68 Peripheral Arterial Disease
• Intermittent claudication is the earliest clinical manifestation of pathologically significant peripheral arterial disease.
• The ankle-brachial index can help confirm clinical suspicion of occlusive arterial disease.
• Ischemic rest pain signals critical, limb-threatening disease.
• The classic manifestation of acute arterial occlusion is described by the six “P’s”: pain, polar (cold), paresthesia, paralysis, pallor, and pulselessness.
• Treatment of nonischemic peripheral arterial disease consists of modification of risk factors, exercise programs, and medications aimed at platelet inhibition.
• Prompt initiation of therapy is the most important aspect of the treatment of acute limb ischemia, and patients should receive a heparin bolus followed by an infusion, ideally even before diagnostic testing is begun.
• Treatment of ischemic peripheral arterial disease depends on whether the extremity is viable (angiography to assess the extent of disease), nonviable (primary amputation), or threatened (immediate surgical intervention required).
Epidemiology
The most common term used to describe atherosclerotic vascular disease of the lower extremities is peripheral arterial disease (PAD). In North America and Europe, it is estimated that 27 million individuals are affected by PAD. In a significant proportion of patients the disease is occult but is nevertheless an important indicator of significant cardiovascular events.1,2 Systemic atherosclerotic disease with damage to end-organs other than the heart continues to be associated with high morbidity and mortality,3 and surprisingly little research is being done on it.
By 50 years of age the prevalence of PAD is 2% to 3%, and it rises to 20% in those older than 75 years.4 The clinical findings of PAD in patients older than 50 years is as follows: 10% to 35% have classic claudication, 20% to 50% are asymptomatic, 40% to 50% have atypical leg pain, and the remaining 1% to 2% have critical ischemia.5,6 Women have a relative risk of 0.7 in comparison with men. African American subjects have the highest risk for PAD (2.5) relative to the white population, followed by Hispanic subjects (1.5).
Box 68.1 lists the risk factors for PAD.6 They are similar to the risk factors that promote the development of coronary atherosclerosis. The risk factor with the highest correlation to PAD is cigarette smoking. When compared with nonsmokers, smokers have a 1.7- to 5.6-fold increase in the development and progression of atherosclerosis in the peripheral vasculature.7 In patients with symptomatic PAD, smoking increases this risk 8 to 10 times.8 Risk increases in a powerful dose-dependent manner according to the number of cigarettes smoked per day and the number of years of smoking. Diabetes increases the risk for PAD, 3.5 times in men and 8.6 times in women.9 Diabetic patients are also 7 to 15 times more likely to require amputation. The Framingham Heart Study found that risk for the development of intermittent claudication was 2.5-fold and 4-fold higher in men and women, respectively, who had hypertension and that this risk was proportional to the severity of the hypertension.9 Genetic predisposition represents an important risk factor for atherosclerosis, and such predisposition accounts for as much as 50% of the risk in some studies.10 Patients who have PAD also have a high incidence of coronary heart disease (CHD), and in general, patients have a two to four times higher incidence of CHD and cerebrovascular disease if PAD is also present.7
Box 68.1 Risk Factors for Lower Extremity Peripheral Arterial Disease
Age 50 to 69 years with a history of smoking or diabetes
Age younger than 50 years with diabetes and one other atherosclerotic risk factor (smoking, dyslipidemia, hypertension, or hyperhomocysteinemia)
Leg symptoms with exertion (suggestive of claudication) or ischemic rest pain
Abnormal lower extremity pulse findings
Known atherosclerotic coronary, carotid, or renal artery disease
Pathophysiology
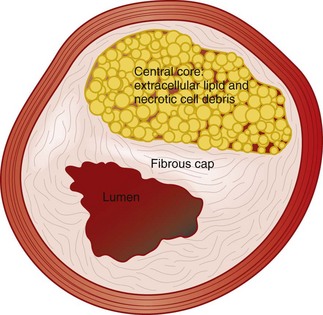
Atherosclerosis was originally thought to be primarily lipoprotein accumulation but is now better understood, fundamentally, as chronic inflammatory disease of the arterial system.11 The inflammatory process leads to plaque disruption and thrombosis, and the plaques that are vulnerable are characterized by a large lipid core, a thin fibrous cap, and inflammatory cells at the thinnest portion of the cap surface (Fig. 68.1).12 Plaque rupture has been shown to be critical in the development of acute coronary syndromes, but the importance of this event in patients with PAD is not known at this time.
The vascular smooth muscle cell is important in the development of atherosclerosis. Once activated, the cell migrates into the intima and begins to proliferate and secrete matrix proteins and enzymes. This step has been shown to be important in the development of stenosis both in the atherosclerotic vessel and in vessels that have been stented.13 In addition, the vessel often constricts rather than dilates, thereby narrowing the lumen even more.14 Progression of PAD can result from worsening local atherosclerotic disease or a superimposed embolic, thrombotic, inflammatory, traumatic, or vasospastic event.
Thromboembolism
More than 80% of arterial emboli originate in the heart and travel to the extremities, the lower extremities being much more frequently affected than the upper ones. Emboli typically lodge in places with acute narrowing of the artery, such as an atherosclerotic plaque or a point where the vessel branches. The frequencies with which emboli lodge in various areas are as follows15: femoral arteries, 28%; arm vessels, 20%; aortoiliac vessels, 18%; popliteal arteries, 17%; and visceral vessels, 9%.
Presenting Signs and Symptoms
The clinical signs and symptoms of PAD may be nonspecific and be manifested in a variable fashion according to degree and location of the atherosclerotic disease, as well as the presence of other previously described pathologic processes, such as thromboemboli, atheroemboli, inflammation, trauma, and vasospasm. The clinical spectrum ranges from a nonspecific systemic illness to a catastrophic event such as an ischemic leg. The gastrointestinal tract is an often-overlooked area of involvement that has been shown to be involved in about a fifth of cases. Patients may complain of nausea, vomiting, abdominal pain, melena, or hematochezia. Stools may be heme positive, and intestinal ischemia can progress to infarction in some cases. Skin manifestations are the most common finding in patients with PAD and appear in approximately a third of cases.16 Livedo reticularis is a red-blue netlike mottling of the skin and represents embolization to the skin. Such mottling is generally seen on the legs, buttocks, and thighs and rarely involves the arms.
Key components of the vascular review of symptoms and family history are listed in Box 68.2. Physical findings in patients with PAD are listed in Box 68.3. Despite general relationships between PAD and the site of pain, the history and physical examination are not reliable for the detection of lower extremity PAD. Relying solely on the presence of classic claudication will miss up to 90% of cases.5,6 Physical examination can also be unreliable. For instance, an abnormal femoral pulse has high specificity and positive predictive value but low sensitivity for large-vessel disease. The best single discriminator is an abnormal posterior tibial pulse.17
Box 68.2 Key Findings in the Vascular Review of Systems
Any exertional limitation of the lower extremity muscles or any history of walking impairment (fatigue, aching, numbness, or pain). The primary site or sites of discomfort in the buttock, thigh, calf, or foot should be recorded along with the relationship of such discomfort to rest or exertion
Any poorly healing or nonhealing wounds on the legs or feet
Any pain at rest localized to the lower part of the leg or foot and its association with the upright or recumbent positions
Postprandial abdominal pain that is reproducibly provoked by eating and is associated with weight loss
Box 68.3 Key Components of the Vascular Physical Examination in a Patient with Possible Peripheral Arterial Disease
Measurement of blood pressure in both arms and notation of any interarm asymmetry
Palpation of the carotid pulses and notation of carotid upstroke and amplitude and the presence of bruits
Auscultation of the abdomen and flank for bruits
Palpation of the abdomen and notation of the presence of aortic pulsation and the maximum diameter of the aorta
Palpation of pulses at the brachial, radial, ulnar, femoral, popliteal, dorsalis pedis, and posterior tibial sites
Auscultation of both femoral arteries for the presence of bruits
Assessment of pulse intensity, which should be recorded numerically as follows: 0, absent; 1, diminished; 2, normal; 3, bounding
Inspection of the feet for evaluation of color, temperature, and integrity of the skin and intertriginous areas and recording of the presence of ulceration
Documentation of the presence of symmetry, edema, and venous distention of the lower extremities
Recording of additional findings suggestive of severe peripheral arterial disease, including distal hair loss, trophic skin changes, and hypertrophic nails