49 Patient-Ventilator Interaction
The clinical management of patients with acute respiratory failure is based on the assumption that significant abnormalities in respiratory mechanics, respiratory muscle performance, and control of breathing are the underlying mechanisms responsible for acute respiratory failure.1 The effects of mechanical ventilation on gas exchange, respiratory muscle load, and dyspnea depend on the matching between the ventilator settings and the patient’s respiratory physiology. However, mechanical ventilation is rarely optimized, which would require that ventilator settings be based on accurate and reproducible measurements of lung and chest wall mechanics, respiratory muscle function, and respiratory drive.2–5
 Respiratory Physiology
Respiratory Physiology
The goal of the intrinsic ventilatory control system is to integrate the timing and intensity of the phrenic nerve signal, inputs from chemoreceptors and pulmonary stretch receptors, and variations in metabolic demands. Contraction of the respiratory muscles leads to the generation of flow and volume to provide adequate alveolar ventilation with minimal work of breathing.6 During spontaneous breathing,7 the respiratory muscles generate pressure (Pmus) to generate flow against the resistive properties (RRS) and volume against the elastic properties (ERS) of the respiratory system to eventually overcome intrinsic positive end-expiratory pressure (PEEPi). Under these circumstances, the act of spontaneous breathing can be described at any instant as follows:
where Pres represents the resistive pressure and is a function of flow (Pres = Flow × RRS), and Pel represents the elastic recoil pressure and is a function of volume (Pel = Volume × ERS). Assuming that RRS and ERS are linear, the equation becomes:
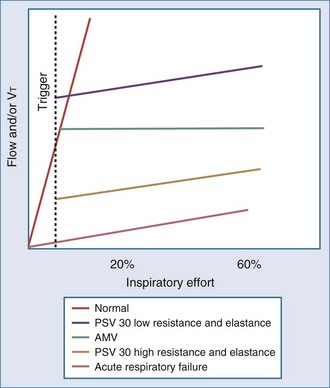
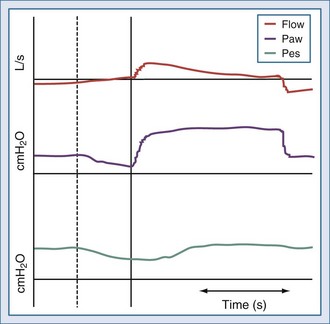
The complex interaction among all the variables in equation 3 can be summarized by the concept of neuroventilatory coupling (Figure 49-1).8 Under normal conditions, as well as at the onset of acute respiratory failure, the spontaneous contraction of the respiratory muscles suddenly generates flow and volume; the slope of the relationship between effort and ventilatory output is conditioned by the contractile properties of the respiratory muscles and the impedance of the respiratory system. When positive pressure is applied to assist the action of breathing in most common modes of mechanical ventilation (pressure-support or pressure-assist mandatory ventilation), the coupling between effort and output is compromised. During assist-control ventilation, flow and volume remain constant despite changes in muscle contraction; during pressure-support ventilation, despite coupling between inspiratory effort and ventilatory output, any increase in respiratory impedance decreases the amount of delivered flow and volume.8 During noninvasive ventilation (NIV), air leaks may further compromise the coupling between patient effort and ventilatory output.9
 Patient and Ventilator Variables
Patient and Ventilator Variables
Patient Variables
The patient interacts with the ventilator based on three physiologic variables2,10,11:
Ventilator Variables
Three phase variables define inspiration13,14:
Features of ventilators such as blowers and inspiratory, expiratory, and positive end-expiratory pressure (PEEP) valves are also important in determining the interaction between patient and ventilator.23–26
Total Ventilator-Controlled Mechanical Support
In this mode, the patient’s breathing pattern is totally controlled by the ventilator. The pressure generated by the respiratory muscles is abolished by paralysis or sedation. Flow, volume, and pressure are imposed by the ventilator, and the patient’s breathing pattern is totally replaced by that of the ventilator. The risk of patient-ventilator asynchrony is therefore abolished, but there are potential risks associated with sedation and paralysis,27 respiratory muscle atrophy,28 lung damage due to overdistention,29 patient discomfort,30 and difficulty weaning after prolonged controlled mechanical ventilation.1
Partial Patient-Controlled Mechanical Support
With this mode, spontaneous breathing activity is partially preserved.31 The need for sedation and paralysis may be reduced, disuse atrophy of the respiratory muscles may be minimized, and the weaning process may be accelerated, provided the patient’s ventilatory demand and ventilator settings are synchronized.32 The ability to restore gas exchange, unload respiratory muscles, and relieve patient dyspnea with partial patient-controlled mechanical support therefore depends on the absence of patient-ventilator asynchrony.33
Although there are no well-accepted definitions, patient-ventilator asynchrony is common; it is often unrecognized, underestimated, and inappropriately treated.3–5,22,33–35 The cause of patient-ventilator asynchrony can be described as occurring because of a mismatch between the three physiologic variables characterizing spontaneous breathing (ventilatory drive, ventilatory requirements, and duration and ratio of inspiratory time to total breath cycle duration) and the three technologic variables characterizing ventilator function (trigger function, gas delivery algorithm, and cycling criteria).
 Respiratory Drive–Ventilator Trigger Asynchrony
Respiratory Drive–Ventilator Trigger Asynchrony
During partial ventilatory assistance (assisted breath), the inspiratory synchronization system (inspiratory trigger) detects any patient inspiratory effort and activates a mechanical act. Therefore, inspiratory effort is tracked in order to couple the patient’s effort with the delivery of pressure, flow, or volume. The goal of a good inspiratory trigger is to reduce as much as possible the duration and intensity of the muscular effort that comes before mechanical support, while avoiding autotrigger effects.36 Auto-triggering can be defined as a mandatory breath not following a patient’s inspiratory effort.
It has been suggested that a trigger (independently of its algorithm) must have a response time less than 100 ms. However, the inspiratory effort necessary to trigger a breath may be a significant part of the total inspiratory effort, representing 17% and 12% of the total inspiratory effort during pressure and flow triggering, respectively.15–23,34,35 Aslanian and coworkers found that even though the time required for triggering was 43% shorter, and effort during the time of triggering was 62% less with flow triggering than with pressure triggering, effort during the post-triggering phase was equivalent for both pressure and flow triggering.37 The clinical benefit of flow triggering therefore appears to be much less relevant than commonly stated.3
Inspiratory phase asynchrony may be due to problems with inspiratory triggering, and this can be correlated with respiratory drive. Phase lag quantifies the delay between the commencement of inspiratory muscle activity and the beginning of mechanical inflation (Figure 49-2).3,10,11 The presence of a threshold load, such as dynamic intrinsic PEEP, may further complicate patient-ventilator interaction during the triggering phase.15 Giuliani et al. suggested that effort during triggering determines patient effort during the remaining portion of inspiration.38 Leung and coworkers demonstrated that the higher the level of ventilator-applied pressure, the lower the respiratory drive, but the longer the time required to trigger the ventilator. As a result, respiratory muscles generate smaller inspiratory swings in intrathoracic pressure but over a longer inspiratory time.2 Another problem is related to the fact that pressure is mostly detected inside the ventilator; therefore, any resistive load (e.g., endotracheal tube or upper airways during noninvasive ventilation) reduces the responsiveness of the gas delivered by the ventilator in response to patient effort.22
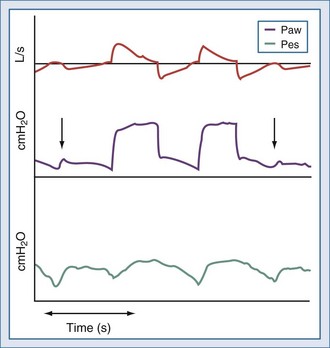
Ineffective triggering is due to the ventilator’s inability to detect the patient’s “request” for an assisted breath despite substantial inspiratory effort (Figure 49-3). This phenomenon usually occurs with high levels of ventilator assistance and short expiratory times. Mechanical characteristics that may induce ineffective triggering include low elastance, high resistance, and intrinsic PEEP; ineffective triggering is not correlated to an increase in the patient’s inspiratory effort.2 The application of external PEEP below the intrinsic PEEP level can reduce the inspiratory effort required to trigger the ventilator.39 Parthasarathy and coworkers demonstrated that prolonging mechanical inflation into neural expiration reduces the time available for unopposed exhalation, resulting in the need for a greater inspiratory effort to trigger the ventilator.40 Younes and colleagues found that ineffective triggering in ventilator-dependent patients exacerbates dynamic hyperinflation.41
New trigger algorithms aim at improving patient-ventilator interaction during sudden changes in flow or respiratory rate or in the presence of air leaks during NIV. This can be achieved with volume triggers, triggers linked to flow waveform algorithms, combining pressure and flow signals in the same trigger algorithm, or using both pressure and flow triggers. However, all inspiratory trigger drawbacks may be overcome by using a neural trigger obtained by means of a dedicated nasogastric tube with a multiple array of electrodes placed in the distal esophageal portion.8,42,43
 Ventilatory Requirement–Gas Delivery Asynchrony
Ventilatory Requirement–Gas Delivery Asynchrony
Gas delivery asynchrony occurs when ventilator-delivered flow, volume, and pressure are insufficient to meet the patient’s ventilatory demand. Ward and coworkers demonstrated that increasing the flow rate could be used as a means of reducing the patient’s respiratory drive and active respiratory muscle work,17 although doing so may exert an excitatory effect on respiratory rate and on the rate of rise of inspiratory muscle activity.3,20,21,44–50 Laghi and colleagues demonstrated that the imposed inspiratory time during mechanical ventilation determines respiratory frequency independent of inspiratory flow and tidal volume.20 Pressure-targeted breaths may better match the patient’s ventilatory requirements, because flow is the dependent variable during constant pressure delivery. In addition, rapid pressurization of the airways is coupled with high inspiratory flow only at the beginning of inspiration, thus reproducing the physiologic flow profile.51 However, during a pressure-targeted breath, the pressure-rise time setting—the time taken to reach the pressure set on the ventilator—may influence patient-ventilator interaction because its modification determines the dependent flow output.13,14
 Inspiratory Time–Ventilator Cycling Asynchrony
Inspiratory Time–Ventilator Cycling Asynchrony
A breath can be pressure-, time-, volume-, or flow-cycled.14 Ventilator-patient asynchrony occurs when the patient is trying to exhale, but the ventilator is still delivering gas.37,40,52 In patients ventilated with a time-cycled breath, expiratory phase asynchrony takes place when the patient’s neural inspiratory time is shorter or longer than the ventilator inflation time. For proper cycling off the ventilator and optimal patient-ventilator synchrony, the patient’s inspiratory flow and ratio of inspiratory time–to–total breath cycle duration must be tracked.
During flow-cycled breaths, inspiratory time is determined exclusively by the time taken for the exponentially declining flow to reach the flow threshold value (when cycling between inspiration and expiration occurs).34,53 As a consequence, a flow-cycled ventilation mode (e.g., pressure-support ventilation [PSV]) is cycled when inspiratory flow decay reaches a given threshold value. The inspiratory flow threshold value, also called expiratory trigger, thus controls the inspiration-to-expiration switch in these modalities.13,54 The aim is to detect the very end of patient inspiration through inspiratory flow measurement. The goal of these ventilatory modes is to optimize synchronization between spontaneous patient inspiratory time and ventilator inspiratory time. However, for proper cycling off and optimal patient-ventilator synchrony, the ventilator always has to track the patient’s inspiratory flow.40,55,56
 Patient-Ventilator Asynchrony During Pressure-Support Ventilation
Patient-Ventilator Asynchrony During Pressure-Support Ventilation
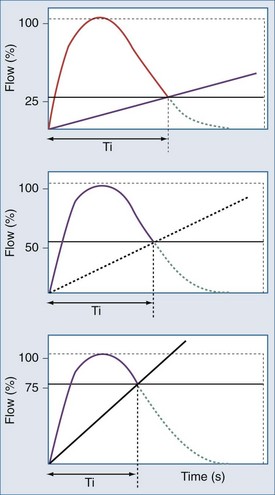
(1) The expiratory trigger sensitivity can be fixed (default at 25% of peak flow ) or can vary from 5% to 90% or from 5 to 25 L/min (Figure 49-4).57 It can also be linked to algorithms where there is a ranking logic of expiratory cycling criteria that links cycling to expiration. Setting the expiratory trigger at a higher percentage of peak inspiratory flow (i.e., 50% to 70% of decay of peak inspiratory flow) in patients with obstructive pulmonary disease improves patient-ventilator synchrony and reduces inspiratory muscle effort.58
In addition, the modification of cycling-off criteria may have a beneficial effect on reducing the dynamic hyperinflation and inspiratory effort in chronic obstructive pulmonary disease patients, especially at low levels of pressure support.59
The proper adjustment of expiratory trigger threshold may be also important in improving patient-ventilator synchrony and in decreasing the work of breathing during acute lung injury. Unlike in obstructive pulmonary disease, setting the lower threshold at 5% of the peak inspiratory flow might be the optimal value for patients with acute respiratory distress syndrome or acute lung injury.60
Chiumello et al. found in patients recovering from acute lung injury during PSV at 15 cm H2O, the lowest cycling-off criteria reduced the respiratory rate and increased the tidal volume without modifying the work of breathing.61
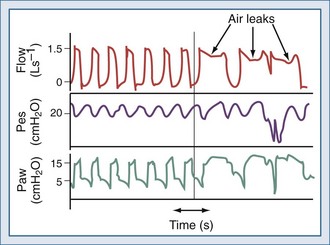
The expiratory sensitivity setting is crucial when ventilators are used to deliver NIV, because air leaks may cause an abnormal prolongation of the inspiratory time; during this time, the patient may make efforts to exhale against the machine or to inhale, without receiving any ventilatory support (inspiratory hang-up) (Figure 49-5).62–66 In addition, leak-compensating capabilities differ markedly between ventilators.56,67
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree