Physical Therapy
Physical therapy is used to preserve, enhance, or restore physical function and movement. The mainstays of this therapy include balance, endurance, stretching/range of motion, and strengthening. The goal is to alleviate current painful symptoms and prevent future pain. To accomplish this, the physical therapist acts as a motivator, challenger, and educator. Functional goals and targeted exercises are based on the patient’s specific complaints. Physical therapists use a number of exercises, as well as devices, in treating patients. Patients are taught proper form and technique in performing these exercises, which helps to facilitate maximal response. Along with alleviating pain, physical therapy has been shown to improve mood and quality of life. The techniques are often useful in combination with other forms of pain management including injection therapy, medication, and surgery.
Physical therapists emphasize lifestyle modification, because environmental factors can maintain and in some cases enhance pain. Lifestyle modifications include alteration in posture and improvement in body mechanics to minimize mechanical stress during daily activities. Nutritional guidance may also be appropriate.
Acute painful conditions can resolve during the set time the patient is working with the physical therapist. For chronic pain conditions, the patient will need to learn how to take an active role in self-care and transition to a structured home physical therapy program. In the current health care climate, patients are no longer seen as passive recipients of therapy. Patients are expected to take an active role in their well-being and to learn to perform their own physical therapy routine after being properly educated – much like insulin-dependent diabetics who learn how to check blood sugar, change their diet, and administer insulin after being taught the basics.
When to use
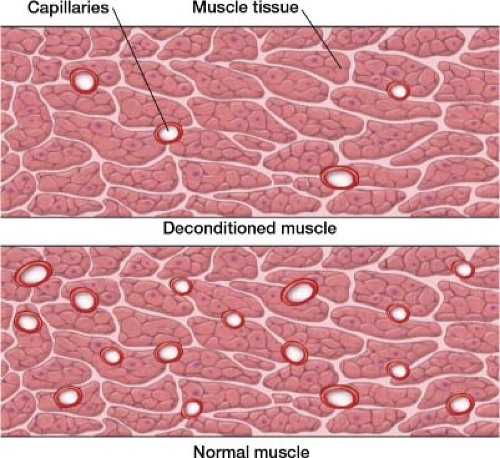
Chronic pain patients often try to protect the area that hurts by avoiding movement that exacerbates the pain. This in turn causes a negative series of events to occur that results in deconditioning: Muscle disuse, atrophy, and loss of contractile strength. Tendons and ligaments lose tensile and insertion strength as well as tissue elasticity. In the absence of movement and weight-bearing, there is minimal remodeling of tissue which is necessary to maintain proper integrity. Vital structures are then subject to rapid tearing, even with minor stresses. Physical therapy breaks this vicious cycle of deconditioning and pain.
Wolff law, developed by anatomist/surgeon Julius Wolff, states that bone in a healthy person will adapt to the loads to which it is exposed. Connective tissue and muscle responds to mechanical loading the same way bone does. This is why people lift weights to maintain and increase muscle strength. To remain healthy, muscle and connective tissue demands regular mechanical loading. Exercise is crucial to the health of articular cartilage because it ensures the passage of synovial fluid over articular surfaces. This critical movement of synovial fluid over cartilage provides nutrients and removes waste; otherwise, waste products build up and articular surfaces degenerate (Fig. 32-1). It is essential that the synovial lined load-bearing joints, of the spine, the hips and knees, receive appropriate filtration. Interestingly, the spine’s intervertebral discs are also heavily dependent on the same sort of movement. Lumbar spine movement facilitates
critical fluid exchange between the discs and their nutritional source, the interstitial fluid surrounding the spine. Joint stiffness and pain are caused by deterioration and inflammation of the lining of the synovial joints.
critical fluid exchange between the discs and their nutritional source, the interstitial fluid surrounding the spine. Joint stiffness and pain are caused by deterioration and inflammation of the lining of the synovial joints.
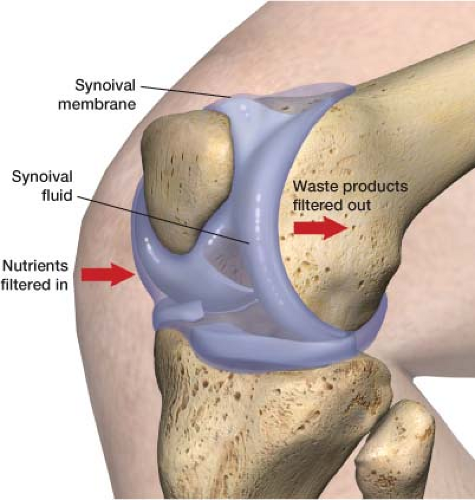 Figure 32-1 Synovial fluid filtering over cartilage tissue which provides nutrients and takes away waste products. |
Physical therapy is effective in returning patients to work and in decreasing sick time and medication use. It is especially important to start physical therapy quickly if a patient is too debilitated to work. Less than 50% of people who are disabled by their pain for more than 6 months ever return to work.1
How to use
During the initial consult, the physical therapist establishes a baseline of the patient’s pain and functional status. The patient and therapist then define endpoints and a time frame to achieve goals, for example, they may decide that at the end of the program the patient should be able to walk on the treadmill for 10 minutes and lift 15 lb from knee to chest eight times. The patient should reach these goals through a series of exercises that gradually increase in intensity.
Balance
Proper balance is often a problem for people with chronic painful conditions. It can lead to falls and difficulty walking. Balance exercises are crucial to many physical therapy routines. Patients may require a device to aid in balance, such as a four-prong cane. Instruction on proper use of the device is part of physical therapy.
Endurance
One of the mainstays of physical therapy is endurance, which improves the patient’s cardiovascular status. Working muscles may require energy faster than the body can deliver. This is especially true in deconditioned individuals, who have a decreased oxygen supply available to working tissue. The deprivation of oxygen leads to the early formation of lactate in muscles with use. In those cases, the working muscles generate energy anaerobically. When oxygen is limited, the body does not produce energy aerobically but proceeds to its next best option, temporarily converting pyruvate into a substance called lactate, allowing energy production to continue.
A side effect of high lactate levels is an increase in the acidity of the muscle cells, along with disruption of other metabolites, causing both pain and fatigue. This is one reason why patients have soreness when they start physical therapy. Endurance training increases capillary density, decreasing the diffusion distance from blood to muscles (Fig. 32-2). The positive change in the oxygen supply available allows for more efficient muscle dynamics with less production of lactic acid. Endurance exercises are key in becoming conditioned. If your patient is not keen on traditional physical therapy because they think it is too much, start with aqua therapy. I have had a number of patients decline physical therapy; starting it is just too much for them. When I suggest an alternative, aqua therapy – physical therapy in the pool, a number of patients are willing to try. These are often the patients who need it the most.
Stretching/Range of Motion
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree