
Penetrating Chest Trauma
Stephen J. Wolf
Although it is occasionally the result of mechanical accidents or impalements, penetrating trauma to the chest is often the result of interpersonal violence. Given the nature of the weapons encountered in the civilian population, injuries will typically be limited to tissues within the direct course of the penetrating implement. In military settings, penetrating trauma generally results in tissue injury as a result of transmitted compression waves or the formation of temporary cavities that are associated with higher-energy ballistics. These are all distinct from the shear injuries caused by acceleration–deceleration mechanisms and from the contusions and crush injuries resulting from forces dispersed about large contact areas, as seen in blunt thoracic trauma.
CLINICAL PRESENTATION
Pneumothorax
A common injury in penetrating thoracic trauma, pneumothorax is the collection of air in the potential space between the parietal and visceral pleura. The precise incidence varies across series and is largely dependent upon mechanism but has been reported to be significantly more common in penetrating trauma than blunt trauma (1). The clinical presentation depends on the patient’s overall condition as well any underlying illnesses. Although multiply injured patients or those with decreased mentation may not report cardiopulmonary symptoms, the typical presentation includes pleuritic chest pain, dyspnea, and air hunger. Physical examination may reveal tachypnea, tachycardia, and hypoxia, as well as the classic findings of decreased breath sounds and hyperresonance to percussion. Vital signs may deteriorate as the size of the pneumothorax increases. Simple pneumothoraces—confined collections of air within the pleural space—often result from direct injury to the pulmonary parenchyma and escape of air from bronchioles and alveoli. It has traditionally been thought that simple pneumothorax is likely to progress in the setting of positive-pressure ventilation, although the frequency of this occurrence has since been questioned. Open pneumothoraces result from an injury mechanism that creates a continued external communication to the pleural space. If the chest wall defect affords less resistance than the upper airways, air moves preferentially through the defect and gas exchange is impaired. Tension pneumothorax results from an expanding collection of intrapleural air. In the setting, increased intrathoracic pressures result in pulmonary collapse on the ipsilateral side first through direct pressure, then the contralateral side through mediastinal shifting. As a result tidal volume is compromised considerably. Ultimately, there is a significant decrease in venous return due to the compressive forces with resultant decreased cardiac output. Simple or open pneumothorax may progress to this grave clinical state if air continues to enter the pleural space from an external or bronchopulmonary source and is unable to escape. Clinical findings may include progressive tachypnea and tachycardia with hypotension and hypoxia. Physical examination may reveal jugular venous distention and absent breath sounds ipsilaterally. Tracheal deviation is a late finding and suggests impending cardiopulmonary collapse.
Tracheobronchial Injuries
Most tracheobronchial injuries occur superior to the thoracic inlet within the cervical trachea, where this structure is more superficial and in a relatively unprotected position. Although blunt trauma is a more common cause of tracheobronchial injuries, a penetrating mechanism is often associated with injury to other vital mediastinal structures (2). Pneumomediastinum is frequently seen and may be associated with pleuritic chest pain, dyspnea, or Hamman sign—a “crunching” sound on cardiac auscultation. Other concerning clinical presentations are hemoptysis or an air leak from a penetrating neck wound. Injury to a bronchus may lead to a bronchopulmonary fistula and pneumothorax. In this case, tube thoracostomy reveals a large air leak and may exacerbate respiratory distress because of an increased loss of inspired air (2). Concomitant disruption of a bronchus and a major vessel may result in venous air embolism.
Hemothorax
Hemothorax is a common finding in penetrating thoracic trauma and is often associated with pneumothorax. Direct injury to intercostal vessels, pulmonary parenchyma, mediastinal structures, great vessels, and the internal mammary artery are possible etiologies. The presentation is occasionally subtle, with no associated pneumothorax and minimal associated blood loss. More significant injuries result in respiratory distress and symptoms consistent with hemorrhagic shock or tension physiology, as up to 1.5 L of blood can accumulate in the hemithorax. Physical examination may reveal abnormal vital signs, dullness to percussion, and diminished breath sounds dependently. The presence of these findings has an excellent positive-predictive value for hemothorax in penetrating trauma, but physical examination has been demonstrated to be insensitive for this injury, and the absence of these findings does not exclude a clinically significant hemothorax (1).
Mediastinal Injuries
The mediastinum has a dense arrangement of critical structures, and penetrating trauma to this anatomic region can result in profound injury. The presentation may vary from only local physical complaints to full traumatic arrest. Penetrating mediastinal injury holds the potential for serious delayed complications.
Esophageal Injuries
The majority of penetrating injuries to the esophagus occur in the cervical region (see Chapter 27, Penetrating Neck Trauma). Thoracic esophageal injuries may present with subtle clinical findings yet can potentially progress rapidly to mediastinitis. The clinical presentation is often dominated by injuries to adjacent vital structures, but isolated esophageal injuries may produce odynophagia, dysphagia, and hematemesis. Progression to mediastinitis is associated with fever and worsening chest pain over time. Physical examination frequently reveals no specific findings of esophageal injury, but Hamman sign is classically described.
Cardiac Injuries
Penetrating wounds to the heart are commonly fatal. The majority of patients sustaining these injuries are hemodynamically unstable as a result of hemorrhage, cardiac tamponade, or a mixed pathophysiology. Up to 80% of cardiac stab wounds present with cardiac tamponade, but the majority of critical patients with cardiac gunshot wounds present in hemorrhagic shock (3). The specific location of the cardiac injury, as well as the presence or absence of associated injuries to the great vessels and pericardium, determines the course of the disease. Because of the position of the heart within the chest, the right side of the heart is most often injured (ventricle > atria), followed by the left-sided chambers (ventricle > atria). Major coronary arteries are also at risk for injury, presenting with regional electrocardiographic abnormalities, dysrhythmias, tamponade, or hemothorax. Cardiac injuries associated with defects in the pericardium that are small or effectively obstructed by epicardial fat or clot are more likely to progress to tamponade physiology, and injuries of the higher pressure chambers are associated with a more rapid progression to clinical instability. Hemorrhage of as little as 50 to 100 mL into the pericardium may result in decreased stroke volume and cardiac output. Tachycardia and hypotension are common in both hemorrhage and tamponade, but the patient with cardiac tamponade may demonstrate a pulsus paradoxus and jugular venous distention. A small proportion of patients may be hemodynamically stable at presentation, with only local symptoms and without evidence of cardiopulmonary compromise.
Great Vessel Injuries
Although only a minority of victims of penetrating thoracic trauma sustain injuries to the great vessels, up to 90% of injuries to the major thoracic vessels are the result of penetrating trauma (4). The associated mortality rate has been reported to be as high as 92%, with poorer outcomes associated with delayed recognition (5). In contrast to blunt mechanisms, most injuries are to the subclavian vessels, with associated mortality rates of 65% (4). Thoracic aortic injuries carry a high rate of associated vascular and nonvascular injuries. The clinical presentation depends on the degree of vascular disruption and the tissues supplied by the injured vessel, ranging from prehospital arrest to minimal local symptoms with a normal neurovascular examination.
Venous air embolism is an important complication of the disruption of any major vein that is in contact with a source of air. An example is a fistula between the pulmonary vein and a main bronchus. Valsalva or positive-pressure ventilation, may establish a pressure gradient that favors entry of air into the venous circulation, which then travels to the heart or more distal targets. In venous injuries other than those to the pulmonary vein, air emboli are confined to the right heart and pulmonary vascular bed in the absence of a preexisting right-to-left shunt. The presenting signs and symptoms may include hemoptysis, chest pain, evidence of end-organ ischemia (e.g., central nervous system deficits, myocardial ischemia), and cardiovascular collapse. Dramatic findings of “frothy” arterial blood gas samples and a machine-like murmur on auscultation have also been reported.
Diaphragmatic Injuries
Injury to the diaphragm must be considered in all thoracoabdominal gunshot wounds and in all stab wounds between the umbilicus and intermammary line anteriorly and up to the inferior tips of the scapulae posteriorly. Suspected injury to the diaphragm mandates consideration of both intra-abdominal and thoracic pathology. Contrary to previous teaching, recent reports suggest that diaphragmatic injury may be more common in penetrating rather than blunt trauma, with an incidence as high as 42% in patients with penetrating wounds to the left thoracoabdominal region (6). Concomitant injuries—cardiothoracic, intra-abdominal, neurologic, and musculoskeletal, in decreasing frequency—are the norm. Herniation of intra-abdominal structures into the thorax is a complication of diaphragmatic injury and may occur acutely, subacutely, or even years after an identifiable traumatic insult. This delayed presentation occurs because of the difficulties in diagnosing diaphragmatic injury, as well as the poor rate of healing of diaphragmatic defects because of the pressure gradient across this structure.
In an acute traumatic injury to the diaphragm, the clinical presentation is most often dictated by associated injuries to adjacent thoracoabdominal structures but may be associated with minimal symptoms. Referred shoulder pain may be reported, as well as respiratory distress from herniation of abdominal contents into the left hemithorax. There may be ausculatory findings of decreased breath sounds or borborygmi in the chest. A large herniation may result in a tension viscerothorax (shift of the mediastinum and hemodynamic collapse) and may be difficult to distinguish from tension pneumothorax.
The delayed presentation of diaphragmatic injury is associated with upper abdominal pain occasionally radiating to the shoulder. The signs and symptoms vary depending upon the segment of hollow viscus that has herniated. Classic signs and symptoms of bowel obstruction develop only with distal small bowel and colonic herniation. Delayed recognition and development of strangulation or incarceration is associated with significant morbidity and mortality.
DIFFERENTIAL DIAGNOSIS
The initial differential diagnosis in penetrating chest trauma is broad. Simple pneumothoraces are frequently detected; they are associated with local symptoms and may produce respiratory distress. Progression to tension pneumothorax is associated with worsening respiratory difficulty, hemodynamic instability, and the late finding of tracheal deviation. Findings of immobility of the chest wall, decreased breath sounds, and hyperresonance to percussion may aid in the diagnosis. Hemothorax, which often accompanies a pneumothorax, should be suspected when significant dullness to percussion is appreciated in the dependent portions of the thorax. Significant hemothorax can be associated with hemodynamic compromise and hemorrhagic shock.
Tracheobronchial injuries are most common with concomitant penetrating injuries to the neck or with missile trajectories that pass into the cervical region. Suspicion for this condition may be increased by findings consistent with pneumomediastinum (Hamman sign), hemoptysis, or a large persistent air leak after chest tube placement. Injuries to the mediastinal esophagus may also be associated with a “crunching” sound on cardiac auscultation but are likely to result in hematemesis or bloody output from suctioning of oral secretions or from a gastric tube.
Cardiac tamponade is classically associated with Beck triad of hypotension, jugular venous distention, and muffled heart sounds. Beck triad is present in less than half of patients with tamponade, however. Detection of pulsus paradoxus may contribute to a bedside evaluation for suspected tamponade, but it lacks sensitivity and specificity and may be present in a number of cardiopulmonary disorders. In the patient with hemodynamic instability and the possibility of a transmediastinal injury, however, hemopericardium and tamponade remain the diagnostic entities of greatest concern.
The emergency physician must consider injury to structures outside the confines of the thoracic cavity. The dome of the diaphragm extends superiorly to the nipple line, placing this structure, as well as intra-abdominal structures, at risk for injury from penetrating trauma. Injuries to the vertebral spine and associated neurologic injury must be considered (see Chapter 30). Finally, it must be emphasized that the trajectory of missiles is remarkably unpredictable; thoracic entry wounds may be associated with exit wounds in the abdomen, neck, and extremities.
ED EVALUATION
Physical Examination
Assessment begins with a primary survey of the airway, which is performed as continuous cardiac monitoring and pulse oximetry are instituted. Sinus tachycardia—although potentially secondary to pain—is a common and early finding in injuries causing hemodynamic compromise. The physician should direct attention to the thorax, noting chest wall asymmetry or the use of accessory muscles of respiration and listening for the presence and equality of breath sounds. Palpation of the chest wall may reveal crepitus, focal tenderness, or obvious instability. Thoracic wounds should not to be probed, as this is of uncertain diagnostic value and may cause further injury. Cardiac auscultation should be performed to discover muffled heart sounds or murmurs associated with direct cardiac injury. Jugular venous distention is an indicator of the elevated right-sided pressures seen in pericardial tamponade. Conversely, flat jugular veins are more consistent with hemorrhage and hypovolemia. A careful abdominal examination should also be performed, given the possibility of associated abdominal and diaphragmatic injuries. An extremity pulse deficit or focal neurologic deficits may indicate great vessel injury to the subclavian or common carotid arteries, respectively. Finally, there must be a thorough inspection to identify wounds to the thorax, abdomen, and extremities, as well as the axillae and gluteal cleft.
Unfortunately, physical examination is insensitive for hemo- and pneumothorax, and abdominal tenderness is reportedly lacking in a significant proportion of patients with documented diaphragmatic injury (1).
Chest Radiography
Chest radiography remains a critical tool in the evaluation of patients with penetrating thoracic trauma. An initial examination is most often performed anteroposteriorly (AP), at the bedside, in a supine or sitting patient. This examination may reveal large hemo- or pneumothorax and may provide information regarding missile trajectory by showing the location of a foreign body relative to external wounds (as indicated by radio-opaque markers). At least 200 mL of blood must be present for a hemothorax to be reliably detected on this examination, and small pneumothoraces are commonly missed. Larger pneumothoraces may be detected by a “deep sulcus sign” in the costophrenic angle (Fig. 32.1), but a normal study offers little reassurance because up to 67% of traumatic pneumothoraces are missed with this technique (7). A traditional posteroanterior (PA) film with an accompanying lateral view has a higher diagnostic yield; expiratory views may help in detection of small pneumothoraces. Traditionally, a negative initial chest radiograph was repeated after 6 hours to rule out the development of pneumothorax. However, literature now supports using a 3-hour repeat chest radiograph, or an immediate computed tomography (CT), to exclude occult injury (8). CT is recommended for select cases of significant diagnostic uncertainty (9).
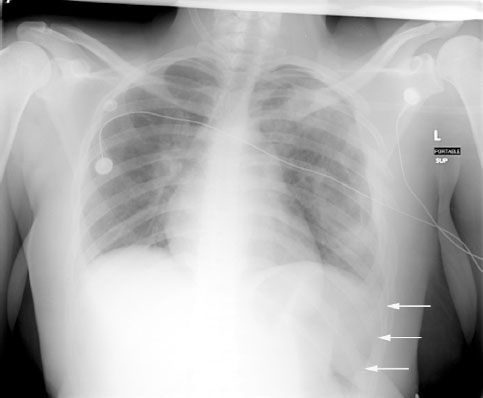
FIGURE 32.1 Chest radiograph. Portable, supine anteroposterior chest radiograph in a patient with thoracic trauma demonstrating a deep sulcus sign on the left. The relative lucency visualized over the left hemidiaphragm (indicated by white arrows) is suggestive of a pneumothorax. (Image courtesy of James F. Holmes, MD.)









