Chapter 20
Pelvic Fractures
Jameel Ali and Jeremie Larouche
Patients with pelvic fractures may have major hemorrhage from the fracture itself or from other major injuries and will often require care in the ICU at some point. Management of the hemodynamic, cardiopulmonary, coagulation, metabolic, acid–base and hypothermic derangements that frequently occur in such patients are discussed elsewhere in this textbook. Understanding issues specific to the pelvic fracture is crucial to optimize management of these patients. In this chapter, we discuss the clinical presentation, diagnosis, classification and principles of management that will guide the intensivist in caring for these patients.
Initial assessment of mechanical stability, as well as the application of a pelvic binder in hemodynamically compromised patients is a crucial first step in managing individuals with a pelvic fracture. For those injuries associated with ongoing hemodynamic compromise, clinicians must differentiate arterial from venous hemorrhage and urgently determine in consultation with the appropriate specialist whether the patient would benefit most from arterial embolization or retroperitoneal packing. Definitive management often involves both internal and external fixation options, the timing and priority of which requires consultation with the orthopedic surgeon.
Introduction
The care of pelvic fractures has evolved significantly over the last 50 years. As highlighted by Flint and Cryer,1 the recognition of retroperitoneal bleeding associated with pelvic fractures as well as the difficulties in controlling it have lead to vastly different approaches. Initial enthusiasm for exploration of the hematoma and attempts at direct control of the source of bleeding quickly lost popularity as surgeons realized that there was often no discreet bleeding vessel and decompression of the hematoma too often resulted in exsanguination of the patient.2 Instead, four major therapeutic modalities have evolved in the management of acute pelvic fractures. Various commercial and improvised pelvic binders, minimally invasive surgery via external fixators or percutaneous screw fixation, the use of Transcatheter Arterial Embolization (TAE), and retroperitoneal pelvic packing.
Despite these advances, there is no universally accepted algorithm in the management of the hemodynamically compromised patient with a pelvic fracture. A review of the literature reveals very contrasting practices by different institutions, with certain regional preferences. Regardless of the algorithm used, the challenge lies in adequately resuscitating the patient while identifying and controlling the hemorrhage. Three possible sources of bleeding exist3: (1) venous, from tearing or puncturing of pre-sacral venous plexuses, (2) from the cancellous surface of bone, and (3) arterial, from disruption of the anterior or posterior trunk of the internal iliac arteries or their branches. Patients may often have multiple sources of hemorrhage occurring simultaneously. Tamponade can normally be achieved in low pressure venous bleeding but it is not as effective in significant arterial bleeding. Conversely, non-specific embolization of supplying arteries does not decrease venous blood loss, and carries significant complications.4 It is therefore imperative that physicians who are managing these severely injured patients collaborate as part of a multidisciplinary team, and consider each patient individually.
Classification
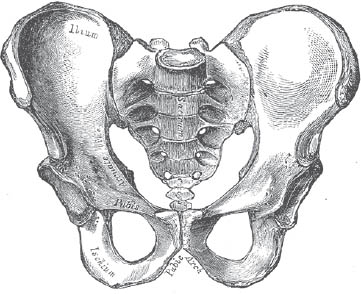
The pelvic ring is formed by three components: the left ilium, the right ilium, and the sacrum (Fig. 1). These are joined posteriorly by the left and right sacroiliac ligaments and anteriorly at the pubis symphysis. The sacrospinous and sacrotuberous ligaments, as well as the pelvic floor musculature provide further stability. Disruption at any one particular aspect of the ring usually leads to failure at a second point, and clinicians should be weary of diagnosing isolated pelvic ring injuries.
Injuries to the pelvic ring are normally classified according to one of two systems: the Young–Burgess classification (Table 1), or the Tile classification (Table 2). Both are based on the information available by physical examination and plain radiographs. While both of these classification systems are widely used, studies have historically demonstrated very little inter- or intraobserver reliability.5 It is also important to note that fracture classification has little predictive ability to determine which patients are at risk of significant hemorrhage.1,6 Physicians should therefore take into account not only the X-ray appearance of the fracture, but also the mechanism of injury and the patient’s physiologic status.
Fig. 1. Drawings of pelvic osseous anatomy.
Table 1. Tile classification of pelvic ring fractures.
Type A: Pelvic ring is stable | |
A1 | Fractures not involving the ring (avulsions, iliac crest or wing fractures) |
A2 | Stable, minimally displaced fractures of the pelvic ring |
Type B: Pelvic ring is rotationally unstable, but vertically stable | |
B1 | Open book |
B2 | Lateral compression injury |
B2-1 | Anterior ring displacement through ipsilateral rami |
B2–2 | Anterior ring displacement through contralateral rami |
B3 | Anterior ring injury to bilateral rami |
Type C: Pelvic ring is both rotationally and vertically unstable | |
C1 | Unilateral |
C1-1 | Posterior ring injury is iliac fracture |
C1-2 | Posterior ring injury is through sacroiliac fracture/dislocation |
C1-3 | Posterior ring injury is through sacral fracture |
C2 | Bilateral pelvic injury with one type B and one type C |
C2 | Bilateral pelvic injury with both sides type C |
The Young–Burgess classification focuses on the vector of force at the time of injury, and the resultant bony displacement. This force is divided into three categories: anterior to posterior compression that can result in “open book” injuries, lateral compression injuries with fractures through the ilium or the sacrum, and lastly vertical shear injuries in which one hemi-pelvis becomes detached from the remaining skeleton (Table 2).
Table 2. Young–Burgess classification of pelvic fractures.
Epidemiology
There is an estimated incidence of 23 pelvic fractures per 100,000 persons per year in the USA.5 Of these, approximately half are low energy, with a propensity to occur in geriatric patients with low bone mineral density. Reported mortality for these patients is <1%.1 The other half occurs in younger patients in the setting of a high-energy trauma, and is associated with a higher injury severity score, a higher propensity for massive hemorrhage, and a mortality rate ranging from 19–50%.2,5
In their series of 174 patients with unstable pelvic ring injuries, O’Sullivan et al.6 have demonstrated an association between mortality and an Injury Severity Score >25, a Triage-Revised Trauma Score less than 8, age over 65, systolic blood pressure <100 mmHg, a GCS <8, and a requirement for more than 10 units of blood in the first 24 hours. Morphology of the fracture was not predictive of mortality.
Physical Exam
All trauma patients should initially undergo a complete and thorough assessment according to the latest Advanced Trauma Life Support (ATLS) guidelines. Between 60–80% of patients with a pelvic ring injury will possess another musculoskeletal injury, and 8% will possess a lumbosacral plexus injury.5 Assessment of pelvic injuries is a critical part of determining the source of hemorrhage in any hemodynamically compromised patient. It has been estimated that the retroperitoneum can accommodate up to 4L of blood prior to physiological tamponade of venous bleeding.2 If there is significant disruption of the retroperitoneal muscle compartment, or if arterial bleeding exists, the patient may completely exsanguinate in the absence of acute intervention.
Assessment of pelvic stability
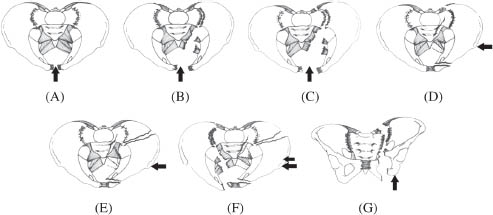
Determination of pelvic stability is required as part of the initial assessment of a polytraumatized patient. This should be done only once and performed gently to minimize pain and the disturbance of any clot that may have formed. It should be carried out by the most experienced physician available. It is performed by first having the examiner’s thumbs placed over the anterior superior iliac spines of the patient, which are to be used as a reference point. The palms of the examiner then come to rest on the anterior inferior iliac spines, and from there, both a distraction and compression force may be applied (Fig. 2). Any movement of one hemi-pelvis compared to the contralateral side constitutes a positive examination. Fluoroscopy, if available in the trauma bay, may be a useful adjunct in this examination.
Application of Pelvic Binder
Any pelvis that is deemed to be mechanically unstable should have a pelvic binder applied immediately. While many physicians are concerned about the theoretical risk of inappropriately applying a binder to a lateral compression-type fracture and “over-reducing” the fragments, this must be weight against the possibility of not reducing a fracture that may directly affect the patients chance of survival. We therefore recommend the immediate application of a pelvic binder to any pelvis fracture that is mechanically unstable, which should be followed up with an anterior–posterior radiograph of the pelvis when possible to judge the quality of the reduction.
Fig. 2. Picture of how to assess for pelvic stability.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree