CHAPTER 33 PERTINENT SURGICAL ANATOMY OF THE THORAX AND MEDIASTINUM
The thorax consists of the chest wall comprising the sternum, ribs, and thoracic vertebrae; the mediastinum containing the pericardium, heart, esophagus, trachea, great vessels, thoracic duct, and thymus; and the paired pleural cavities containing the lungs. This chapter will discuss the anatomy of these structures and spaces, as pertinent to trauma surgery and the surgical intensive care unit.
CHEST WALL
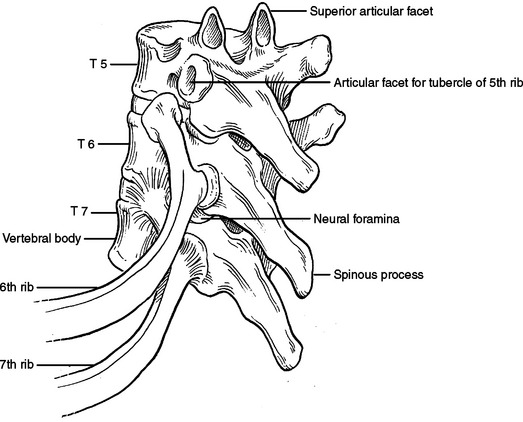
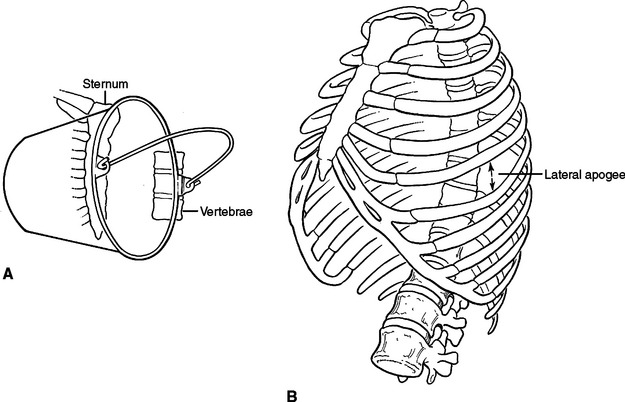
The bony structures of the chest wall include 12 ribs, 12 thoracic vertebrae, and the sternum. All ribs articulate posteriorly with the transverse processes and vertebral bodies of their respective thoracic vertebrae and the vertebral body directly superior (Figure 1). Ribs 1 through 7 are called true ribs because they articulate anteriorly directly with the sternum through their own costal cartilage. Ribs 8, 9, and 10 are called false ribs because they articulate anteriorly to the costal cartilage of the rib above. This creates a construct of stairstepping costal cartilages, which ultimately articulates with the sternum and creates the costal arch or costal margin. Ribs 11 and 12 are called floating ribs because they do not articulate with any structure anteriorly (Figure 2). Rather, they attach to the abdominal wall musculature, primarily the internal oblique muscle.
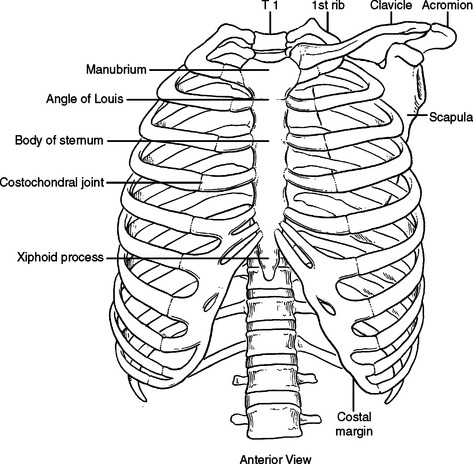
Figure 2 Bony chest wall. Anterior view.
(Redrawn from Grant’s Atlas of Anatomy, 11th ed., Philadelphia, Lippincott Williams & Wilkins, 2004, figure 1.8, p. 9.)
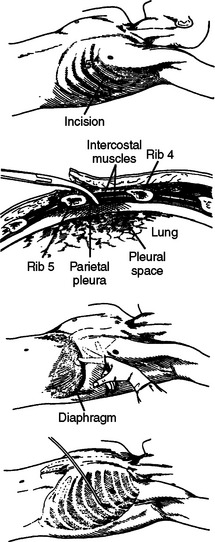
Because ribs 1 through 10 are fixed anteriorly and posteriorly, they function much like a bucket handle (Figure 3A). When performing a tube thoracostomy, as you approach the sternum anteriorly and the transverse processes posteriorly, the size of the interspace becomes fixed and narrow. Laterally, away from these points of attachment, the ribs separate and the interspace opens. The widest portion of the interspaces can be found at the lateral apogee or “keystone” of the rib. Tube thoracostomies placed laterally will be easier to place through the interspace and more comfortable for the patient (Figure 3B). Also, when creating a thoracotomy, division of the intercostal muscles far anterior and posterior will create a larger working space without tearing the intercostal muscle or fracturing a rib with placement of the rib spreader. The skin need only be divided over the working space, not over the entire intercostal incision.
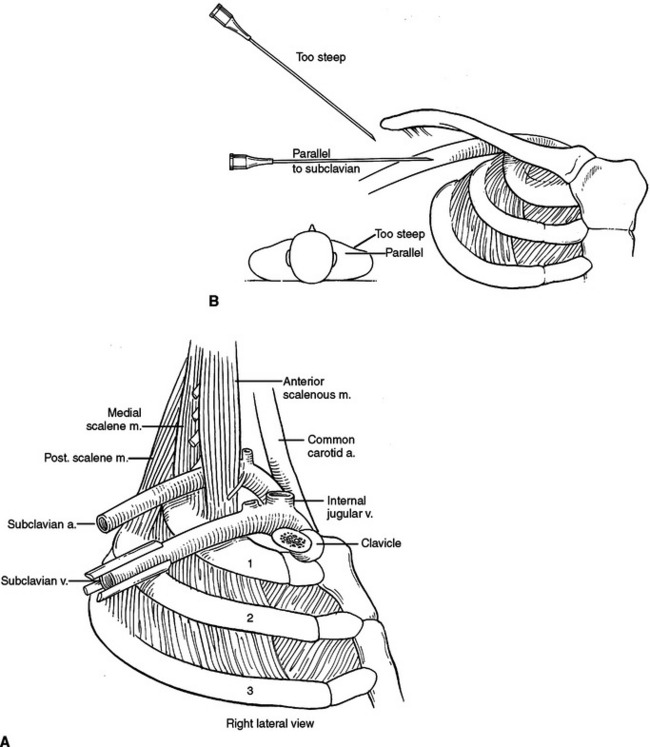
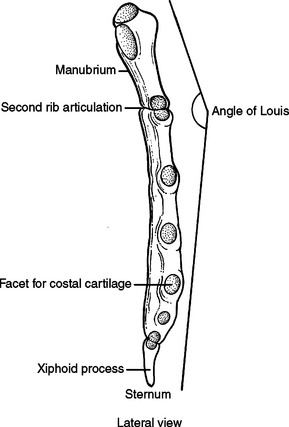
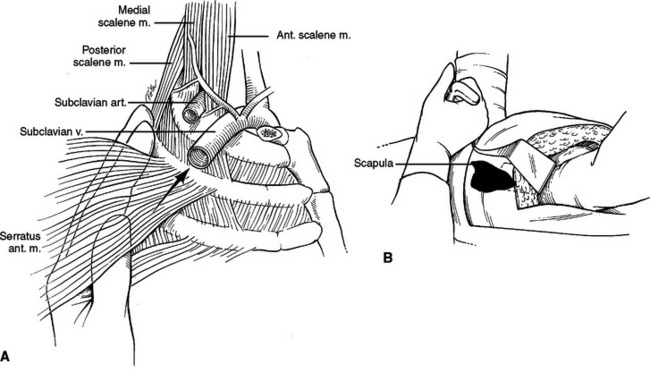
The sternum has three parts, the manubrium, the body, and the xiphoid process. The manubrium is thick and broad, articulating with the clavicle, first rib, and sharing the second rib articulation with the body of the sternum. The sternoclavicular articulation is the only bony articulation of the thorax to the shoulder girdle (see Figure 2). Understanding the angle of the clavicle, manubrium, and first rib is important in safe placement of central venous catheters into the subclavian vein. The subclavian vein and artery leave the arm and enter the thoracic inlet over the top of the first rib and under the clavicle. Once under the clavicle, a needle directed parallel to the clavicle and first rib will not enter the chest and cause a pneumothorax before finding the subclavian vein. A needle directed too steeply in its approach will quickly enter and exit the triangle where the subclavian vein is found, penetrate the intercostal space, and puncture the lung (Figure 4).
The second rib inserts into the sternomanubrial junction (angle of Louis). This can be easily palpated in most people as a horizontal ridge in the sternum or where the two planes that make up the sternum intersect (Figure 5). The interspace immediately below the angle of Louis is the second interspace. The angle of Louis serves as a landmark to rapidly locate the second rib and second interspace for placement of a catheter to decompress a tension pneumothorax or to place an anterior tube thoracostomy for an apical pneumothorax.
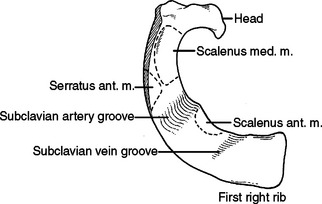
The first rib is short, broad, flat, and arches sharply from posterior to anterior (Figure 6). The second rib is longer than but very similar to the first rib (Figure 7). The first slip of the serratus anterior muscle attaches to the second rib approximately one-third of the arc from posterior to anterior—this slip also attaches to the inferior aspect of the first rib. Posterior to this attachment, the scalenus posterior attaches to the second rib.
When performing a thoracotomy, counting ribs can identify the correct interspace. Once the latissimus dorsi muscle has been divided and the serratus anterior muscle divided or swept anterior, the scapula is elevated. Thin fibrous attachments hold the undersurface of the scapula to the chest wall. A hand placed deep to the scapula, posterior near the spine, and apically can palpate ribs. The first rib is identified by its conspicuously broad and flat contour. Inferior to this, the second rib can be identified by the attachment of the scalenus posterior muscle. This muscle body is palpable by sweeping the finger from posterior to anterior along the second rib (Figure 8). Less distinct will be the third rib, which seems to “turn the corner” from the apex of the chest to the lateral chest wall (Figure 9). In a lateral decubitus position, the tip of the scapula overlies the sixth interspace. In a male, the nipple overlies the fourth interspace.
MUSCLES OF THE CHEST WALL
The paired pectoralis major muscles cover the majority of the anterior chest wall. The pectoralis major muscle originates from the clavicle and anterior aspects of ribs 1 through 6 inserting on the proximal humerus. Its origin from the chest wall is broad and an anterior thoracotomy will divide or separate its fibers. Inferiorly, the rectus abdominus muscle inserts onto the costal cartilages of ribs 5 through 7 and the xiphoid process. Lateral to this, the muscle fibers of the external oblique insert onto ribs 5 through 12. The external oblique muscle interdigitates with the serratus anterior muscle as it inserts on ribs 1 through 8 (Figure 10). Most thoracotomies do not traverse the interspaces guarded by the rectus abdominus and external oblique. These muscles will be encountered with thoracoabdominal incisions crossing the costal margin.
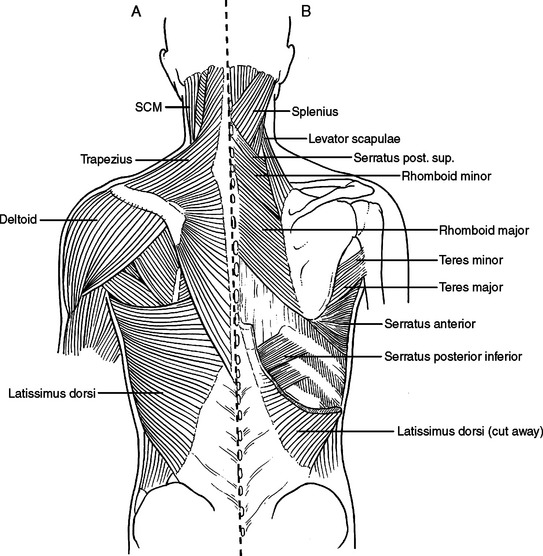
Laterally and posteriorly, two musculo-fascial layers guard the ribs. The more superficial layer contains the latissimus dorsi muscle laterally. Posteriorly, at the ausculatory triangle, or posterior border of the latissimus dorsi, this layer becomes a thin but tough layer of fascia, which more posteriorly envelopes the trapezius muscle. The second musculo-fascial layer contains the serratus anterior muscle laterally, becoming a broader sheet of thin but tough fibrous tissue posteriorly and then becoming the rhomboid major muscle then the rhomboid minor muscle posteriorly and superiorly (Figure 11). A tube thoracostomy will traverse these muscle layers to reach the ribs and interspaces. Knowing where you are in these layers allows precious time to be saved in traversing them and getting to where you need to be to complete the procedure.
A thoracotomy can be fashioned to divide or spare these muscles as needed in order to gain access to the rib cage. A full thoracotomy will divide the latissimus dorsi laterally and the trapezius posteriorly. The incision sweeps from horizontal across the lateral chest to vertical and parallel to the spine posteriorly (Figure 12). Deep to this layer, the serratus anterior can be swept anterior or divided. Posteriorly, the fascial layer coming off the serratus anterior is divided and then the rhomboid major and rhomboid minor muscles are divided. The innervation of the trapezius muscle and rhomboid muscles runs from medial to lateral. The more muscle body that is left medially, the more muscle function will be retained. Enough muscle needs to be left attached to the scapula to allow suture repair of the muscle, and the muscle should not be stripped from the scapula. The posterior and vertical aspect of this incision where the trapezius and rhomboids are divided is done to elevate the scapula off the chest wall, to access the interspaces underneath.
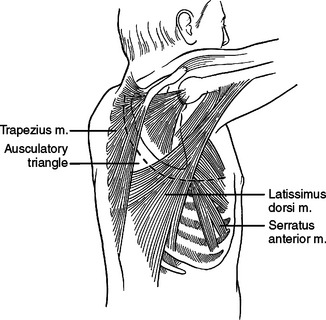
Figure 12 Full posterolateral thoracotomy.
(Redrawn from Grant’s Atlas of Anatomy, 11th ed., Philadelphia, Lippincott Williams & Wilkins, 2004, Figs. 4.47, 4.48, 6.13, pp. 233, 234, 367.)
INTERCOSTAL SPACE
Each intercostal space from superficial to deep, has two layers of muscle; an artery, a vein, and a nerve; and a diminutive inner layer of muscle. The external intercostal muscles run obliquely with fibers in the same orientation as the external oblique muscle of the abdomen (fingers in pockets). Deep are the internal intercostal muscles running in the opposite direction. The intercostal artery, vein, and nerve run along the inferior aspect of each rib, occasionally running underneath a ledge in the costal groove. To avoid injury to these three structures, tube thoracostomies and thoracotomies are directed over the superior aspect of each rib or through the middle of the interspace, but not the inferior aspect of the rib (Figure 13). The innermost intercostal muscles are located deep to the neurovascular bundle and run in the same direction as the internal intercostal muscles. While mentioned in anatomy texts, surgically, the innermost intercostal muscles do not need to be considered separately from the internal intercostal muscle (Figure 14). The intercostal arteries originate as segmental branches off the descending aorta. The intercostal space, including the underlying pleura, can be harvested as a posteriorly based pedicled muscle flap (Figure 15). This flap is useful for reinforcing bronchial or esophageal repairs.
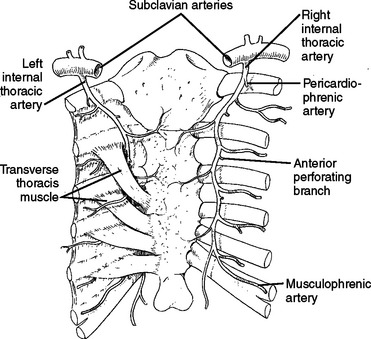
The internal mammary artery originates from the subclavian arteries bilaterally, and descends on the inside of the chest wall, approximately 1 cm lateral to the sternum bilaterally (Figure 16).
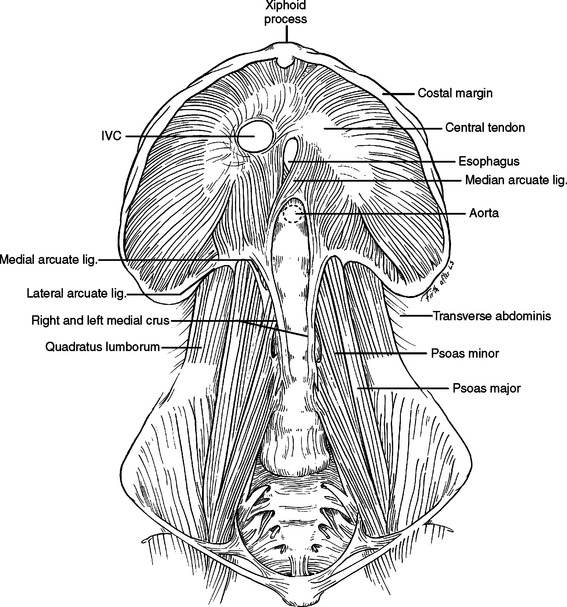
DIAPHRAGM
The diaphragm is the movable dome-shaped partition between the thoracic and abdominal cavities. With full exhalation, the dome of the diaphragm can rise to the level of the fourth interspace anteriorly (nipple level). With full inhalation, the diaphragm flattens, bringing the thoracic cavity down to the level of the costal margin anteriorly and the 12th rib posteriorly. The muscle fibers of the diaphragm originate from the sternum, the ribs, and the vertebral column. All three groups insert on a tough, fibrinous central tendon. Fibers of the sternal portion are short, arising as small slips from the back of the xiphoid process. Laterally on either side of the xiphoid, fibers originate from the inner surface of the lower six costal cartilages (costal margin). Posteriorly, fibers originate from a thick band arching over the quadratus lumborum (lateral arcuate ligament) and the psoas major (medial arcuate ligament). The paired lateral arcuate ligaments extend from the tip and lower margin of the 12th ribs and arch over the quadratus lumborum muscle to the transverse processes of L1. The paired medial arcuate ligaments complete the journey, arching over the psoas major from the tip of the transverse process of the first lumbar vertebrae to the tendinous portion of each diaphragmatic crus (Figure 17).
The posterior medial portion of the diaphragm is composed of two crura—an anatomic right crus originating from the upper three lumbar vertebral bodies and an anatomic left crus originating from the upper two lumbar vertebral bodies. Anterior to the aorta, the medial margins of the two crura form a poorly defined arch called the median arcuate ligament. Anterior to this arch, either the anatomic right crus (64%) or the anatomic left crus (2%) or both (34%) form the esophageal hiatus. While anatomists name the crura left or right by their origin from the left or right side of the vertebral bodies, surgeons name the crura left or right by their relationship to the esophagus. In the abdomen, visualization of the esophagus and division of the crus running to the left of the esophagus will expose the distal thoracic aorta above the level of the celiac artery and renal arteries. A clamp can be applied here to obtain vascular control. Alternatively, a retractor wrapped with a laparotomy pad can be used in this position to occlude the aorta by compressing it against the posteriorly located vertebral body (Figure 18).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree