Pneumothorax and Barotrauma
Bhiken Naik
CASE SUMMARY
A 28-year-old, 75 kg man is involved in a motor vehicle accident. His injuries include blunt head trauma with an admission Glasgow Coma Scale of 12 and multiple rib fractures on the left, with radiological evidence of an underlying pulmonary contusion. On admission to the emergency room, the arterial blood gas results are: pH 7.34, PO2 52 mmHg, PCO2 26 mmHg, HCO3 2 to 14 mEq per L, and lactic acid 5 mmol per L on a nonrebreathing face mask. Clinical examination reveals a flail segment on the left hemithorax with extensive subcutaneous emphysema, and a chest radiograph demonstrates a left hemopneumothorax. A chest tube is placed, with drainage of approximately 400 mL of blood; however, the patient’s respiratory status worsens. He is intubated and transferred to the surgical intensive care unit for mechanical ventilation. The patient was placed on pressure support and synchronized intermittent mandatory ventilation. Initial ventilator settings were as follows: FiO2 of 60%, pressure support of 10 cm H2O, positive end-expiratory pressure (PEEP) of 10 cm H2O, synchronized intermittent mandatory ventilation rate of 12 breaths per minute and a tidal volume of 600 mL. During the next 48 hours, the patient developed acute respiratory distress syndrome (ARDS) and required escalation of the ventilator parameters. Ventilator settings were readjusted: FiO2 80%, pressure support (PS) 20 cm H2O, PEEP 15 cm H2O, synchronized intermittent mandatory ventilation rate of 14 breaths per minute, and tidal volume of 750 mL. The patient’s respiratory status improved during the next 12 hours, and the FiO2 was weaned to 40%. However, following central venous line placement through the right subclavian route, the peak and plateau inspiratory pressures increased to 40 cm H2O, accompanied by hemodynamic compromise. A presumptive diagnosis of a right-sided tension pneumothorax was made, and needle decompression was performed, with rapid resolution of the ventilatory and hemodynamic instability.
What Baseline Knowledge of Pulmonary Physiology Is Important?
▪ INTRAPLEURAL PHYSIOLOGY
Normal respiration is a cyclical event characterized by an active inspiration phase followed by expiration, which is passive in nature. During quiet breathing, inspiration is achieved by contraction of the diaphragm, which displaces the abdominal contents downward and increases the vertical intrathoracic dimension. During expiration, the lung and chest wall passively return to their resting position.
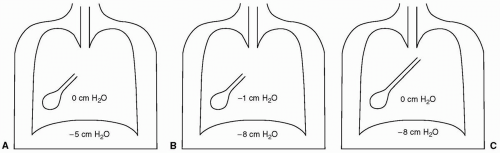
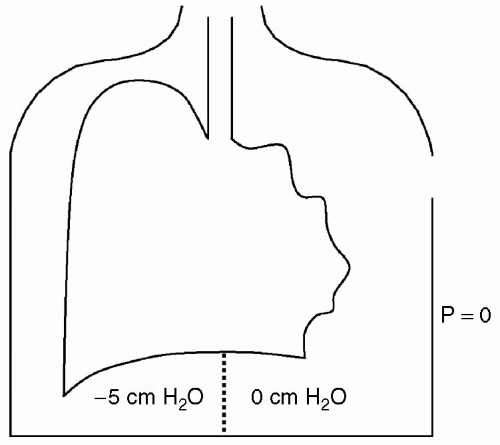
The elastic forces of the lung and chest wall maintain the intrapleural space at subatmospheric pressure (see Fig. 11.1). During inspiration, the intrapleural pressure decreases further, and alveolar pressure becomes subatmospheric, creating a pressure gradient for airflow into the alveoli. In the expiratory phase, the intrapleural pressure rises and alveolar pressure increases, thereby facilitating airflow out of the lung.
▪ PATHOPHYSIOLOGY OF PNEUMOTHORAX AND TENSION PNEUMOTHORAX
When there is loss of integrity of the visceral or parietal pleura, air enters the subatmospheric intrapleural space. The forces opposing the retraction of the lung are reduced, causing the lung to collapse (see Fig. 11.2). Respiratory compromise occurs from altered pulmonary mechanics, the pendeluft effect, and ventilation-perfusion mismatching.
If a flap-valve injury to the pleura develops, air can be entrained into the intrapleural space during inspiration,
with no escape route during expiration. The intrapleural pressure becomes supra-atmospheric, with accompanying severe hemodynamic and respiratory compromise, resulting in a tension pneumothorax (see Fig.11.3).
with no escape route during expiration. The intrapleural pressure becomes supra-atmospheric, with accompanying severe hemodynamic and respiratory compromise, resulting in a tension pneumothorax (see Fig.11.3).
What Are the Common Etiologies of Perioperative Pneumothorax?
A pneumothorax can occur with the disruption of the visceral or parietal pleura, and may occur spontaneously or secondary to a surgical or anesthetic procedure. Table 11.1 lists the common causes of pneumothorax during the perioperative period.
▪ SPONTANEOUS PNEUMOTHORAX
Spontaneous pneumothoraces occur in the absence of thoracic trauma and are classified as primary or secondary.1 A primary spontaneous pneumothorax affects people who have no clinically apparent lung disorders, whereas a secondary pneumothorax occurs in the setting of underlying lung disease.
Primary Spontaneous Pneumothorax
Primary spontaneous pneumothorax has a higher incidence in men, particularly those with a tall, thin body habitus.2 The exact mechanism of spontaneous pneumothorax is not fully understood but is probably multifactorial in nature. Gravitational stress, underperfused alveoli, and abnormal connective tissue may contribute to the development of spontaneous pneumothorax.3 Smoking increases the risk of spontaneous pneumothorax 22-fold in a dosedependent manner.4
The anatomical abnormality found in patients with spontaneous pneumothorax is subpleural bullae. These
subpleural bullae are seen in approximately 76% to 100% of the ipsilateral lung and 79% to 96% of the contralateral lung.5
subpleural bullae are seen in approximately 76% to 100% of the ipsilateral lung and 79% to 96% of the contralateral lung.5
TABLE 11.1 Classification of Pneumothorax | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
If the primary spontaneous pneumothorax is small and the patient is clinically stable, the American College of Chest Physicians recommends observation in the emergency department for 3 to 6 hours and discharge if the repeat chest radiograph does not demonstrate progression of the pneumothorax.1 If the pneumothorax is large, the lung should be reexpanded with a small bore catheter or a thoracostomy tube. In the absence of an air leak, the drainage device can be removed 12 to 24 hours later, providing the chest radiograph demonstrates no evidence of pneumothorax. Persistent air leaks for >4 days should be evaluated for surgery and possible pleurodesis.
Secondary Spontaneous Pneumothorax
Secondary spontaneous pneumothorax can occur because of a variety of causes. These include chronic obstructive airway disease, asthma, pulmonary fibrosis, pulmonary infarction, and infective disorders of the lung, with chronic obstructive pulmonary disease being the most common. Patients complain of a dramatic increase in dyspnea associated with pleuritic chest pain.6 Secondary spontaneous pneumothorax represents a significant marker for mortality in patients with chronic obstructive pulmonary disease, with Videm et al. demonstrating a fourfold increase in mortality.7 In the absence of pleurodesis therapy, the recurrence rate for pneumothorax is 40% to 50%.8 The current recommended treatment for secondary spontaneous pneumothorax is chest thoracostomy followed by surgical pleurodesis, given the potential lethality of recurrent pneumothoraces.1
▪ TRAUMATIC PNEUMOTHORAX
The mechanism of traumatic pneumothorax can be due to blunt or penetrating trauma. Blunt trauma results in widespread energy transfer to the body. In the thoracic area, this action can result in alveolar rupture, esophageal laceration, bronchial tears, and multiple rib fractures that can violate the pleura. In addition, there may be soft tissue, bone, and possible vascular injuries.
Penetrating trauma is classified as high or low velocity. With low velocity-penetrating trauma, the injury is confined to the anatomic track. With high velocity trauma, there may be additional injury distant from the anatomic track, secondary to the accompanying shock wave.
Traumatic pneumothorax can be further subclassified into closed, open, tension, or hemopneumothorax.
Closed Pneumothorax
With closed pneumothorax, there is no violation of the chest wall, and the degree of respiratory dysfunction is related to the patient’s underlying medical condition, associated injuries, and the size of the accompanying pneumothorax.
Open Pneumothorax
Open pneumothoraces communicate with the atmosphere through the chest wall. They can result in severe respiratory embarrassment because of the large amount of air entrained into the pleural cavity during inspiration. They are initially managed by placing moist sterile gauze loosely over the wound, which prevents air from being entrained into the pleural space during inhalation.
Tension Pneumothorax
Tension pneumothorax is a life-threatening emergency and requires prompt identification and decompression of the pleural cavity with a needle thoracostomy, followed by placement of a tube thoracostomy (Fig. 11.3).
Hemopneumothorax
Hemopneumothorax occurs when there is both air and blood within the pleural space. These injuries have to be managed with a large bore tube thoracostomy (e.g., 28 to 32 Fr) to allow adequate drainage and decompression of the pleural cavity. If bleeding from the chest tube is persistent, and the rate exceeds 100 to 200 mL per hour or the total output is >1,000 mL, a thoracotomy should be performed.9
▪ OCCULT PNEUMOTHORAX
Occult pneumothorax is a pneumothorax identified by computed tomography (CT) scan but is not visible by routine chest radiographs. With the increasing use of CT scanning to evaluate polytrauma patients, this entity is being diagnosed with increasing frequency. Hill et al. in a retrospective review of 3,121 patients admitted to a level 1 trauma center, found an incidence of 2.2% for occult pneumothorax.10 The management of occult pneumothorax
remains controversial. There are no large multicenter prospective trials to draw clinically relevant conclusions. In a small retrospective review by Collins et al. it appears that patients who are hemodynamically stable can be managed conservatively with interval chest radiographs.11 However, if the patient requires positive pressure ventilation, it is safer to place a tube thoracostomy to avoid the risk of developing a tension pneumothorax.12
remains controversial. There are no large multicenter prospective trials to draw clinically relevant conclusions. In a small retrospective review by Collins et al. it appears that patients who are hemodynamically stable can be managed conservatively with interval chest radiographs.11 However, if the patient requires positive pressure ventilation, it is safer to place a tube thoracostomy to avoid the risk of developing a tension pneumothorax.12
▪ IATROGENIC PNEUMOTHORAX
Iatrogenic pneumothorax can be caused by a myriad of diagnostic and therapeutic interventions both adjacent and remote from the chest cavity. The common causes of iatrogenic pneumothorax, as reported by Sassoon et al. are transthoracic needle lung biopsy, subclavian vein catheterization, thoracentesis, pleural biopsy, and positive pressure ventilation in decreasing order of frequency.13 During the perioperative period, additional risk factors for developing an iatrogenic pneumothorax are neuraxial blockade, brachial plexus block, anesthesia equipment malfunction, and certain surgical procedures.
Thoracic Neuraxial and Periclavicular Blocks
Although uncommon, several case reports have documented pneumothoraces related to thoracic epidural anesthesia.14 In this scenario, a pneumothorax can be caused by direct needle puncture of the contralateral pleura when the needle angle and the sagittal plane are >30 degrees. Additionally, transintervertebral foramina migration of the epidural catheter has been implicated in precipitating a pneumothorax.15,16
Intercostal nerve blocks provide analgesia for rib fractures, which helps to alleviate the pulmonary complications associated with atelectasis and pneumonia. The incidence of pneumothorax associated with intercostal nerve block procedure varies between 0.073% and 19%.17,18,19 Shanti et al. in a retrospective review of 161 patients undergoing 249 intercostal nerve block procedures, reported an incidence of pneumothorax of 5.6% per patient.20
Periclavicular brachial plexus blocks provide dense anesthesia and analgesia in the upper extremity. The brachial plexus can be blocked at four distinct anatomic areas: Interscalene, supraclavicular, infraclavicular, and axillary. Owing to the close proximity of the brachial plexus to the pleura, a pneumothorax can potentially develop when performing blocks adjacent to the clavicle. The incidence of pneumothorax related to upper extremity plexus blockade varies depending on the type of block being performed (see Table 11.2).20,21,22
Central Venous Cannulation
Central venous catheters are indispensable in modern anesthesia and critical care practice. They provide a means to evaluate central venous pressures, deliver vasoactive agents, and rapidly administer large volumes of fluid. The subclavian, internal, and external jugular veins are the vessels most commonly cannulated. The incidence of pneumothorax is related to the site of cannulation, level of operator experience, and the local anatomy. Mansfield et al. reported a 1.5% incidence of pneumothorax during subclavian vein catheterization. During univariate analysis, gender, body mass index and the number of needle passes were associated with a higher rate of complications.23 The incidence of pneumothorax is lower with the internal jugular approach. Shah et al. described an incidence of 0.5% in their study of more than 6,000 patients undergoing pulmonary artery catheterization.24 The overall incidence for pneumothorax related to central venous cannulation is 0.2% to 0.5% for the internal jugular approach, and 0.5% to 2% for the subclavian vein approach.25
TABLE 11.2 Incidence of Pneumothorax with Various Nerve Blocks | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
Anesthesia Equipment
Incorrect use or malfunction of anesthesia equipment can result in serious pulmonary injury during the perioperative period. The anesthesia delivery machine is supplied with oxygen and air from a wall pipeline at approximately 50 lb per sq in. The oxygen flush valve is connected to this intermediate pressure system and can supply oxygen between 35 and 75 L per minute.26 Activation of the oxygen flush valve during the inspiratory phase of positive pressure ventilation can result in a dramatic increase in the peak airway pressure, thereby increasing the risk of a pneumothorax.
Occasionally, a mucus plug within an endotracheal tube can create a ball-valve effect during intermittent positive pressure ventilation, resulting in pulmonary hyperinflation and subsequent barotrauma.27
Self-inflating bag-valve devices are operated by a variety of health care workers. Improper use of this device can result in airway pressures >135 cm H2O. This occurs when high flows of supplemental oxygen and a decreased or occluded flow through the oxygen reservoir bleed locks the device in the inspiration mode and prevents exhalation.28
Minimally Invasive Surgery
Minimally invasive surgery reduces the tissue trauma associated with the interventional procedure, but still aims to achieve a satisfactory therapeutic result. Laparoscopic intra-abdominal procedures are now routinely performed, and carbon dioxide insufflation combined
with various patient positions can have a major impact on cardiorespiratory function. Pneumothorax during abdominal laparoscopy can cause paradoxical ballooning of the hemidiaphragm, a decrease in lung compliance, hypo-oxygenation, hypercarbia, and pneumothorax. A carbon dioxide pneumothorax has a >90% resolution within 2 hours, whereas a helium pneumothorax remains essentially unchanged during the same time period;29 therefore, expectant management (e.g., observation) with asymptomatic carbon dioxide pneumothoraces can be advocated. On the contrary, helium pneumothoraces do not resolve rapidly and may require aspiration, even in asymptomatic patients.
with various patient positions can have a major impact on cardiorespiratory function. Pneumothorax during abdominal laparoscopy can cause paradoxical ballooning of the hemidiaphragm, a decrease in lung compliance, hypo-oxygenation, hypercarbia, and pneumothorax. A carbon dioxide pneumothorax has a >90% resolution within 2 hours, whereas a helium pneumothorax remains essentially unchanged during the same time period;29 therefore, expectant management (e.g., observation) with asymptomatic carbon dioxide pneumothoraces can be advocated. On the contrary, helium pneumothoraces do not resolve rapidly and may require aspiration, even in asymptomatic patients.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree