb methionine)
 Box 15.5 Patients at Special Risk of Liver Damage (Treated According to the ‘High Risk’ Line on the Graph in Figure 15.1)
Box 15.5 Patients at Special Risk of Liver Damage (Treated According to the ‘High Risk’ Line on the Graph in Figure 15.1)- Has a condition that causes glutathione depletion (i.e. malnutrition, cachexia, failure to thrive, anorexia nervosa and other eating disorders, malabsorption states and chronic debilitating illnesses, including cystic fibrosis, malignancies, alcoholism, hepatitis C, HIV infection and AIDS)
- Is taking hepatic enzyme-inducing drugs such as carbamazepine, phenytoin, phenobarbital, primadone, rifampicin, rifabutin, efavirenz, nevirapine or St John’s wort
- Drinks excessive amounts of alcohol (>21 units/week in males and >14 units/week in females)
Figure 15.2 The mechanism of action of antidotes in paracetamol toxicity. NAPQi, N-acetyl-p-benzoquinoneimine.
Patients who have received NAC or methionine will subsequently require measurements of clotting time (international normalised ratio or INR), glucose, U&Es and creatinine. Vitamin K should be given if the INR is increased (>2) with fresh frozen plasma (FFP) and clotting factors reserved for active bleeding.
Patients with signs of liver damage should be discussed early on with a specialised liver unit. This would include those with:
- INR >3.0
- elevated plasma creatinine (>300 mcmol/L)
- hypoglycaemia
- severe acidosis (arterial pH <7.3 or lactate >3.5 mmol/L)
- encephalopathy
- hypotension (mean arterial pressure <60 mmHg)
- pre-existing liver disease.
Severe liver damage after paracetamol poisoning has been defined as a peak plasma alanine aminotransferase (ALT) activity exceeding 1000 IU/L. An aspartate aminotransferase (AST) level >1000 IU/L is similarly diagnostic. Most patients who are clinically unwell have peak ALT and AST levels of several thousand units per litre. In clinical practice, the prothrombin time (PT) or INR is a more accurate test for assessing prognosis.
Children:
paracetamol poisoning with paediatric preparations is rarely serious as toxic amounts are not usually ingested. In addition, young children may metabolise the drug differently from adults. However, children poisoned with adult preparations may be at risk of liver damage and so assessment and treatment are virtually identical to those for adults. Nausea and vomiting are very common in children who have ingested excessive amounts of paracetamol. If there is a certainty of an accidental ingestion of a single dose of paracetamol of <150 mg/kg (or 75 mg/kg in children at enhanced risk → Box 15.5), then measurement of paracetamol levels is unnecessary and the child can be discharged. However, all children with deliberate self-poisoning, including those who have taken insignificant amounts, should be admitted for child psychiatric assessment → p. 365.
Management of Patients Who Present Within 8 h of Ingestion
- For patients who present within 1 h of a significant ingestion, give activated charcoal 50 g, although it is of unproven benefit in this situation.
- Assess whether the patient is at an enhanced risk of severe liver damage (→ Box 15.5).
- Measure the plasma paracetamol concentration as soon as 4 h or more have elapsed since the ingestion.
- Start treatment with NAC if the plasma paracetamol level is on or above the relevant treatment line (→ Figure 15.1) (for normal patients, this is 200 mg/L at 4 h and 110 mg/L at 8 h, and for high-risk patients 100 mg/L at 4 h and 55 mg/L at 8 h). If the paracetamol concentration is unavailable within 8 h of ingestion and if >150 mg/kg (or 12 g) of paracetamol has been taken, then the antidote should be started anyway and treatment stopped if the result subsequently indicates that it was not required.
- Arrange admission to a medical ward or psychiatric referral as appropriate. Patients who have received NAC within 8 h of a paracetamol overdose can be expected to be fit for discharge on completion of its administration. However, INR, ALT and plasma creatinine should be measured before discharge in everyone who has received NAC. Patients should be advised to return to hospital if vomiting or abdominal pain develops or recurs.
Management of Patients Who Present 8–15 h After Ingestion
- Measure the plasma paracetamol concentration immediately. Also take blood for INR, plasma creatinine and ALT.
- Start IV NAC, without delay, while waiting for the paracetamol concentration result if a significant amount (>150 mg/kg or total 12 g) is thought to have been taken. The efficacy of the antidote declines progressively from 8 h after ingestion.
- Assess whether the patient is at special risk of severe liver damage (→ Box 15.5).
- Discontinue NAC only if the paracetamol level is below the relevant treatment line (→ Figure 15.1) (for normal patients, 110 mg/L at 8 h and 35 mg/L at 15 h; for high-risk patients, 55 mg/L at 8 h and 15 mg/L at 15 h) and the patient is asymptomatic with a normal INR, plasma creatinine and ALT. If there is any doubt about the timing of the overdose, then continue the infusion of NAC.
- Arrange medical admission or psychiatric referral as appropriate. INR, ALT and plasma creatinine should be measured before discharge in all patients who have received a full course of NAC. Patients should be advised to return to hospital if vomiting or abdominal pain develop or recur.
Management of Patients Who Present 15–24 h After Ingestion
- Measure the plasma paracetamol concentration immediately, together with the INR, ALT, glucose, U&Es, creatinine, LFTs and venous bicarbonate.
- Start IV NAC, without delay, while waiting for the paracetamol concentration result in all patients unless convinced that a significant amount (>150 mg/kg or total 12 g) has not been ingested. Urgent action is required because the efficacy of NAC is limited when more than 15 h have passed since the ingestion.
- Assess whether the patient is at special risk of severe liver damage (→ Box 15.5).
- Discontinue NAC only if the paracetamol level is below the relevant treatment line (→ Figure 15.1) and the patient is asymptomatic with a normal INR, plasma creatinine and ALT. If there is any doubt about the timing of the overdose, then continue the infusion of NAC. The prognostic accuracy of the treatment lines after 15 h is uncertain but a plasma paracetamol concentration above the applicable treatment line should be regarded as indicative of a serious risk of severe live damage.
- Arrange admission for patients with abnormal clotting, renal function or liver enzymes or whose paracetamol level exceeds the relevant treatment line.
- No symptoms
- Normal INR, ALT and creatinine
- Plasma paracetamol concentration <10 mg/L
- Normal mental state (confirmed by psychiatric review) and adequate social circumstances.
Management of Patients Who Present More Than 24 h After Ingestion
- Measure the plasma paracetamol concentration together with the INR, ALT, glucose, U&Es, creatinine, LFTs and venous bicarbonate.
- Start IV NAC immediately in all patients who have taken an overdose of paracetamol within the last 36 h (as recommended by the British National Formulary), unless convinced that a significant amount (>150 mg/kg or total 12 g) has not been ingested.
- Arrange admission or referral if a significant ingestion is thought to have occurred. All patients with abnormal clotting or liver enzymes or renal function require admission and monitoring and should be discussed with a specialist liver unit or the National Poisons Information Service. An infusion of NAC may still be recommended for some of these patients.
Management of Patients Who Ingest a Significant Amount of Paracetamol Over a Short Period of Time, as Opposed to a Single Ingestion (Staggered Overdose)
Staggered overdose of paracetamol is particularly difficult to assess and treat. The paracetamol treatment graph relates to a single acute ingestion rather than ingestion over a period of time.
- Measure the plasma paracetamol concentration, but accept that it is very difficult to interpret.
- These high-risk patients should all be considered for treatment with NAC. They should be discharged only if they are asymptomatic and the INR, ALT and creatinine are normal at 24 h after the last dose of paracetamol.
- In patients who have ingested the paracetamol over <12 h, the plasma paracetamol concentration should be measured again 4 h later. If the second level is more than half the first level, then a significant overdose is likely to have occurred.
Aspirin
Aspirin poisoning is now relatively uncommon. The main features of salicylate toxicity are:
- hyperventilation
- tinnitus and deafness
- vasodilatation
- sweating
- hypoglycaemia (especially in children).
In severe poisoning, convulsions and coma may occur and complex acid–base disturbances are inevitable. Initial stimulation of the respiratory centre causes a respiratory alkalosis. As more of the drug is absorbed, a metabolic acidosis supervenes. In between these two phases there may be a transitory period with a relatively normal blood gas picture.
TX
- Plasma salicylate concentration must be measured in all patients in whom analgesic poisoning is suspected. It is usually measured with the plasma paracetamol level 4 h after ingestion. Peak levels may not be reached, however, for at least 6 h. U&Es, glucose and blood gases must also be measured.
- It is worth attempting to decontaminate the stomach with charcoal for up to 8 h after ingestion as salicylates markedly delay gastric emptying.
- Repeated doses of charcoal may also be useful.
- Intravenous fluid should be administered.
- Forced alkaline diuresis (with sodium bicarbonate 1.26% → p. 252) should be considered in cases of significant poisoning, i.e. when the plasma salicylate concentration is:
- Haemodialysis may be required if the plasma salicylate concentration is >700 mg/L (5.1 mmol/L) or in the presence of a severe metabolic acidosis.
Ibuprofen, Mefenamic Acid and Other NSAIDs
Ibuprofen is of low toxicity; poisoning with <100 mg/kg does not require any treatment. Ingestions in excess of 400 mg/kg will cause symptoms including nausea, vomiting and epigastric pain. Diarrhoea, GI bleeding, headache and tinnitus may also occur, but more severe toxicity (convulsions, central nervous system [CNS] depression and metabolic acidosis) is very uncommon. The half-life of ibuprofen in overdosage is 2–3 h.
Mefenamic acid is the most dangerous non-steroidal anti-inflammatory drug (NSAID) when taken in overdosage. It may cause convulsions.
TX
Ibuprofen and mefenamic acid:
treatment with activated charcoal is indicated if ibuprofen >100 mg/kg has been taken within the preceding hour (or longer for sustained-release preparations). All patients who have ingested in excess of this amount will require observation for at least 4 h and monitoring of plasma electrolytes. A good urine output must be maintained.
Activated charcoal effectively absorbs mefenamic acid and should be considered for all patients, even when only small amounts of the drug have been ingested. Observation and monitoring of plasma electrolytes should be arranged.
Other NSAIDs:
- Ascertain the time and amount of the ingestion.
- Seek specific information concerning the toxicity and treatment of poisoning with that drug.
- Consider the need for gastric decontamination.
- Consider admission for observation and supportive therapy.
Salbutamol
This β2-receptor agonist causes predictable adrenergic side effects:
- Tremor
- Tachycardia
- Agitation and headache
- Hypokalaemia.
TX
- Consider activated charcoal for all patients, especially if a controlled-release preparation has been taken.
- Monitor the heart rate, BP and ECG continuously.
- Measure the U&Es and glucose.
- Consider specific therapy with a cardioselective β blocker. This would probably be contraindicated in patients with a history of bronchospasm.
- Admit for observation and monitoring.
β Blockers
The effects of poisoning vary considerably according to the specific drug. Sotalol in particular, may cause bizarre dysrhythmias (For torsade de pointes and prolongation of the Q–T interval by sotalol → p. 173). In overdosage, most β blockers can cause:
- severe bronchospasm
- bradycardia, hypotension and syncope
- heart failure
- coma and convulsions (especially with propranolol).
TX
- Apply supportive measures.
- Consider activated charcoal in recent ingestions and for modified-release preparations (repeated doses for sotalol in particular).
- Give nebulised salbutamol for wheezing.
- Administer IV atropine for bradycardia and hypotension (up to 3 mg for an adult and 40 mg/kg for a child).
- Give IV glucagon for hypotension refractory to atropine (boluses of 2 mg, up to a maximum of 10 mg for an adult; 50–150 mcg/kg for a child).
- Give IV dobutamine for severe cardiac depression or an infusion of isoprenaline for resistant bradycardia.
- Establish transvenous pacing for intractable bradycardia.
Calcium Channel Blockers
Poisoning with calcium channel blockers causes nausea, vomiting, dizziness, confusion and coma. Metabolic acidosis and hypoglycaemia can occur. Depending on the exact drug, hypotension may be primarily due to cardiac depression (verapamil and diltiazem) or profound vasodilatation (nifedipine), although the selectivity of calcium antagonists tends to disappear on overdosage.
TX
Activated charcoal is effective if given within 1 h of ingestion or after modified-release preparations (when repeated doses may also be considered). IV calcium may be used in severe poisoning → p. 249. For symptomatic bradycardias and hypotension, atropine and inotropes are indicated. An insulin and glucose infusion may be used in the management of severe hypotension and myocardial failure.
Tricyclic and Related Antidepressants
Poisoning with tricyclic antidepressants (TCAs) is dangerous and common, being implicated in over a fifth of all fatal ingestions. Dosulepin is the most common drug involved. Some of the newer cyclic antidepressants – with different ring structures – seem less toxic. Ingested amounts are usually significant because the patient who needs TCAs will often have a mental state compatible with suicide. One in 40 patients who overdoses on TCAs will die. An ingestion of 35 mg/kg is the median lethal dose for an adult.
The effects of TCAs are largely related to their anticholinergic activity and so include peripheral effects such as:
- blurred vision and dry mouth
- dilated pupils
- urinary retention
- diverse GI symptoms
- tachycardia and dysrhythmias
and central effects such as:
- agitation and anxiety
- hyperactivity
- disorientation and confusion
- drowsiness and lethargy
- hallucinations
- nystagmus, dysarthria, ataxia and movement disorders
- hyperreflexia and extensor plantar response
- hyperthermia or hypothermia.
However, the most serious features are probably unrelated to anticholinergic activity:
TX
This depends very much on the time of ingestion and the condition of the patient. Serious complications occur within 12 h of ingestion. Rapid deterioration may occur. Most patients will require the following:
- Gastric decontamination (worthwhile for up to 8 h after ingestion – little absorption of TCAs takes place in the stomach). The administration of activated charcoal may be repeated because charcoal prevents absorption in the small intestine
- A 12-lead ECG
- Referral for monitoring and observation.
Agitation or convulsions should be controlled with IV benzodiazepines.
Patients with a significantly depressed level of consciousness or fitting also require:
- airway protection
- high-concentration oxygen
- blood gas analysis
- monitoring
- anaesthetic advice and a consideration of the need for paralysis and ventilation (this may need to be accompanied by an infusion of thiopental to control fits)
- intensive care unit (ICU) admission.
Cardiovascular complications should be treated by alkalisation (→ later). Antidysrhythmic drugs are best avoided in TCA poisoning because conduction deficits may make the ECG difficult to interpret. Moreover, some of these drugs will produce a synergistic cardiotoxicity. Torsade de pointes should be treated with magnesium (→ p. 250). Mild hypotension usually responds to IV fluids; for more severe hypotension alkalisation is appropriate.
Alkali therapy for TCA poisoning:
induction of an alkalosis with IV sodium bicarbonate reduces mortality in TCA poisoning. The mechanism of action is not fully understood but is related to protein binding of the TCA and the movements of ions into the heart. The benefits of alkalisation are seen not only in patients who are acidotic – those with a minimal or absent base deficit also show improvement. Suggested indications for bicarbonate in TCA-poisoned patients are:
- systemic acidosis
- QRS duration of >120 ms
- ventricular dysrhythmia
- hypotension
- cardiac arrest.
The aim of therapy is to maintain a pH of between 7.50 and 7.55. The initial dose of bicarbonate can be up to 1–2 mmol/kg; further doses will depend on the clinical picture. Hyperventilation can be used as an adjunct to the bicarbonate to help achieve the desired pH.
Selective Serotonin Reuptake Inhibitors
Selective serotonin reuptake inhibitor (SSRI)-type drugs inhibit the reuptake of serotonin (5-hydroxytryptamine or 5HT). Some related compounds (serotonin–noradrenaline reuptake inhibitors or SNRIs) also inhibit the reuptake of noradrenaline. These drugs are widely prescribed for the treatment of depression and consequently self-poisoning with them is common. SSRIs in overdose cause:
- sweating and dizziness
- drowsiness, convulsions and coma
- tachycardia, hypotension or hypertension (prolongation of the Q–T interval and the QRS complex may also occur with consequent ventricular dysrhythmias; torsade de pointes is a particular risk → p. 173).
TX
Activated charcoal may be given if a significant amount of an SSRI has been ingested within the previous hour. Observation for at least 6 h is indicated. Otherwise, treatment is supportive.
Theophylline
Large doses of slow-release theophylline preparations may be taken intentionally. They cause:
- severe and intractable vomiting
- agitation and restlessness
- dilated pupils
- tachycardia and tachydysrhythmias
- convulsions
- haematemesis
- hyperglycaemia and hypokalaemia.
TX
- Consider gastric lavage within 2 h of ingestion and give repeated doses of activated charcoal.
- Administer potassium, anticonvulsants, sedatives and other supportive treatment as indicated.
- Intravenous propranolol may be considered in patients who are not asthmatic to reverse tachycardia, hypokalaemia and hyperglycaemia.
- Large clumps of drug in matrix may require endoscopic removal.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree