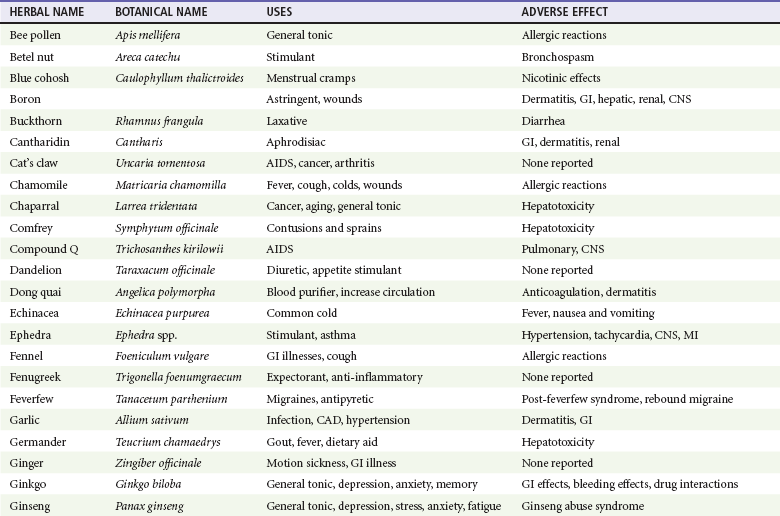
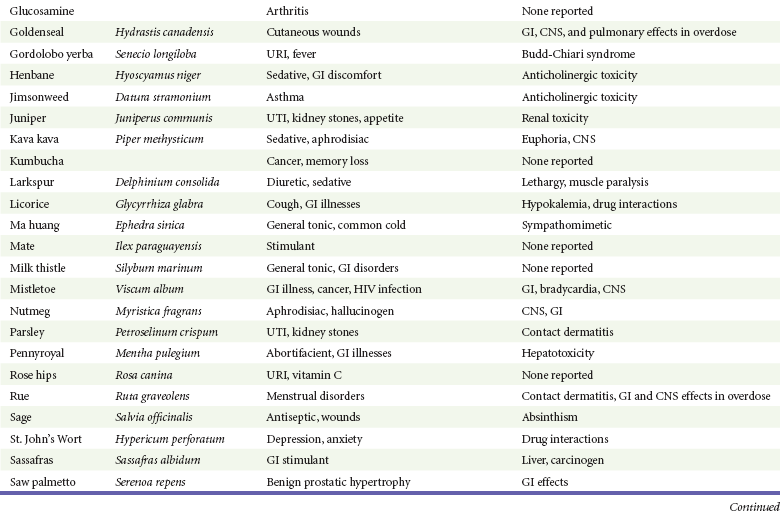
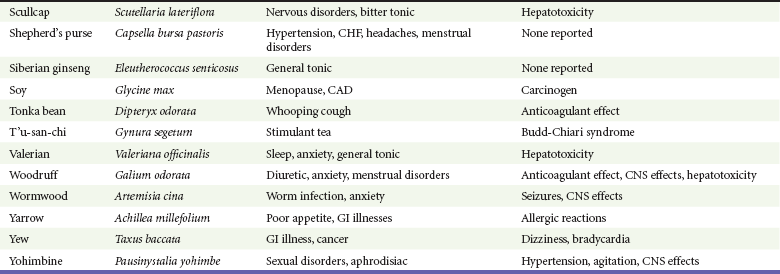
Chapter 164 Unintentional childhood exposure occurs most commonly with plants. Approximately 5% of all poison center calls involve plants. Of these, about 80% involve children younger than 5 years. Most of these cases involve household plants with a limited amount of plant material or toxin ingested, resulting in little or no toxicity.1,2 Identification of the botanical in question is most useful, but most patients and medical professionals do not have enough knowledge of botany or plant identification. The name of the plant or mushroom is often confusing because the scientific name is not typically known, and common names often overlap. Most emergency department personnel cannot identify common plants, such as mistletoe, holly berries, philodendron, and others. Several resources may be helpful, including plant atlases, CD-ROM plant databases, a local botanical expert, botanical garden personnel, or a poison center. Alternatively, a digital photograph of the plant or mushroom in question can be quickly e-mailed to a local expert to aid in identification.5 With herbal products, the product name or herbal plant may be known. Because of the limited Food and Drug Administration (FDA) regulation, however, the purported herb might have been harvested from the wrong plant or contaminated with other toxic material. Among more than 60,000 plant exposures reported to U.S. poison centers annually, most plant exposures occur in children (younger than 5 years) and involve household plants. Hospitalization for plant poisoning is rare, and fatalities occur in less than one in 10,000 exposures. Of thousands of different plant species, only a few are dangerously toxic.1,2,6 Following is a more detailed discussion of specific plants focusing on plants that are most poisonous or most commonly implicated in human exposures.1,6 Abrus precatorius (Fig. 164-1), known by several different common names (jequirity pea, rosary pea, prayer bean, Seminole bean, Indian bean, and crab’s eye), contains the toxin abrin, which affects protein synthesis, leading to cell death. The toxin is found in highest concentration in the seeds, which are used in jewelry or decoration. Because of their attractiveness, the seeds are often ingested by children. The hard, shiny coat causes most seeds to pass through the gastrointestinal tract without being digested. If the seeds are chewed or do not pass through the bowel rapidly and become digested, abrin is released, causing nausea, vomiting, and abdominal pain, which can be severe, and fluid and electrolyte balance is disturbed.7–11 Systemic absorption of the toxin is limited because the protein is enzymatically digested in the gastrointestinal tract. Rare parenteral exposure of small amounts is associated with severe toxicity and possible death. Treatment is supportive, with attention to fluid rehydration and electrolytes. Symptomatic patients should be given activated charcoal to absorb leaking abrin, and whole-bowel irrigation has not been studied but may help in moving numerous seeds more rapidly through the gastrointestinal tract. Capsicum annum includes many types of peppers (e.g., chili pepper, red pepper, bell pepper) and contains the active toxin capsaicin. This alkaloid releases and depletes selected nerve terminals of substance P, causing a severe local inflammatory response manifested by swelling, fluid exudation, and pain, which resolves rapidly as capsaicin depletes substance P. Capsaicin is not absorbed well through intact skin, but rarely symptoms can occur with prolonged and intense exposure.12 Ingestions often cause gastrointestinal symptoms, depending on the amount of toxin exposure. Most capsaicin exposures are from a pepper spray product, causing chemical conjunctivitis. Keratitis can occur and is assessed with fluorescein. Treatment consists of local irrigation and analgesics. Despite their often dramatic appearance, cases resolve rapidly during several hours without sequelae.13–15 Use of topical antacids may be effective for dermal exposures. Inhalation of capsaicin-containing powders is less common but can cause severe pulmonary exudation, potential acute respiratory distress syndrome, and death.16 Treatment is supportive, but extracorporeal membrane oxygenation has been used in children who have acute respiratory distress syndrome. Cicuta maculata (Fig. 164-2), commonly known as water hemlock, contains the potent neurotoxin cicutoxin.17 Deaths from water hemlock are among the most commonly reported plant fatalities in the United States. Water hemlock has small white flowers at the ends of umbrella-like stems. They resemble Daucus carota (Queen Anne’s lace) and Heracleum lanatum (cow parsnip). The mistaking of water hemlock for one of these edible plants is a common cause of exposure.18 Ingestion of any part of the plant can lead to nausea, vomiting, and abdominal cramping. Severe toxicity is manifested by seizures occurring within the first hour, which often are intractable and are a common cause of death. The toxic mechanism may be due to γ-aminobutyric acid (GABA) receptor antagonism. The ingestion is highly toxic and may be fatal. Seizures are common and are initially treated with benzodiazepines (i.e., lorazepam, 1-2 mg intravenously). If response is poor, treatment is as described for status epilepticus in Chapter 102. Because of the severe toxicity and lack of effective antidote, activated charcoal may be useful. Consultation with a regional poison center may be useful in individual cases. Conium maculatum (Fig. 164-3), or poison hemlock, was purported to be used in the execution of Socrates. It is mistaken for several edible plants, such as Daucus carota (Queen Anne’s lace), Foeniculum vulgare (sweet fennel), and Heracleum lanatum (cow parsnip).19 Poison hemlock contains the toxin coniine, which is similar to nicotine in structure and toxicity. The clinical picture and management resemble those of tobacco poisoning (see section on Nicotiana tabacum).20,21 Datura stramonium (jimsonweed) (Fig. 164-4) is one of numerous plants with alkaloids that have anticholinergic effects (see Chapter 150). The fruit is spiny and when opened contains 50 to 100 black seeds. All parts (including the seeds) contain the toxins atropine, hyoscyamine, and scopolamine, which are potent anticholinergic agents.22,23 One hundred seeds approximate 6 mg of atropine. Exposures are most commonly a result of abuse for hallucinogenic effects, usually by smoking of dried leaves or ingestion of the seeds.24–26 The clinical picture is that of the anticholinergic toxidrome.27,28 The symptoms can last for several days if the overdose is due to ingestion of seeds. It is unclear if activated charcoal and gastric emptying measures are effective at decreasing the course of toxicity and are not routinely recommended. Consultation with a regional poison center may be useful in individual cases.24 Treatment is as for anticholinergic poisoning29,30 (see Chapter 150). Dieffenbachia (Fig. 164-5) has more than 30 different common names, including dumb cane, mother-in-law’s tongue, dumb plant, and tuft root. Some of these names refer to the inability to talk that can occur after biting into parts of this plant. Typically, the mucous membranes of the mouth are affected immediately with severe pain, swelling, and the sensation of biting into glass. Most cases are limited to the mucous membranes of the oropharynx, but rare cases of airway compromise have been reported.31 The local effects are due to calcium oxalate crystals, packaged into bundles called raphides, that are found in cellular structures called idioblasts.32 These idioblasts also contain proteolytic enzymes that are ejected out of the idioblasts with the oxalate crystals when plant parts are chewed.33,34 Because of the immediate pain, further exposure typically is limited. Treatment is aimed at pain relief and local supportive measures, typified by feeding of ice cream to a symptomatic infant. Analgesics such as nonsteroidal anti-inflammatory drugs or opioids may be needed for pain. Epipremnum aureum is a common household plant also known as pothos ivy, devil’s ivy, hunter’s robe, and golden pothos. Toxicity is due to calcium oxalate crystals,6 the same toxin found in the Dieffenbachia, and the toxicity and treatment are similar. Eucalyptus plants have common names, such as the silver dollar, lemon-scented gum, cider gum, and blue gum. These plants are not toxic but are implicated in frequent plant exposures.35 The plants are used, however, to produce concentrated (approximately 70%) eucalyptus oil. Ingestion of small amounts (1-3 mL) has been reported to cause severe toxicity.36 The predominant symptoms are neurologic, including mental status alteration, headache, ataxia, and seizures. Treatment of severe toxicity is symptomatic supportive, except for seizures, which are treated as described in Chapter 102. Euphorbia pulcherrima (poinsettia) is a popular ornamental plant that is frequently implicated in plant exposures. It has a false reputation for being extremely poisonous. Ingestions are benign or cause minimal toxicity. However, contact dermatitis is relatively common with skin exposure and can be treated with steroids or antihistamines. Further discussion is found in Chapter 120. Nerium oleander (Fig. 164-6), or oleander, is one of many plants that contain toxic cardiac glycosides37,38 structurally similar to digoxin. Ingestion of several leaves is unlikely to cause serious symptoms.39,40 Large exposures from suicide attempts or misidentification of plants used for teas or herbal products can lead to severe toxicity or death. The cardiac glycosides are potent sodium-potassium–adenosine triphosphatase inhibitors, and the symptoms they cause are similar to those of digoxin poisoning (see Chapter 152). Measurement of an abnormal digoxin level is only qualitative proof of exposure because the serum digoxin test can falsely measure nondigoxin cardiac glycosides. Conversely, a normal digoxin measurement does not rule out exposure because the level of cardiac glycoside cross-reactivity varies. Treatment of dysrhythmias and hypotension includes multidose activated charcoal (50 g every 6 hours for 3 days) and digoxin-specific Fab antibodies (see Chapter 152).39–44 However, larger doses of Fab fragments generally are needed than for comparable digoxin poisonings. The initial empirical dose of digoxin-specific Fab fragments is 10 vials. If response to therapy is poor, repeated administration of an additional 10 vials is recommended. Nicotiana tabacum is widely grown in the southeastern United States as a source for cigarette and cigar tobacco. Several Nicotiana species contain nicotine as their major toxin, which activates and subsequently blocks acetylcholine receptors in the central nervous system (CNS) and peripheral autonomic nervous system. Most exposures are the ingestion of cigarettes or cigars by young children. Dermal exposure to workers harvesting plants and ingestion of wild plants mistaken for edible plants also have led to poisoning.45,46 The ingestion of one or two cigarettes has the potential to cause moderate poisoning in children, but most children ingesting cigarettes do not manifest toxicity. Patients without nausea and vomiting do not seem to progress to more severe toxicity.47 Dermal exposure in tobacco workers has been called green tobacco sickness.48 Nicotine is absorbed through the skin and occurs most severely when the skin or plant is wet. Exposure can be avoided by wearing of proper protective equipment. Symptoms begin shortly after absorption. Nausea, vomiting, salivation, lacrimation, diarrhea, hypertension, tachycardia, diaphoresis, agitation, and fasciculation are seen initially. More severe toxicity is manifested by seizures, respiratory depression (muscle weakness), and hyperthermia.49 Activated charcoal may be useful to limit absorption. Other treatments are supportive in nature because no specific antidote for nicotine is available. If seizures occur, initial treatment is with a benzodiazepine (i.e., lorazepam, 1-2 mg intravenously). If response is poor, treatment is as described for status epilepticus in Chapter 102. If severe salivation and lacrimation occur, atropine in 1-mg doses may be repeated until symptoms improve. Found in the eastern United States, Phytolacca americana (Fig. 164-7) is commonly known as pokeweed, poke, pokeberry, inkberry, scoke, American cancer, garget, phytolacca, and pigeonberry. Although the plant is poisonous, it can be detoxified by boiling it in water twice before use in salads or other recipes. Toxicity is seen when the plant is inadequately detoxified or raw parts of the plant are eaten.50 Symptoms begin shortly after ingestion and include severe nausea, vomiting, abdominal cramping, and diarrhea. Treatment is supportive. Rhododendron includes more than 1000 species of azaleas and rhododendrons, including mountain laurel, dwarf laurel, rose bay, western Labrador tea, and Japanese pieris. Numerous structurally related toxins (diterpene polyalcohols) have been identified from these plants, including grayanotoxin, rhodojaponin, asebotoxin, and others.51–53 These toxins bind to sodium channels and increase permeability (sodium channel openers), causing cardiovascular (e.g., bradycardia and hypotension) and gastrointestinal (e.g., nausea, vomiting, and abdominal pain) effects. Although ingestion of a few leaves is unlikely to cause symptoms, larger exposures can cause severe toxicity. In addition, these plant toxins can be concentrated in honey, so large honey ingestions, “mad honey,” can also lead to toxicity.52,54 However, no deaths have been reported. Treatment is supportive; atropine and cardiac pacing are used for bradycardia. For ventricular dysrhythmias, sodium channel–blocking agents, such as quinidine and procainamide, are used. However, limited efficacy data are available for these therapies. If response is poor, treatment with standard advanced cardiovascular life support (ACLS) protocol is warranted. Taxus (yew trees) (Fig. 164-8) have a hard seed surrounded by a fleshy red cup (the aril). The aril portion is not poisonous, and the seed has a hard coat that limits toxin release in the gastrointestinal tract so that most ingestions are nontoxic. If the seed is chewed or leaves are ingested, cardiac (e.g., bradycardia and hypotension) and gastrointestinal (e.g., nausea, vomiting, and abdominal pain) symptoms may occur. Deaths from this plant have been reported, usually in the setting of a suicide and secondary to cardiac manifestations. Bradycardia is treated with atropine. Wide-complex tachydysrhythmias are not responsive to sodium bicarbonate and should be treated per standard ACLS guidelines.55,56 Herbal products have gained an extraordinary amount of popularity in the past several decades. Although the highest use is among immigrants and patients with difficult-to-treat diseases, such as advanced cancer and acquired immunodeficiency syndrome (AIDS), these products are used by approximately 30% of the general population.57–59 Consumers often perceive herbals as more “natural” and thus “safer” and “harmless” despite many examples of toxicity associated with their use. This is coupled with medical practitioners’ having limited knowledge about herbal medications. In addition, herbals are widely marketed as safe and effective, especially on the Internet.60 One study of pregnant patients documented 45% herbal medicine use during some point of the pregnancy.61 Emergency department patients are also frequent users of herbal products.62–64 Herbal products are classified as dietary supplements and are not regulated as medications, even though they are used for their medicinal value.58,64,65 Regulation of dietary supplements is limited. Safety, quality, and efficacy for medicines are the responsibility of manufacturers. For herbal products used as dietary supplements, of which there are thousands to hundreds of thousands of potential products, the burden of proving efficacy and safety lies with the FDA.65–68 Studies looking at the efficacy of herbal products are limited, with few randomized, controlled studies. The National Institutes of Health sponsored several high-profile randomized placebo-controlled studies assessing the efficacy of several well-known herbals: St. John’s wort for depression, hawthorne extract for congestive heart failure, echinacea for the common cold, glucosamine–chondroitin sulfate for arthritis of the knee, saw palmetto for benign prostatic hypertrophy, and ginko biloba for dementia onset. Unfortunately, none of these trials has shown the herbal treatment to be effective.69–74 In addition, herbal manufacturers are not required to conduct efficacy studies. Studies evaluating side effects, drug interactions, and toxicity are even less available. Most herbal products have some direct pharmacologic action. The potency of these agents is usually limited, however. As a result, toxicity and side effects from the direct actions of herbal products are relatively uncommon.69–76 The lack of manufacturing quality control accounts for most toxicologic problems associated with their use. Four major types of toxicologic problems are associated with herbal product use: the misidentification of an herbal plant and toxicity resulting from a substituted plant, contamination with nonherbal toxic material, direct toxicity or overdose of the herbal product (Table 164-1), and drug-herbal interaction (Table 164-2).77
Plants, Mushrooms, and Herbal Medications
Perspective
Epidemiology
Unintentional Childhood Exposure
Botanical Identification
Plants
Abrus precatorius
Capsicum annum
Cicuta maculata
Conium maculatum
Datura stramonium
Dieffenbachia
Epipremnum aureum
Eucalyptus
Euphorbia pulcherrima
Nerium oleander
Nicotiana tabacum
Phytolacca americana
Rhododendron
Taxus
Herbal Medicines
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree