21 Pediatric Gynecologic Disorders
• Prepubertal girls have thin, sensitive vaginal mucosa that is easily irritated.
• If speculum examination is necessary in a young girl, examination under anesthesia should be considered.
• Parents of young girls taken to the emergency department because of gynecologic complaints are often worried about the possibility of sexual abuse but may not verbalize their concern until appropriate questions are asked.
• Most pediatric gynecologic complaints are not related to abuse.
• Most sexually abused children have no abnormalities on examination.
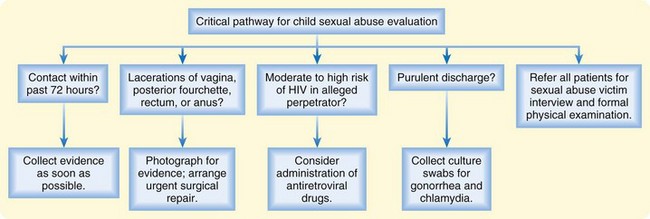
• Emergency department evaluation of possible sexual abuse should focus on identification of patients who require urgent treatment, urgent collection of evidence, or protective custody.
Pathophysiology
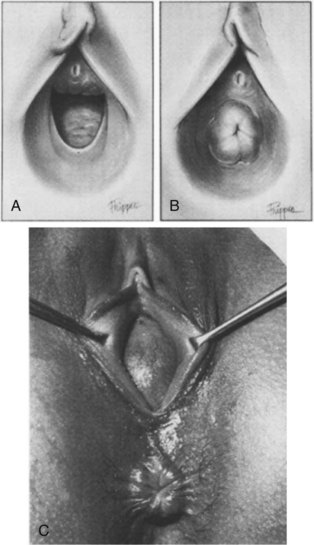
Pediatric gynecologic problems differ from those of adult women chiefly because the vaginal mucosa is thin, dry, and easily irritated in the absence of estrogen. This makes prepubertal girls more sensitive to a variety of chemical, physical, and microbiologic irritants. The normal hymen looks thin, with an average opening of about 4 mm. However, there is great variability in normal hymenal shape, ranging from imperforate to multiple small fenestrations to oval, round, or stellate openings (Fig. 21.1). Abnormal findings that may correlate with vaginal penetration include lacerations of the hymen or a thickened hymen with rolled edges. These findings are extremely difficult to differentiate from normal variations, and photos should always be taken if sexual abuse is suspected. Neonates have swollen labia and thick, moist vaginal epithelium for several weeks after birth, but most prepubertal girls have smooth pink vaginal mucosa and a pale vulva that barely covers the clitoris.
Presenting Signs and Symptoms
The chief complaints of children with gynecologic problems include vaginal discharge or bleeding, itching or rubbing of the genitals, dysuria or refusal to void, or a foul genital odor noted by caregivers. The initial differential diagnosis can be guided by the predominant complaints (Box 21.1).
Tips and Tricks
Promoting Body Safety While Accomplishing the Necessary Genital Examination
State to the child that you are a doctor or nurse.
Perform the nonthreatening aspects of the physical examination first (listen to the heart and palpate the abdomen).
Review and respect privacy and safe-touching rules.
Stand back and let the parent or other caregiver help the child with undressing.
Sexual Abuse
ED evaluation of possible sexual abuse should focus on identifying patients who require urgent treatment, urgent collection of evidence, or protective custody (Fig. 21.2). Open-ended questions by the emergency practitioner (EP) will allow the parents to voice their concerns about possible molestation (this should be done away from the child). When interviewing the patient, history taking should be limited to open-ended questions phrased in child-appropriate language, such as “How did you get this ouchie?” Do not make suggestions that the child may follow in an attempt to please. Do not direct, lead, or ask questions with embedded information because such information can appear in the child’s later responses. Formal interviewing and complete examination are best minimized in the ED and instead carried out by trained personnel. ED providers should be aware of local resources and if possible refer children to a designated child sexual abuse evaluation center.
If abuse is alleged within the past 72 hours, collection of evidence should be undertaken as soon as possible. In studies of forensic evidence collection in prepubertal sexual assault cases, the majority of usable evidence is found on clothing and linen. In one large study of prepubertal sexual assault victims, no swabs were positive for blood after 13 hours or for semen or sperm after 9 hours.1