Chapter 55 Pediatric Neurologic Assessment and Monitoring
Overview and Basic Principles of Pediatric Intensive Care Unit Neurology
The approach to the neurologic assessment of the patient in the pediatric intensive care unit (PICU) requires an interdisciplinary approach using bedside neurologic examination and laboratory testing combined with invasive and noninvasive monitoring.1 While this approach to patients with neurologic disorders recapitulates elements of the approach to differential diagnosis used in the outpatient setting and non-ICU inpatient care, there are important fundamental differences that are specific to the practice of critical care neurology.2,3 In general, these differences involve the need to obtain testing (imaging, neurophysiology, laboratory) on patients who may appear neurologically intact, the need to intervene before a specific neurologic diagnosis has been obtained, and the challenge of determining whether such interventions affect long-term outcome. Thus, the cardinal features of the practice of neurology in the PICU are the need for serial neurologic examinations, the importance of communication between nurses and physicians and between multiple medical services, the need for early recognition of changes in the neurologic exam, and the anticipatory management of patients with the potential for progressive neurologic deterioration. The confounding effects of sedation and/or postoperative anesthesia on neurologic functioning pose an additional set of challenges to the assessment of these patients. Nevertheless, a logical approach to the neurologic examination is possible by using the standard structure of a neurologic examination, combining this exam with attention to the mechanisms of injury (present or potential), and thereby developing a plan for ongoing monitoring and management. Last, it is prudent to regard every patient in the PICU as having the potential for neurologic complications of his or her illness. These patients, whose primary diagnoses range from neurologic complications of solid organ transplant to liver failure to congenital heart disease, may suffer neurologic injury from any combination of hypoxic, ischemic, inflammatory, or metabolic cerebral insults.
Recognition of Neurologic Complications in the PICU Patient
Children who develop neurologic complications of critical illness deserve a specific mention. This is likely an underrecognized population in many PICUs, not least because of the prevalence of nonconvulsive seizures4 (NCS) or ICU-acquired paresis.5 In these cases, the recognition of new neurologic deficit(s) relies on the ability of the PICU team to recognize changes in the neurologic exam. In general, interventions to treat or attenuate neurologic insults, whether seizures, ischemia, or increasing intracranial pressure (ICP), are more likely to be successful if initiated early in the process of injury. This means that effective neurologic monitoring in the PICU does not rely solely on the availability of a neurologist, electroencephalogram (EEG), or neuroimaging. Rather, the prerequisite to using these monitoring tools is a high index of suspicion for new neurologic injury on the part of the medical team for patients who do not have primary neurologic injuries.
In addition to the physical exam, there are a number of modalities that can be used for the monitoring of neurologic function in critically ill children and adults.6,7 This includes continuous EEG monitoring, which is well-established as a modality essential for the detection of NCS in the adult and PICU populations,8,9 ICP monitoring, transcranial Doppler,10 and metabolic11 and tissue oxygen monitoring.6,12 Thresholds for detection of cerebral ischemic injury have been proposed for brain oxygen tension13 and near-infrared spectroscopy (NIRS).14 With respect to pediatric neuromonitoring, as yet there is no consensus on normal values or the age-dependence of these endpoints.
Iatrogenic Complications of Pharmacotherapy
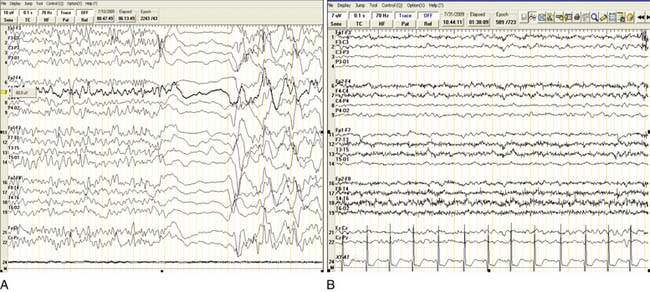
It is not uncommon to overlook the side effects of drugs in the PICU. A review of medications should be part of the neurologic assessment of any patient with new neurologic symptoms. The initial assessment of the patient should include attention to medications that cross the blood-brain barrier, or that may interfere with the renal or hepatic metabolism of centrally active drugs. In patients in renal or liver failure, or requiring dialysis, the side effects of a centrally acting drug must be considered in the differential diagnosis for any neurologic symptom. This may occur even in the presence of “normal” doses of drugs or levels of anticonvulsants, as off-target drug toxicities may be due to metabolites, not the drug itself. An example is shown of a child with a mild static encephalopathy and spasticity, on dialysis as the sequela of perinatal renal injury, who developed progressive encephalopathy (Figure 55-1). Treatment with flumazenil with immediate improvement in mental status, confirmed that the accumulation of baclofen in this dialsysis-dependent patient was the source of a waxing and waning encephalopathy. Common examples in the PICU include immunophilin-associated seizures, encephalopathy, hypertension; oculogyric crisis, delirium during reduction of sedation, and persistent paralysis from prolonged neuromuscular blockade. In many cases, the attribution of the symptoms to a drug side effect (excess level, too-rapid withdrawal, idiosyncratic reaction, impairment of clearance) will be a diagnosis of exclusion. Nevertheless, a review of medications and recent changes should be a routine component of the neurologic assessment.
Approach to the Physical Exam
Vital Signs
Therapies that target specific mechanisms of cell injury for acute CNS disease are lacking in adult and pediatric neurocritical care. Nevertheless, one simple intervention, the prevention of hyperthermia, may significantly reduce neurologic injury after stroke or traumatic brain injury (TBI). The neuroprotective benefit of induced hypothermia remains to be proven for pediatric TBI.15–17 While hypothermia may remain as yet an unproven therapy for neurologic insults, the prevention of hyperthermia can be regarded as a safe, and probably effective, intervention.18 Therefore, as a general principal for ICU neurology in patients with known or suspected central nervous system (CNS) injury, the neurologic exam should first include vital signs and fever should be treated aggressively. The range of temperatures determined to be “normothermic” may vary but a consensus should be reached and temperatures above the accepted range treated quickly.
In contrast to adults, there are limited data on the optimum ranges for blood pressure, ICP, and cerebral perfusion pressure (CPP) for children. In adults, there are goal-directed protocols aimed at improving outcome following TBI. The targets of ICP less than 20 mm Hg and CPP above 60 mm Hg are based on a number of studies.19–23 In contrast, very limited data exist for children with TBI.24,25 Guidelines suggest an ICP threshold of 20 mm Hg for all ages and a CPP threshold of 40 to 65 mm Hg as an “age-related continuum.”26 In children younger than 15 years of age, a mean CPP less than 40 mm Hg during the first 48 hours following injury has been associated with increased mortality.27 Although children with TBI younger than 2 years of age have a high mortality rate compared with older children, no thresholds for ICP or CPP have been established for this age group.28 Accordingly, blood pressure, temperatures, and oxygenation must be interpreted in the context of the underlying neurologic insult or risk for further injury. As a general principle, hyperthermia with the attendant increase in cerebral metabolic demand should be treated aggressively whatever the primary injury.29
General Physical Exam
An essential component of the neurologic examination is obtaining an accurate head circumference. This may serve as a baseline for following the development of hydrocephalus in the at-risk infant. In older children, an abnormal (large or small) head circumference may be a previously overlooked sign of pathology. The fontanelle should be palpated and the findings on the exam agreed upon with the infant in a quiet, resting state. A bulging fontantelle is an important finding of meningeal irritation or increased ICP. Examination of skin for the cardinal features of the phakomatoses may identify café au lait spots characteristic of neurofibromatosis, or shagreen patches, hypopigmented macules, and angiomyofibromas characteristic of tuberous sclerosis. The physical findings associated with inflicted trauma deserve particular mention as these may be subtle30; they include unusual patterns of bruising, blood in the oropharynx, and burn or belt marks.
Importance of Observation in the Neurologic Exam
The pattern of breathing rate and rhythm should be observed. Specific patterns may help localize the site of neurologic dysfunction but not the mechanism involved (Table 55-1). The crescendo-decrescendo pattern alternating with periods of apnea, characteristic of Cheyne-Stokes respiration, may be due to dysfunction of the cerebral hemispheres, the thalamus, or the hypothalamus with preserved brainstem function, but can also be found in patients with congestive heart failure or primary respiratory disease. Similarly, the sustained, deep breathing pattern of central neurogenic hyperventilation may be due to either structural injury to the midbrain, sepsis, pulmonary disease, or compensated metabolic acidosis.
Table 55–1 Approach to the ICU Neurologic Examination: Localization and Mechanism
| Exam Finding | Structural-Vascular Insult | Toxic-Metabolic |
|---|---|---|
| Consciousness | Stays at same level or deteriorates | Waxes and wanes, milder impairment; toxins may cause progressive decline |
| Respiration | Cheyne-Stokes (crescendo-decrescendo alternating with apnea): loss of cerebral, thalamic, or hypothalamic control of breathing | |
| Fundoscopy | Papilledema due to increased ICP | Papilledema does not occur except in hypertensive encephalopathy, lead intoxication, hypoparathyroidism |
| Eye position | ||
| Pupil reactivity | ||
| Eye movements | If asymmetric, likely structural | Roving more common with metabolic derangements Absence of all movement with intact pupil light reflex |
| Adventitous movements | Restlessness, tremor, spasm, myoclonus, chorea, akathisia | |
| Muscle tone | Asymmetric; increased, normal, or decreased | Symmetric, normal, or decreased |
The conventional neurologic examination proceeds from mental status, cranial nerves, motor (bulk, tone, and strength), reflexes, and sensation to cerebellar exam and gait. In children and in the PICU in particular, the exam must be based on good observation and typically performed out of sequence. It is easier to assess tone and reflexes in the asleep, relaxed patient, before waking the patient up to assess mental status. While the exam is discussed in the standard order below, it is often more informative to begin the hands-on part of the exam with assessment of tone and reflexes. Once awake and agitated, it may be difficult to elucidate subtle asymmetries of tone and reflexes, which may be key findings of the exam.
The state of arousal (awake, asleep), responsiveness, (interactive, verbal, nonresponsive), position (tone and asymmetry of limb position), movement (purposeful, spontaneous, dystonic, choreic, asymmetry of movement) can all be reliably assessed by observation. In a nonintubated, nonsedated patient the examiner may proceed directly with a standard mental status exam adjusted for age. In the young child who is able to cooperate, the specific cognitive and language skills expected for age can be assessed (Table 55-2).
Table 55–2 Age-Dependent Motor and Language Patterns
| Age (mo) | Motor | Language |
|---|---|---|
| 15 | Walks alone, crawls up stairs | Jargon; follows simple commands |
| 18 | Runs, sits on chair, walks up stairs with hand held | Knows 10 words, names pictures, identifies body parts |
| 24 | Runs well, walks up and down stairs | Uses three-word sentences |
| 30 | Jumps | Refers to self as “I” |
| 36 | Stands on one foot, goes up stairs with alternating feet | Knows age and gender, counts three objects |
| 48 | Hops on one foot, throws ball | Tells a story |
| 60 | Skips | Names four colors, repeats 10-syllable sentences |
Modified from Behrman RE, Kliegman RM, Nelson WE, et al: Nelson textbook of pediatrics, ed 14, Philadelphia, 1992, WB Saunders, pp 18–104.
Nonorganic Pathology in the Pediatric Intensive Care Unit
Not all neurologic deficits in the PICU are organic. Conversion disorders also occur in critically ill patients or result in patients being admitted to the PICU. In the latter case, this is most often associated with nonepileptiform seizures. These cases may have been treated with anticonvulsants, resulting in respiratory depression requiring intubation or ICU monitoring. A number of features of the examination and history may help make this distinction (Table 55-3). Seizures are a common complication of critical illness in adults and children31 and are also a common reason for neurologic consultation in the PICU. A high index of suspicion for seizures in the PICU is important in order to decrease the risk for secondary brain injury resulting from the metabolic stress imposed by seizures. In such cases, video EEG monitoring is the most efficient means of distinguishing ictal from nonictal events. While continuous EEG monitoring may be needed to determine whether such events are seizures or not, there are features of the physical exam that may aid in making this diagnosis. In general, and particularly in infants, the eyes are open during a seizure. In one series,32 over 90% of cases with electrographically confirmed seizures occurred with eye opening. The eyes may look straight ahead, versively deviate to one side contralateral to the hemisphere from which the seizures originate, or exhibit only nystagmus. Seizures are typically a “positive” phenomenon and will have movement associated with them unless there has been injury to the corticospinal tracts resulting in a paretic limb. Other features of the exam or description of the spells including stereotypy, crescendo-decrescendo behavior, or the presence of automatisms may help to distinguish ictal and nonictal behavior. In most cases, video EEG monitoring is the most efficient means of distinguishing ictal from nonictal events.
Table 55–3 Clinical Features of Seizures and Nonepileptic Spells
| Seizures | Nonepileptic Spells | |
|---|---|---|
| Eyes | Open | Closed |
| Automatisms | Common | Rare |
| Stereotypical behavior | Common | Rare |
| Gradual onset | Rare | Common |
| Waxing and waning course | Rare | Common |
| Thrashing movements | Rare | Common |
Even in the PICU, the examiner should remember that functional deficits may occur, and a number of motor signs may help identify the origin of functional symptoms. Given the complex pathophysiology of many critically ill patients and the multiple potential mechanisms of neurologic injury, the diagnosis of a functional neurologic deficit should be made only after a thorough evaluation for organic causes. Although this is uncommon in the PICU, a functional etiology should not be overlooked and early identification may help to minimize diagnostic testing and unnecessary or high-risk treatment. There are a number of elements of the physical exam that may help distinguish between organic and functional neurologic deficits.33 An inconsistent examination may be the first clue; for example, a patient with apparent weakness during bedside strength testing may be noted to change position during sleep or another may walk despite apparent paresis on bedside testing. These observations can often be very helpful in the assessment of children with weakness thought to be due to a neuromuscular disease. After first observing for inconsistency, the most useful test for functional weakness is the Hoover sign. This test relies on the principle that when flexing one’s hip, the natural accompanying movement is to extend the contralateral hip.33 With the patient supine, the examiner places one hand on the weak leg and the other hand under the ankle of the strong leg. The patient is then asked to perform a straight-leg raise of the healthy limb. In a functional pattern of weakness, the examiner will feel no downward pressure from the good leg since there is no effort being applied to raise the ostensibly weak leg. Other tests include the “arm-drop” in which a paretic or plegic arm is dropped over the patient’s face (the patient with organic weakness is more likely to allow the arm to strike the face), or observation of exact splitting of sensory or vibration deficits in the midline. A number of functional gait disturbances are also characteristic, including a monoplegic dragging gait (the whole limb is dragged without the circumduction present in pyramidal hemiparesis), a “walking on ice” pattern, excessive slowness, or sudden buckling at the knees with recovery. Of these, none are definitively diagnostic of a functional pathology, and in children in particular must be interpreted with caution. Importantly, functional and organic deficits may coexist.
Assessment of Level of Consciousness and Mental Status
For children with depressed consciousness, the precise stimulus required to elicit a response and the nature of this response should be specified. It is not helpful to describe the patient as “lethargic” or “obtunded.” First, the child is called by name to determine whether there is a response. If this is not effective, the examiner may ask a family member to speak to the child. Next, the stimulus is increased. It is most helpful to simply describe the patient’s response to specific stimuli and to use the same stimuli for serial examinations. The Glasgow Coma Scale score, although of limited use in preverbal children, is a quantitative measure (Table 55-4). If the patient’s eyes open to voice, the response to commands is next tested. This is discussed in more detail below, but the commands should be increased in complexity from one-step to two- or three-step. If there is no response to voice, a painful stimulus is next applied. It should be noted that in patients with sensory deficits due to neuropathy, spinal cord, or CNS lesions or with focal limb weakness, the extremity or dermatome selected for testing should have intact sensory or motor function. In the sedated or severely impaired patient the response may comprise only increase in heart rate. It is important that the stimulus and the specific response, rather than vague descriptors (“lethargic, drowsy, sleepy”) are documented, as this will be more helpful in assessing serial examinations. The rate of sedating drugs or recent administration of sedating drugs should be documented with this exam.
| Activity | Best Response | Score |
|---|---|---|
| Eye opening | Spontaneous | 4 |
| To command | 3 | |
| To pain | 2 | |
| None | 1 | |
| Verbal | Oriented | 5 |
| Confused | 4 | |
| Inappropriate words | 3 | |
| Incomprehensible sounds | 2 | |
| None | 1 | |
| Motor response | Obeys commands | 6 |
| Localizes pain | 5 | |
| Withdraws to pain | 4 | |
| Abnormal flexion to pain | 3 | |
| Abnormal extension | 2 | |
| None | 1 | |
| Total | 3–15 |
In the older, awake child a complete mental status exam can be performed. This must be adjusted for age (see Table 55-2) but should include assessment of language (fluency and comprehension): the ability to name, repeat, write, read, and respond to written commands. Simple mathematical problems should be adjusted to the child’s age-dependent ability. Praxis can be assessed quickly even in the PICU by demonstration of learned behaviors, even in the young child (brush your teeth, brush your hair). Other components of the mental status exam, including memory, fund of knowledge, and reasoning can be assessed by holding a conversation with the patient.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree