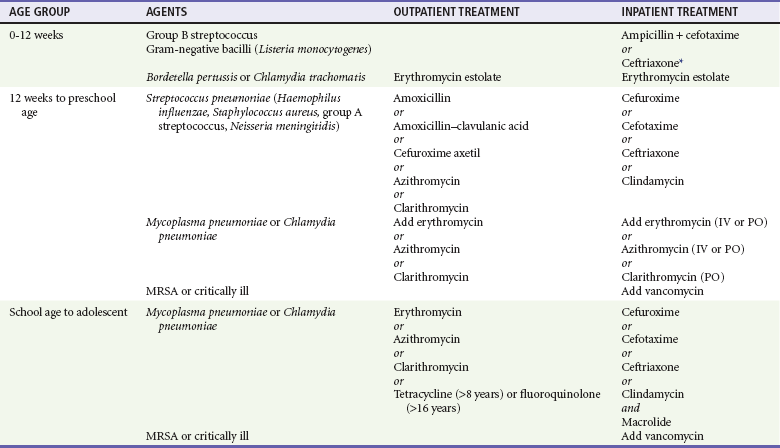
Chapter 170 The causative organisms also vary with the age of the child. Because the organism is not definitively identified in most pneumonia cases, it is difficult to determine the true incidence of the specific etiologic agents.1 Overall, it has been estimated that viral agents cause 60 to 90% of pneumonias.2 Viral agents are more common in younger children. Bacteria predominate in neonates but are a less frequent causative agent in toddlers and older children. Outside of the neonatal period, the incidence of bacterial agents is stable throughout different age groups.2 Mixed viral and bacterial infections or concomitant bacterial infections may occur in one third of pneumonias.2,3 Chlamydia trachomatis is a unique cause of pneumonia in infants 3 to 19 weeks old. Bordetella pertussis classically occurs in children younger than 1 year but also occurs in older children and adolescents.4,5 Mycoplasma pneumoniae is one of the most common causes of pneumonia among children older than 5 years and may play a role in younger children.6,7 Chlamydia pneumoniae is more often seen in children older than 5 years but also may cause infection in younger children.7,8 Among bacteria, group B streptococci and gram-negative bacilli predominate in neonates. Ureaplasma urealyticum and Listeria monocytogenes may cause illness in infants younger than 3 months.1 Streptococcus pneumoniae is the leading bacterial cause of pneumonia in all age groups beyond the newborn period; Haemophilus influenzae and Staphylococcus aureus are less common etiologic agents, most often seen in the first years of life. The incidence of H. influenzae type b disease has decreased by 90% since the onset of immunization of infants and young children.9 The heptavalent pneumococcal conjugate vaccine Prevnar (Lederle Laboratories/Wyeth-Ayerst Pharmaceuticals, Wayne, N.J.) was licensed by the U.S. Food and Drug Administration in 2000 and is recommended as a primary series at 2, 4, and 6 months of age, with a fourth booster dose given at 12 to 15 months of age. Clinical trials suggested 85% protection against serotype-specific cases of bacteremic pneumonia.10 Studies have also shown a decrease in carriage rates of the serotypes included in the daycare setting.11 Pneumococcal polysaccharide vaccines have been recommended for children older than 2 years at high risk for pneumococcal disease since 1985, but they are not immunogenic in younger patients. Pneumococcal vaccine has also been shown to provide some protection against viral pneumonia. One study found a 31% reduction in the incidence of pneumonia associated with seven respiratory viruses in hospitalized children. This may be because viral pneumonia in hospitalized children is often associated with concurrent pneumococcal infection.12 Other, less common bacterial agents include group A streptococci, Neisseria meningitidis, and anaerobic bacteria, the last being particularly common in the setting of aspiration pneumonia. Unusual causes of pneumonia include Pseudomonas aeruginosa, Legionella pneumophila, Pneumocystis jiroveci, and rickettsial infections. The incidence of Mycobacterium tuberculosis is increasing in the United States, particularly in urban and low-income areas and among nonwhite racial or ethnic groups. Infants and adolescents are at highest risk in the United States. Bacterial pneumonia and mycoplasmal infections are transmitted most often person to person by droplet aspiration. Asymptomatic upper airway colonization often occurs in children and may spread infection to other children.13 Less commonly, bacterial pneumonia also may result from hematogenous spread from a distant focus or during primary bacteremia. Viral agents that cause pneumonia proliferate in the upper respiratory tract and spread contiguously to involve the lower respiratory tract. Viruses such as varicella, CMV, herpes simplex, Epstein-Barr, measles, and rubella also may infect the lung through hematogenous spread. History.: Clinical symptoms and signs of pneumonia in pediatric patients vary with the age of the patient, specific pathogen, and severity of the disease. Infants younger than 3 months generally have respiratory symptoms, such as tachypnea, cough, retractions, and grunting, but may show only nonlocalizing symptoms, such as isolated fever or hypothermia, vomiting, poor feeding, irritability, and lethargy. Toddlers with S. pneumoniae infection may have nonspecific symptoms, such as high fever and lethargy, without respiratory symptoms. In general, with increasing age, signs and symptoms in children become more specific and are manifestations of generalized infection, lower respiratory tract disease, and associated extrapulmonary disease, although pneumonia in any child may have only a few or subtle manifestations. General symptoms related to the infection include fever and chills, headache, rigors, and malaise. Symptoms of lower respiratory tract disease may include cough and wheezing. Pleural irritation may cause chest, abdominal, or neck pain or result in neck stiffness. Vomiting or poor oral intake can be seen with pneumonia of any cause and may imply more severe disease or dehydration. Physical Examination.: Physical examination of a child with suspected pneumonia should begin by noting the general appearance and breathing pattern. Vital signs, including oxygen saturation, also should be evaluated on arrival. Important findings include toxicity, level of alertness and interaction, color, and state of hydration and perfusion. Fever most often is present with bacterial pneumonia but may be low grade or absent in neonates and patients with nonbacterial disease. Cardiovascular parameters may indicate dehydration or, rarely, shock. Tachypnea, although not universal, is the most sensitive indicator of pneumonia and may be the only manifestation in a young child.14 The World Health Organization has published guidelines for the clinical diagnosis of pneumonia in developing countries and cites tachypnea and retractions as indicators of lower respiratory disease. Tachypnea is defined by the World Health Organization as a respiratory rate of more than 50 breaths/minute in infants younger than 1 year and more than 40 breaths/minute in children older than 1 year.15 Other manifestations of lower airway disease may include cough, wheezing, nasal flaring, retractions, grunting, and use of accessory muscles. The characteristics of the cough may aid in the diagnosis; a staccato and paroxysmal cough in an infant may indicate pneumonia caused by C. trachomatis or B. pertussis. A hacking quality is often present with Mycoplasma infection. Auscultatory examination of an older child may reveal rales, wheezing, and diminished breath sounds, often with dullness to percussion and associated decreased fremitus. Although these findings may be present, the clinical findings are much less consistent in a younger child; rales may be masked by poor inspiratory effort or noisy upper airway sounds. Perspective.: S. pneumoniae is one of the most frequently seen bacterial agents causing pneumonia in children.12 Whereas any child can acquire S. pneumoniae, children at increased risk for development of infection from S. pneumoniae are children with immune deficiency, chronic renal disease, or functional or anatomic asplenia and Native Americans.10 S. aureus pneumonia, although less common, tends to cause a more severe pneumonia; more than 70% of all cases occur in the first year of life.16 Children with foreign body aspiration, immunosuppression, or skin infections may be at increased risk for S. aureus pneumonia. Progression of the disease is rapid, and empyema (90%), pneumatocele (50%), pneumothorax (25%), and bacteremia are common complications (Fig. 170-1). In contrast to classically described methicillin-resistant S. aureus, which is typically broadly resistant and nosocomially acquired, this agent is resistant to fewer antibiotics.17 Before widespread immunization, H. influenzae was the second most common bacterial cause of pneumonia. However, its incidence has decreased by 90% since the onset of effective immunization, and it is rarely seen presently.9 H. influenzae previously was considered a disease of younger children, but most cases now occur in older children.18 Although it is often clinically indistinguishable from S. pneumoniae pneumonia, H. influenzae pneumonia has a higher incidence of associated pleural effusions (25-75%) and bacteremia (75-95%).19 Although it is still uncommon, the incidence of group A streptococcal pneumonia may have increased since the 1980s. One study reported an increase in the incidence from 0.16 per 100,000 in 1992 to 0.35 per 100,000 in 1999 in Canada, whereas another study suggested stable rates since the 1980s.19,20 Group A streptococcal pneumonia may occur sporadically and may be a complication of varicella.19 It is typically a severe illness with abrupt onset, rapid progression to toxicity, and high fatality rate (30-60% fatality rate reported in a study of all ages).19 Clinical Features.: Bacterial pneumonia beyond the neonatal period generally has a sudden onset, and fever is almost universal (temperature often above 39° C). Patients may or may not have a cough and often appear relatively toxic with tachypnea disproportionate to the fever. Confined rales or wheezes and localized decreased or tubular breath sounds commonly occur in older children, although the physical examination in a younger child may be completely unrevealing. Diagnostic Considerations.: Patients with pneumococcal infections often have a preceding dramatic presentation with high white blood cell (WBC) counts with associated pleural effusion and bacteremia in 10 to 30% of children.21 Radiographic findings may show an alveolar infiltrate in a patchy or consolidated lobar (Fig. 170-2) or subsegmental distribution, although patients with bacterial pneumonia may have an interstitial infiltrate.22 Bilateral involvement, pleural effusion, pneumatocele, and pneumothorax may occur with more severe disease. Although the WBC count may be normal with bacterial pneumonia, leukocytosis often occurs, sometimes exceeding 20,000/mm3. Uncomplicated bacterial pneumonia often has a rapid response to institution of appropriate antibiotics; a stagnant or worsening clinical picture should prompt further investigation. Management.: Of particular concern is the emergence of resistance to penicillin and cephalosporins. At this time, it seems that the outcome of otherwise healthy children with pneumonia secondary to resistant pneumococcus may not differ significantly from the outcome of children with pneumonia secondary to penicillin-sensitive pneumococcus.23 Pneumonia caused by S. pneumoniae may be complicated by empyema, pleural effusion, lung abscess, or necrotizing pneumonia. Since the 1990s, there seems to have been an increase in the incidence of such complications; one study noted an increase from 22.6% in 1994 to 53% in 1999 in children hospitalized with pneumococcal pneumonia.56 It does not seem that this increased incidence is related to intermediate resistant organisms. It is unclear if highly resistant organisms play a role.56 High-dose amoxicillin is recommended for initial outpatient treatment of suspected pneumococcal pneumonia in children younger than 4 years; a standard dose may be used in older children who are immunocompetent (Table 170-1). Children who appear well can be treated with oral antibiotics. In some cases, a dose of intravenous antibiotics followed by an oral prescription may be beneficial. One study reported decreased admission rates for children with S. pneumoniae given an initial intravenous dose of antibiotics followed by oral antibiotics.56 Most viral pneumonias resolve without specific therapy. Because of the likelihood of bacterial superinfection and the difficulty in differentiating between bacterial and viral pneumonia, antibiotics should be considered in a more severely ill child. Potential complications include dehydration, local progression of the disease, bronchiolitis obliterans, and apnea (most commonly in the first 3 months of life).25 Mycoplasmal pneumonia accounts for 10 to 20% of all pneumonias and has traditionally been thought to occur most commonly in 5- to 18-year-olds. It is now clear that it also may play a significant role in younger children but is still rare in infants younger than 1 year.25 The onset is classically gradual and insidious, but some patients also may present with abrupt onset of symptoms similar to its bacterial counterpart.4 Prodromal symptoms include fever, headache, and malaise, followed several days later by a nonproductive, hacking cough. Patients also may present with pertussis-like illness. Other symptoms of infection may include hoarseness, sore throat, and chest pain; coryza is unusual. Children with mycoplasmal pneumonia generally appear nontoxic. Patients may have rales; wheezing occurs less often. Pharyngitis, cervical lymphadenopathy, conjunctivitis, and otitis media may occur occasionally. Bullous myringitis, although rare, is believed to be indicative of Mycoplasma.25 Rash is present in 10% of patients and may be urticarial, erythema multiforme, maculopapular, or vesicular.26 The course may be complicated by pneumatocele, pleural effusion, pneumothorax, or bronchiectasis. Mycoplasma, typically thought to be a benign and self-limited infection, has been shown to play a significant role in exacerbation of asthma and may cause chronic pulmonary structural abnormalities.4 Laboratory diagnosis is problematic. Although it has been used in the past, bedside cold agglutination testing is a poor indication of infection, especially in patients younger than 12 years, and is rarely used today.25 Infection often is diagnosed clinically and treated empirically. Diagnosis may be confirmed with acute and convalescent antibody titers; however, patients may take 4 to 6 weeks to seroconvert, and some patients may fail to mount an immune response.4,26 Culture is not routinely available; polymerase chain reaction diagnosis at this time is available only from research laboratories.4 Complications are varied but unusual and include hemolytic anemia, myopericarditis, neurologic disease (meningoencephalitis, Guillain-Barré syndrome, transverse myelitis, cranial neuropathy), rhabdomyolysis, arthritis, and rash. C. trachomatis is a common sexually transmitted organism causing cervical infection in 2 to 30% of pregnant women.8 It can be transmitted from the genital tract of infected mothers to their newborn infants, resulting in conjunctivitis in 22 to 44% and pneumonia in 5 to 20%.8 An infant with pneumonia caused by C. trachomatis presents at 3 to 19 weeks of age after colonization with the organism at birth. The illness usually begins with nasal congestion followed by cough. In half of the cases, conjunctivitis precedes the onset of respiratory symptoms. The infant is often afebrile and alert but tachypneic, with a repetitive staccato cough that may interfere with feeding or sleeping. It can resemble the paroxysms of pertussis and occasionally precipitates episodes of alarming respiratory distress. Mild retractions and diffuse inspiratory crepitant rales are noted on chest examination; expiratory wheezing is usually absent or minimal. Middle ear abnormalities are present in half of the cases. The radiograph usually shows hyperinflation with bilateral and symmetrical diffuse interstitial infiltrates (Fig. 170-3). The total WBC count is usually normal but often with an eosinophilia of more than 400/mm3.8 Definitive diagnosis is made by isolation of the organism in the tissue culture specimen; diagnostic tests based on polymerase chain reaction are more sensitive than fluorescent antibody stain or tissue culture but may not be as specific. Although it is often a mild illness, chlamydial pneumonia may be complicated by apnea and hypoxemia. Treatment with erythromycin may shorten the course; however, the disease tends to be protracted, with cough and tachypnea often requiring weeks to clear despite the administration of antibiotics.
Pediatric Respiratory Emergencies
Disease of the Lungs
Pneumonia
Epidemiology
Principles of Disease
Clinical Features
Specific Disorders
Viral Pneumonia
Mycoplasmal Pneumonia
Chlamydial Pneumonia
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Pediatric Respiratory Emergencies: Disease of the Lungs
Only gold members can continue reading. Log In or Register to continue