Chapter 15 Pediatric Vascular Access and Centeses
Intraosseous Infusion
IO infusion was first described in 1922 and became widely used in the 1930s and 1940s.1 With the development of disposable needles and catheters, use of IO infusion fell out of favor. It was not commonly used again until the mid-1980s, when a series of publications demonstrated the utility of the technique for rapid venous access in critically ill children.2,3
Indications
IO infusion is indicated in situations requiring the rapid acquisition of intravenous (IV) access in which the establishment of conventional peripheral access is difficult or impossible. The situations in which it is most often used include cardiopulmonary arrest, shock, burns, and status epilepticus. In these situations, one or two attempts at standard peripheral access are usually made prior to placing an IO needle. In cardiopulmonary arrest, one should immediately gain vascular access via the IO procedure. In addition to its use in the hospital, IO access has been successful in the prehospital setting as well as in critical care transport.4,5
The success rate with the technique is high, greater than 95% with experienced practitioners.6 Equal success using the new mechanical intraosseous devices has also been demonstrated.7 Most fluids and medications that can be given through a conventional IV line can be given via an IO infusion with comparable results. In the event of cardiac arrest or severe shock, IO access is at least as effective as peripheral venous access in providing fluids and medications to the central circulation. Studies have shown that commonly used resuscitation, antiepileptic, and antibiotic drugs all can be given effectively through an IO line. Three antibiotics produce subtherapeutic levels when given via an intraosseus line at standard IV doses: chloramphenicol, vancomycin, and tobramycin.8
In addition to the administration of fluids and medications, IO access can be used for certain clinical laboratory studies. No significant differences were found when comparing electrolytes, chemistries, pH, PCO2, or hemoglobin from IO marrow specimen with either arterial or venous blood samples.9 A marrow specimen can be cultured in lieu of a blood culture.10 Finally, the marrow can be used for blood type and crossmatching.
Contraindications
IO infusion has few absolute contraindications. A fractured or previously punctured bone should not be used because infused fluid will extravasate and possibly cause compartment syndrome. Alternate sites in other bones can be used in such situations. Bone diseases such as osteogenesis imperfecta and osteopetrosis have been suggested as contraindications to intraosseous infusion,11 but a case of successful IO access in a patient with osteogenesis imperfecta has been reported.6 Placing the needle into an area of cellulitis or burn could cause osteomyelitis or other infectious complications and is a relative contraindication although if limited sites are available, placing the IO needle through burned skin is acceptable.
Supplies and Equipment
Access to the bone marrow space is accomplished with one of several different types of needles. Conventional bone marrow needles (e.g., Jamshidi needle, CareFusion, San Diego, Calif.) work well. Needles made specifically for IO infusion use are available, including a straight needle or a needle with a threaded screw device (e.g., Sur-Fast, Cook Medical, Bloomington, Ind.). Usually a 15- or 18-gauge needle is chosen. The smaller 18-gauge should be used in infants. Studies have shown no significant differences in time required to insert the needle, success rate, or extravasation rates between standard and threaded IO needles.12,13 If bone marrow or IO needles are not available, standard lumbar puncture needles can be used,6,14 although they are prone to bend. In neonates, even a 19- or 21-gauge butterfly needle can be used.14 Needles with a stylet are preferred to prevent clogging of the needle by bone.
Two new mechanical devices appropriate for the pediatric population have been introduced: the Bone Injection Gun (B.I.G., Waismed Ltd., Herzliya, Israel) and the EZ-IO (Vidacare Corporation, San Antonio, Tex; see Figures 15-1 and 15-2). The B.I.G. is a spring-loaded device, while the EZ-IO is a small battery-powered drill; both of these penetrate the bone marrow more quickly as compared to the manual method.
Technique
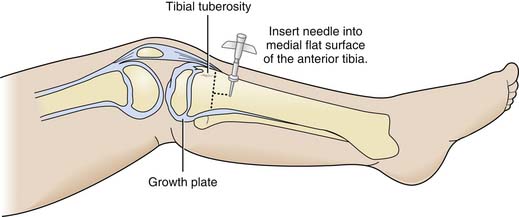
The IO needle can be placed into the bone marrow at one of several sites, including the proximal tibia, distal femur, distal tibia, iliac crest, and sternum. The proximal tibia is the site most commonly chosen. The sternum has been used in adults but should be avoided in children because of the possibility of perforating the smaller chest cavity.15 In addition, placing the needle in the sternum can interfere with airway and circulatory resuscitative efforts. When the needle is placed in the proximal tibia, the insertion site is located by palpation on the flat anterior tibial surface 1 to 3 cm (two fingers breadth) distal to the tibial tuberosity (Figure 15-3). This site is chosen to avoid the proximal growth plate. The midshaft should not be used because of increased risk for fracture. Placing a towel or sandbag under the child’s leg helps stabilize the leg and makes insertion easier. The skin overlying the area should be prepped with antiseptic solution. Because IO lines are usually placed in obtunded patients, local anesthetic is not always necessary. Local anesthesia by infiltration with 1% lidocaine can be performed if the patient is awake. If a needle with a plastic sheath is being used, adjust the sheath so that an adequate length of needle protrudes beyond the sheath. Some authors have suggested inserting the needle at a 60- to 75-degree angle away from the tibial growth plate, but others recommend using a perpendicular or 90-degree angle. The perpendicular angle helps prevent the needle from sliding along the bone. The needle is advanced using firm pressure and a twisting or rotary motion until a “give” or loss of resistance is felt, indicating entry into the marrow space. The force needed to penetrate the bony cortex is considerable; the twisting motion helps significantly in needle insertion. One disadvantage of using a threaded needle is that the “give” or loss of resistance that occurs when the needle enters the marrow space may not be felt; however, the needle may be more secure in the bone once the needle is placed.25 The stylet is removed and a syringe is attached to the needle to attempt to aspirate marrow. Correct placement of the needle should be confirmed to avoid extravasation. Aspiration of bloody fluid into the syringe confirms that the needle is correctly placed. Additional evidence of correct needle placement includes the observation that the needle stands upright in the bone without support and lack of resistance when flush solution is infused into the needle with the syringe. Sometimes, marrow cannot be aspirated even if the needle is correctly placed. If the “give” is felt on insertion and the needle stands alone in the bone but marrow cannot be aspirated, infusion of a small amount of fluid with the syringe can be attempted. Fluid should infuse easily with little pressure and without noticeable swelling of the soft tissues or extravasation of fluid.
In small studies, placement of IO needles with the new mechanical devices have success rates equal to or higher than traditional manual methods, with the added benefit of easy use and less risk to the user.7 However, the high cost of this equipment may be a major limitation for use. In children, prehospital providers preferred the IO drill over the spring-loaded injection gun.16,17
Maintenance
Once correct placement of the needle is confirmed, fluids and medication can be administered with a syringe via a stopcock or T-connector, or a standard IV infusion set can be connected to the needle. The needle is secured using gauze pads and tape. Some have suggested taping a clear plastic cup over the needle to help prevent dislodgment.6 The site should be observed carefully visually and by palpation for signs of extravasation, both immediately after placement and frequently (every 5 to 10 minutes) during use. If evidence of extravasation is seen, the needle should be removed to avoid compartment syndrome. If needle placement is attempted at one site and the cortex is penetrated but the line cannot be used because of extravasation, another bone must be chosen for subsequent attempts.
IO access is intended only for short-term use in emergency resuscitative situations; long-term use increases the risk of extravasation, compartment syndrome, and infection.38,43 Therefore, once IO access is secured, efforts should be directed toward obtaining conventional IV access. Once alternate access is obtained, the IO needle should be removed, manual pressure applied for 5 minutes, and a dressing applied to the site.
Complications
Significant complications of IO infusion are rare. The most common complication is extravasation of fluid. The causes of extravasation include incomplete penetration of the bony cortex, movement of the needle such that the hole is larger than the needle, dislodgment of the needle, penetration of the posterior cortex, and leakage of fluid through another hole in the bone, such as a previous IO site or fracture. Extravasation of a small amount of fluid is usually not problematic, but compartment syndrome may result after extravasation.18 One report documented a compartment syndrome after infusion of only 35 mL of fluid via the IO line.19 Use of the IO line for prolonged periods and use of the IO line with pressure infusion appear to be risk factors for compartment syndrome. Compartment syndrome associated with IO infusion can result in the need for fasciotomy and amputation. Careful frequent observation of the IO site is necessary to detect extravasation and to prevent compartment syndrome. If extravasation occurs, the needle should be removed and the extremity observed for signs of compartment syndrome. Initial experience suggests the complications of the new mechanical devices are similar to the traditional IO needle.
Other rare complications include infection and bone fracture. Osteomyelitis, cellulitis, and sepsis have been reported in conjunction with IO infusion.20 Risk for infection is increased when IO access is used in a bacteremic patient and when the line is used for a prolonged period. The risk of osteomyelitis is low. Although IO access is usually obtained in emergency situations, precautions to prevent infection should be taken, including use of sterile gloves and equipment and preparation of the skin with antiseptic solution (iodine or alcohol). Fracture of the bone has been reported.21 One report of fracture associated with IO infusion is the case of a 3-month-old in whom a 15-gauge needle was used; a smaller needle size (18-gauge) should be used in small infants.
There are some theoretical complications that are probably not significant in clinical practice. Fat embolism occurs with infusion into the bone marrow space. An animal study found fat emboli in the lung with IO infusion, but no changes were seen in oxygen saturation or intrapulmonary shunt.35 There are no reports of clinical fat embolization associated with IO infusion in humans in the English literature. However, intravascular air was discovered on postmortem studies in two patients.22 Because of the risk of fat embolization, children with a right-to-left shunt may be at increased risk for cerebral emboli with IO infusion.6
The physical effects of infusion on the growing bone seem to be self-limited. Both animal studies and human follow-up studies of the bone and bone marrow show only short-term, minor changes and no long-term changes in bone structure, growth, or bone marrow.23,24
Arterial Catheter Placement
Indications
Indications for an arterial catheter include the following:
Contraindications
A catheter should not be placed in an extremity with compromised perfusion. Evidence of adequate collateral circulation is desirable prior to placement of an arterial catheter. The traditional means of assessing collateral circulation to the hand is the Allen test. The radial and ulnar arteries are compressed until the distal extremity is blanched. Pressure over one artery then is released. Capillary refill should return to the distal extremity in less than 5 seconds. The test then is repeated by unblocking the other contributing artery after the distal extremity becomes blanched. Some practitioners question the utility of the Allen test because a normal test result does not guarantee adequate collateral circulation, nor does an abnormal test necessarily indicate possible complications.25 The Allen test is considered less reliable for patients in shock. Additionally, an arterial catheter is often placed without assessing collateral circulation in emergent circumstances.
Procedure
Box 15-1 lists the supplies and equipment required for arterial catheterization.
Technique
Catheters also can be placed in the axillary or femoral arteries if no peripheral sites are suitable. Insertion of a catheter into the axillary artery is technically more difficult than the other sites mentioned and is associated with a risk of brachial plexus injury due to hematoma compressing the neurovascular bundle.26 Traditionally, many physicians have been reluctant to place arterial catheters for long-term use into the femoral artery, particularly in infants and young children, for fear of complications, most notably severe ischemia of the limb. A recent review of 745 femoral artery catheterizations in critically ill pediatric burn patients revealed a 1.1% rate of loss of distal pulse. In this retrospective study, limb ischemia was associated with younger age, smaller patient size, and increased severity of the burn injury. Patients who suffered limb ischemia were managed, for the most part, with immediate catheter removal and systemic heparinization. Three underwent thrombectomy. All patients in this series showed complete recovery of limb perfusion, except for one who required amputation of the fifth toe on the ipsilateral side.
Traditional teaching has held that the brachial arteries should not be used for arterial catheters because of the lack of collateral blood flow and risk of distal extremity ischemia. In a review of arterial catheter placements performed at a pediatric cardiac surgical center, the authors reported on the use of 386 brachial artery catheters in infants weighing 20 kg or less. None of these catheterizations were reportedly associated with permanent ischemic damage, and only three were associated with what was described as temporary loss of distal perfusion.28 Despite these encouraging results, the complete lack of collateral circulation at the brachial artery requires careful consideration of risks and benefits before placement of a brachial artery catheter. Additionally, the superficial temporal arteries also should not be used because of poor collateral flow as well as the fact that retrograde flow from a catheter placed in this artery could result in showering of emboli into the cerebral circulation.
The selected site must be properly immobilized prior to placement of the indwelling catheter. If placing a radial artery catheter, the wrist is hyperextended 30 degrees to develop a straighter course and to bring the radial artery into a more superficial position. Typically, the radial pulse can best be palpated and catheter insertion should first be attempted in a position just proximal to the proximal crease, or usually about 1 to 2 cm from the wrist. Recently, the technique for placement of a radial arterial catheter has been expertly summarized in the “Videos in Clinical Medicine” series in the New England Journal of Medicine.29 The following discussion of insertion technique can be applied to catheter placement at any of the sites discussed above. First, the site is prepared with a chlorhexidine solution and draped with sterile towels. Lidocaine (1% without epinephrine) is infiltrated locally. Alternatively, lidocaine/prilocaine (EMLA) cream can be used as a local anesthetic. Systemic narcotics and/or anxiolytics can be administered as well, although they should be used cautiously in a patient who is not being ventilated. Percutaneous placement of the catheter can be accomplished using one of several techniques. The first method uses a catheter over a needle, very similar to placement of a peripheral IV catheter. The needle is inserted through the skin at a 30-degree angle (bevel up or down). When a flashback of blood is obtained in the hub, the catheter is advanced another 1 to 2 mm. While holding the needle stable, the catheter is advanced over the needle into the lumen of the vessel. Blood should be flowing continuously into the catheter hub prior to attempting to advance the catheter. Once the catheter is inserted through the skin to the hub, a flushed Luer-Lok connector is attached to the hub while pressure is applied over the cannulated artery. Correct placement of the catheter is verified by aspirating arterial blood into a syringe attached to the connector. The catheter is then flushed and securely sutured or taped into position. A transparent dressing is placed over the catheter as a protective barrier. Before the final dressing is placed, many centers use a chlorhexidine-impregnated patch at the site of catheter insertion to decrease catheter-associated bloodstream infections.30
The final percutaneous method for catheter placement involves use of the Seldinger technique. A needle is used to pierce the anterior wall of the artery. When return of arterial blood is seen through the introducer needle, a guidewire is placed through the needle and advanced into the lumen of the artery. The needle is then removed, and a catheter is advanced over the guidewire into the lumen of the vessel. This method also can be used with a catheter over a needle. Confirmation of correct positioning and securing the catheter completes the procedure. A recent study in adults undergoing general anesthesia found no difference in the success rate or time to insertion when arterial catheters were placed using wire guides or without wire guides.31 Placement using the Seldinger technique is the preferred method when placing a catheter into larger vessels such as the femoral artery. When placing a catheter into a central artery using Seldinger technique, a longer catheter (e.g., 2.5 to 3 Fr, 5 to 8 cm) should be used. Such catheters are available in commercially made kits.
Recently, interest has grown in ultrasound-assisted placement of arterial catheters. A study of adult patients requiring arterial catheter placement in an emergency department setting demonstrated decreased time to insertion and decreased number of attempts at catheter placement using ultrasound-guided technique compared to traditional pulse palpation technique.32 A pilot study in pediatric patients undergoing surgery found that ultrasound-guided placement of radial arterial catheters had a higher success rate and required fewer attempts compared to traditional techniques.33 However, a larger pediatric study that randomized patients receiving radial arterial catheters to placement via ultrasound-guided versus traditional techniques by pediatric subspecialty trainees or anesthesiologists found no difference in success rate at the first cannulation site, total number of attempts, or time to successful cannulation.34
Maintenance of an Arterial Catheter
To prolong patency of an arterial catheter, heparinized fluid is most commonly infused through the catheter. A common practice is to infuse 0.9% sodium chloride containing heparin 1 U/mL at 3 mL/hr, although slower infusion rates may occasionally be used in small infants with a need for fluid restriction. Studies of perioperative arterial catheters in adults have found no difference in the rate of catheter patency using heparinized or nonheparinized solutions,35 but this does not take into account the smaller vessel size in children or the need for more prolonged catheter patency common to the care of the critically ill child. A meta-analysis of randomized controlled trials of heparin use to maintain either peripheral venous catheter or peripheral arterial catheter patency demonstrated a positive effect of heparinized fluid on duration of arterial catheter patency and the risk of clot formation.36 Comparison of normal saline to 5% dextrose in water, both with heparin, revealed that infusion of saline resulted in longer catheter life.37 Papaverine is a smooth-muscle relaxant that can decrease vasospasm when used in arterial catheter maintenance fluids. A randomized, controlled trial of the addition of papaverine (60 mg/500 mL) to routine arterial catheter fluids demonstrated a significantly lower rate of catheter failure and longer catheter life in the papaverine group.38 This study evaluated patients from 3 weeks to 18 years of age and recommended avoiding the use of papaverine in neonates due to a perceived increased risk of intraventricular hemorrhage (IVH). More recently, the use of papaverine-containing arterial catheter fluid in neonates from 25 to 36 weeks’ gestational age was shown to prolong catheter life without an increased risk of IVH.39 Despite these results, many institutions routinely avoid the use of papaverine in arterial catheter fluids in preterm neonates and in patients with traumatic brain injury or other preexisting intracranial hemorrhage for fear of causing or worsening an IVH.
For accurate direct measurement of blood pressure with an arterial catheter, one important consideration is the positioning of the transducer in relation to the catheter and the patient’s position. Standard practice for hemodynamic monitoring involves having the transducer zeroed to atmospheric pressure for accurate pressure measurement. The transducer is often maintained as close as possible to the level of the right atrium for accurate blood pressure measurements, particularly when the patient is in the supine position.40 Studies in animal models have demonstrated that positioning the transducer level with the aortic root results in accurate measurement of mean arterial pressure regardless of patient position or catheter site, while placement of the transducer level with the catheter tip resulted in significant error in mean arterial pressure measurement when the patient was in positions such as reverse Trendelenburg.41 It is common practice at present to change the fluids and tubing every 72 hours. A study that investigated increasing the interval for changing arterial catheter fluids and tubing from 48 to 72 hours showed no increased risk for catheter-associated infection.42 The overlying dressing also is changed on a scheduled basis.
Inability to draw blood from a catheter or flattening of the waveform on the monitor is suggestive of either a kinked catheter or thrombus formation at the end of the catheter. If evidence of compromised perfusion distal to the catheter is present, the catheter should be removed. If no evidence of compromised perfusion is present, changing the catheter over a guidewire may be considered. However, strong consideration should be given to removing the existing catheter and placing a fresh arterial catheter in a new position, as changing a catheter over a guidewire has been associated with an increased risk of catheter-associated bloodstream infection (CABSI), at least in central venous catheters.43
Complications
Complications related to arterial catheters include hemorrhage, thrombus formation, emboli, distal ischemia, and infection. Permanent ischemic complications related to radial artery catheters in adult patients are a very rare event.25 A recent study used ICD-9 codes to define arterial catheter complications in a large multi-institutional administrative database in an effort to examine the prevalence of and risk factors for arterial catheter complications in critically ill children.44 This study found a complication of some sort in 10.3% of patients with arterial catheters, most often infection/inflammation, and found a rate of thrombotic or embolic complications of 7.5%. Complications were more common in younger children and tended to be associated with longer hospital courses. Arterial catheter complications were independently associated with cardiac surgery, bone marrow transplantation, and dialysis, probably reflecting an effect of the severity of illness. In addition to bleeding, infection, and distal limb ischemia, an uncommon but well-recognized complication of arterial catheter placement is growth arrest due to physeal injury from extravasation, aneurysm formation, or ischemia.45 Such injury can occur to the femur, tibia, radius, or ulna.
Catheter-related infections can be local or the focus for systemic sepsis. The risk of catheter-related infection has previously been thought to be lower for arterial catheters than for central venous catheters. Recent studies, however, have found very comparable rates of catheter-related infection in critically ill patients having both types of catheters.46 The risk of arterial catheter infection has been related to the duration of catheter use and to placement of a catheter in the femoral artery. 46–48 In one recent study of catheter-related infections in children, the presence of an arterial catheter was noted to be a risk factor for any type of catheter-related infection, but in this study the arterial catheter most likely represents a surrogate marker for greater severity of illness.49 Regardless, however, the arterial catheter should be considered a possible source of sepsis, as is the central venous catheter, and strong consideration should be given to removing an arterial catheter when it is no longer absolutely necessary for optimal care.
Summary
Arterial catheters are a routine part of the monitoring of many critically ill children, and the ability to place an arterial catheter is a necessary skill for the pediatric intensivist. As with any procedure, the potential risks and benefits of arterial catheter placement should be carefully weighed prior to the procedure. Recent publications demonstrate that the rates of and risk factors for complications of arterial catheterization in critically ill children need further study.44
Pericardiocentesis
Indications
Drainage of a pericardial effusion of any cause is absolutely indicated when cardiac tamponade is present. Often drainage is recommended if the effusion is large, even in the absence of tamponade, for diagnosis and fluid removal.50 For small effusions, pericardiocentesis may be indicated for diagnosis alone. In pediatric patients, pericardial effusions most commonly occur with postviral or idiopathic pericarditis, but they are also seen with postpericardiotomy syndrome, collagen vascular disease, oncologic disease, and, rarely, uremia. Purulent pericarditis resulting from Staphylococcus aureus or Streptococcus pneumoniae infection can be seen in cases of concomitant pneumonia with empyema. Although rare in developed countries, tuberculous pericarditis can occur. Drainage of purulent pericarditis is indicated for relief of tamponade, prevention of constrictive pericarditis, diagnosis, and drainage of infection. With purulent pericarditis, open drainage may be more effective because of the difficulty in draining thick pus.51 If using a tube pericardiocentesis and drainage, instillation of a thrombolytic such as alteplase (recombinant tissue plasminogen factor) or urokinase may be considered with purulent effusions.52 Traumatic pericardial effusions secondary to penetrating trauma often require surgical drainage of the blood, because tamponade is common. Pneumopericardium secondary to pulmonary air leaks in mechanically ventilated patients is usually well tolerated hemodynamically but may require drainage, especially in small infants, because of the development of tamponade.
Contraindications
When acute tamponade is present, pericardiocentesis is unequivocally indicated. However, when elective or diagnostic pericardiocentesis is to be performed, the presence of a bleeding diathesis is considered a contraindication. The presence of aortic dissection is considered a major contraindication.50 Lack of experience with the procedure is a relative contraindication for elective pericardiocentesis. Open drainage is preferred to closed drainage when the patient has traumatic tamponade and is in cardiac arrest.53 When the effusion is loculated in a location not easily reached using the subxiphoid approach, needle pericardiocentesis is contraindicated because the risk of complications increases and the possibility of successful drainage becomes remote.
Equipment
Technique
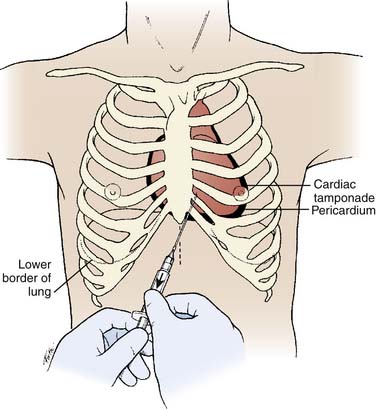
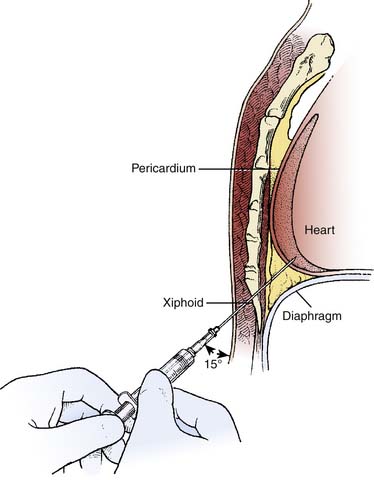
Echocardiographic guidance is recommended for most pericardiocenteses because it can be done at the bedside and is logistically less complex. The most common technique uses transthoracic scanning, which can easily visualize the effusion. Echocardiographic scanning is indicated prior to needle drainage or catheter insertion for any reason except tamponade with cardiac arrest. Pericardial fluid can be identified by computed tomography or magnetic resonance imaging. Because these techniques are cumbersome and time consuming, they should not be used in acute tamponade because echocardiography is more readily available at the bedside and is usually fast in skilled hands. The echocardiogram can show the size of the effusion, its distribution around the heart including any loculations, the presence of fibrin or clots, and evidence of tamponade.54 Tamponade can be diagnosed using two-dimensional imaging when the right atrium collapses during late diastole. Normally the right atrial free wall is concave throughout the cardiac cycle. With tamponade, the pericardial pressure exceeds the right atrial pressure at end-diastole and causes the right atrial free wall to collapse toward the center of the right atrium. The worse the tamponade, the longer into systole the collapse occurs.55 Echocardiographic guidance in patients with tamponade has been shown in adults to have a 99% success rate in relieving the tamponade.56 After the fluid has been echocardiographically evaluated, the patient is placed supine with the head elevated approximately 30 degrees. The subxiphoid approach is the safest and most common approach, although other approaches have been described. The approach is extrapleural and, in patients with normal anatomy, avoids major vessels such as the internal mammary, coronary, and pericardial arteries.50 The subxiphoid and lower costal margin are prepared with 2% chlorhexidine. The area is draped in sterile fashion. Lidocaine local anesthesia is infiltrated at the junction of the xiphoid and the left costal margin. The needle is inserted at a 30- to 45-degree angle with the needle directed toward the left clavicle (Figure 15-4). The slip-tip syringe is attached and is aspirated continually while the needle is inserted (Figure 15-5). Needle advancement is halted when air or fluid is aspirated. If blood is obtained, analysis is necessary to determine whether the blood is of pericardial or intracardiac origin. Several techniques are helpful for this determination. The hematocrit of pericardial fluid will be lower than that of intracardiac blood, which will be equal to the patient’s hematocrit. Dropping a few milliliters of the fluid on gauze sponges determines whether the fluid will clot. Fluid that does not clot is pericardial; fluid that does clot is most likely intracardiac blood.57 Another technique involves injection of small amounts of saline microbubble contrast (saline in a syringe that has been agitated) through the introducer needle while imaging with echocardiography.58 If contrast bubbles are seen in the heart, then the tip of the needle is intracardiac. If bubbles appear in the pericardial sac, then the needle is appropriately placed in the pericardium.
During insertion the needle is guided using two-dimensional echocardiography. The echocardiographic probe is placed on the chest where the fluid is best seen. The needle tip is identified by ultrasound and followed as the needle is advanced.59 Another technique involves mounting the needle on the echocardiographic probe, which has been placed in a sterile sleeve. The needle is advanced while the operator also handles the probe. This technique allows the use of locations other than the subxiphoid approach for insertion of the introducer needle, with the potential for better fluid visualization.60
Maintenance
The catheter is simple to maintain. The dressing should be changed according to the ICU protocol for central venous lines. The fluid in the drainage bag should be measured and the amount recorded on a regular schedule. If fluid is no longer draining, then a small amount (1 to 2 mL) of heparinized saline can be infused into the pericardium through the stopcock after preparation with antiseptic solution. This process can release any fibrinous material occluding the catheter. If no fluid is forthcoming, then echocardiography can be performed to determine if residual pericardial fluid remains. If more fluid is present, flush the catheter again in an attempt to open up the catheter. If the fluid had originally been purulent, then instillation of a fibrinolytic agent may allow better drainage. If no fluid remains, the catheter can be removed, depending on the patient’s condition and the underlying cause of fluid development.
Complications
Cardiac puncture is not an uncommon complication of the procedure. If the ventricle is entered and the needle quickly withdrawn, then the injury is minor and of no clinical consequence. Coronary laceration occurs rarely, resulting in acute ischemia, and has been associated with death from the procedure.61 The pleural space can be entered with the insertion needle or the catheter, resulting in a hemothorax or pneumothorax. Hemoperitoneum and pneumoperitoneum can occur. Injury to the diaphragm, intestines, and stomach have been reported. Infection of the indwelling catheter can occur, but is rare because the catheter usually is not in place for more than 3 to 4 days. Cardiac arrest and death have been reported during pericardiocentesis.62, 63 In a retrospective study of pericardial drainage catheters in pediatric patients, Zahn et al.64 noted only five complications in a total of 43 procedures. Four of the complications were considered minor and included myocardial perforation with no hemodynamic alteration, pneumopericardium, and ST-segment elevation. One critically ill neonate who had suffered a myocardial perforation during cardiac catheterization died. The results of the study indicated that pericardial catheter placement in pediatric patients is a relatively safe procedure. Most complications of pericardiocentesis with or without catheter placement can be prevented by careful guidance of the needle with echocardiography and greater experience of the practitioner.
Interpretation
With acute nonpurulent pericarditis the fluid should be evaluated for viruses; Coxsackie viruses are the most common causes of viral pericarditis. Viral culture can be performed, although the yield is generally low. Polymerase chain reaction has been used successfully to diagnose viral and bacterial etiologies.65 For purulent pericarditis, Gram stains and acid-fast bacilli stains should be performed, as should appropriate bacterial (both aerobic and anaerobic) and fungal cultures, as well as bacterial PCR analysis. If tuberculous pericarditis is suspected, adenosine deaminase (ADA) and PCR for mycobacteria are indicated.50
Umbilical Arterial Catheter and Umbilical Venous Catheter Placement
Umbilical Artery Cannulation
Indications for umbilical artery cannulation (UAC) placement include the need for frequent monitoring of acid-base balance, continuous measurement of blood pressure, angiography, resuscitation, and exchange transfusions. Infusions of medications or fluids may be warranted when a UAC is present, but placement of a UAC is not indicated for infusions alone. UAC placement is contraindicated in patients with omphalitis, peritonitis, necrotizing enterocolitis, omphalocele, hypercoagulable states, or known ischemia of the perineum, or lower extremities.66,67
Supplies and Equipment
A bed with adequate lighting and a heat source are essential. Prepackaged UAC trays are commercially available and contain different sizes and types of catheters. Umbilical catheters should be radiopaque with rounded tips and single holes. A Luer-Lok system is available on some catheters and has some advantages; others need trimming and attachment of a blunt needle to connect them to a three-way stopcock. Babies weighing less than 1500 g need a 3.5 Fr catheter; infants weighing more than 1500 g require a 5 Fr catheter.68 Other supplies needed include povidone-iodine or chlorhexidine solution; umbilical tie; sterile drapes; gloves; scalpel; scissors; iris forceps; pick-ups; gauze pads; 3-0 silk suture; 3-mL, 5-mL, or 10-mL syringes; tape; and heparin flush (1 unit heparin per milliliter of normal saline).69
Technique
Prior to UAC placement, gently restrain the baby and determine the catheter insertion distance. Restrain the infant in a supine position by using soft restraints of the arm and legs. Alternatively, restrain the baby by swaddling technique.
High or low placement of the catheter is based on the vertebral level at which the catheter resides in the aorta. Complications have been reported with both low and high UACs.70–72 A low UAC should lie at or below the third lumbar vertebra (caudal to the origins of the renal arteries).73 A high UAC should have its tip between the sixth and ninth thoracic vertebrae. A high UAC position is the preferred position and a low UAC should only be used if a high UAC is not attainable.74 The calculation for insertion length can be determined using various methods, such as birth weight, shoulder-to-umbilicus length, and total body length.75–77 A simple method for calculating insertion depth for high placement is as follows: for babies weighing more than 1500 g (3 × birth weight [in kg]) + 9 = centimeters of catheter to insert to the umbilical ring; for babies less than 1500 g, use the formula (4 × birth weight [in kg]) + 7 = centimeters of catheter to insert to the umbilical ring.78,79
Next, attach the UAC to a three-way stopcock, and also attach to the stopcock a 3- or 5-mL syringe filled with heparin flush. Fill the stopcock and UAC with heparin flush solution. Turn the stopcock off to the catheter prior to insertion. Prepare the cord with antiseptic solution and drape the baby, sparing the head and chest to allow for patient monitoring during the procedure. Place an umbilical tie snugly around the epithelialized portion of the umbilical cord using a one-looped tie. The umbilical tape should be able to apply pressure to the cord in the event of acute hemorrhage, but should not be so tight as to hamper introduction of the catheter. Use a scalpel to cut the cord horizontally approximately 1 to 2 cm above the umbilical ring. The larger thin-walled umbilical vein is typically in the 12 o’clock position (cephalad) and two small thick-walled umbilical arteries can be identified at the 5 and 7 o’clock positions. Grasp the cord securely with a hemostat (or forceps) near one of the umbilical arteries. Use the iris forceps to dilate an arterial lumen by first inserting the forceps in the closed position, finally allowing both prongs to spring open and dilate the lumen. Holding the catheter with the iris forceps, introduce the catheter into the dilated artery, taking care to ensure that the catheter is in the lumen of the vessel. Insert the catheter approximately 0.5 cm and pull the umbilical cord toward the infant’s head before attempting to advance the catheter. Aspirate blood and flush the catheter once it has been advanced to the desired length. Ensure air bubbles are cleared prior to flushing the catheter. If the catheter meets resistance, apply gentle steady pressure for approximately 30 seconds to determine if the catheter will advance. Do not force the catheter. If the catheter will not advance or no blood return is seen, a false passage may have been created. A double-catheter technique can be attempted in this situation.80 Leave the catheter that is meeting resistance in place and carefully advance a second catheter beside it to the appropriate distance. If the double-catheter technique fails, the second umbilical artery can be cannulated. Suture the catheter in place, using a pursestring stitch cinched tightly to provide hemostasis and wrapping both ends of the suture around the UAC before tying a square knot. Secure the line using a tape bridge or other available securing device. Finally, loosen the umbilical tie and keep it in place for any needed hemostasis. A transducer may be attached for continuous blood pressure monitoring while still allowing for blood sampling. Anteroposterior and lateral x-ray films of the abdomen are needed to confirm proper positioning of the catheter. A malpositioned catheter should be adjusted promptly. If it is too high, it should be pulled back; if it is too low or in a vessel other than the aorta, the catheter should be removed and replaced.67 Never advance a UAC once the sterile field has been broken.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree