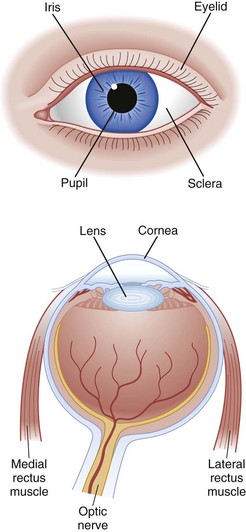
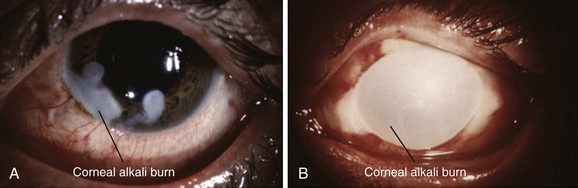
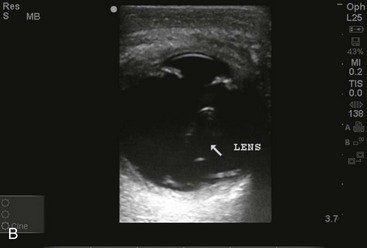
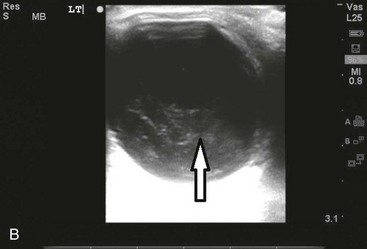
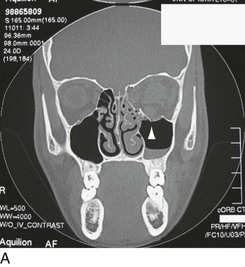
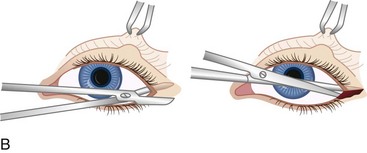
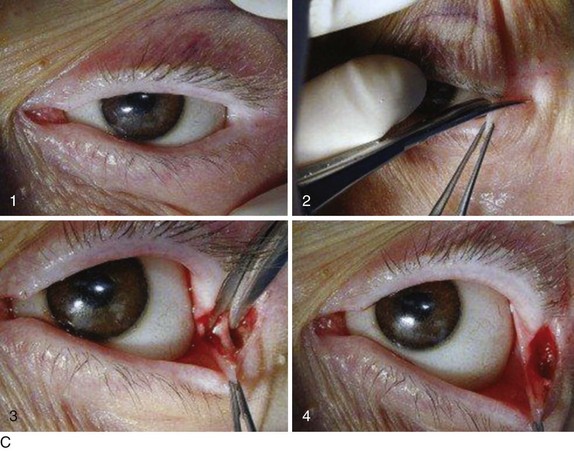
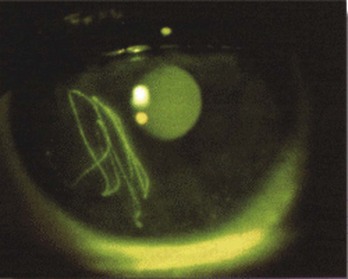
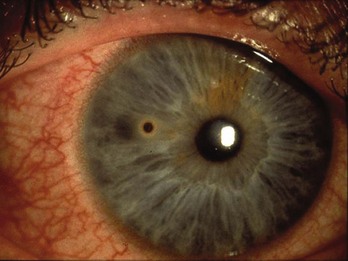
Chapter 71 Two percent of emergency department (ED) patients have eye complaints, including primary ophthalmologic pathology, infectious problems, and traumatic injuries. Eye injuries account for 3.5% of all occupational injuries in the United States, and about 2000 U.S. workers injure their eyes each day.1 The majority of eye complaints can be treated without ophthalmologic consultation, but a few require the involvement of a specialist as well as immediate action. Some specific problems, such as central retinal artery occlusion and caustic exposure, require emergent therapy, even as assessment proceeds. Eye emergencies can be categorized into three main categories, including the red eye, the painful eye, and visual loss. Figures 71-1 and 71-2 are provided as brief reviews of normal ocular anatomy and funduscopic appearance. Approximately 3% of all visits to the ED are a result of eye trauma.2 A systematic evaluation of the periorbital and orbital structures aids in the evaluation of patients with ocular trauma. Many extraocular structures are found in close proximity, and concomitant, nonocular injury is common. Clinical Features and Management: Contusion.: Blunt injury to the orbits and surrounding tissues results in ecchymosis, swelling, and an often dramatic appearance. Related significant injury should be considered. Basilar skull fractures may occur with bilateral ecchymosis (raccoon eyes). Underlying globe injury may be present, and complete examination may be impeded by swelling. The emergency physician should attempt to visualize and examine all structures underlying the eyelids and obtain an accurate determination of visual acuity. This should be done soon after the patient arrives, before further swelling occurs. Examining the structures underlying severely swollen eyelids is difficult. A Desmarres retractor may help avoid global pressure. An orbital computed tomography (CT) scan is indicated if examination of the underlying structures is not possible owing to severe swelling. Orbital Wall Fractures.: An orbital wall fracture is suspected when a patient has soft tissue swelling and trauma to the globe. When blunt force causes an acute rise in intraorbital pressure, the thin walls of the orbit frequently fracture. Prolapse of orbital soft tissues into the maxillary sinus may result because the orbital floor is generally the weakest point. Entrapment of the inferior rectus and inferior oblique ocular muscles, orbital fat, and connective tissues results in enophthalmos, ptosis, diplopia, anesthesia of the ipsilateral cheek and upper lip, and limitation of upward gaze. Subcutaneous orbital emphysema may be palpable. Associated globe injuries occur in 10 to 25% of patients with orbital floor fractures.3 Plain radiographic examination of the face can help but is imperfect. A CT scan of the orbits with axial and coronal views is preferred (Fig. 71-3A). Plain x-ray films have limited utility given the lower sensitivity to delineate soft tissue structures and extent of bony deformity. On x-ray film, the teardrop sign, a bulge extending from the orbit into the maxillary sinus, and an air-fluid level in the maxillary sinus are indirect signs of orbital floor injury. The use of bedside ultrasound has also been shown to be useful in the identification of orbital wall fractures.4 If the fracture involves an infected sinus, treatment consists of nasal decongestants such as pseudoephedrine 30 mg every 6 hours, broad-spectrum oral antibiotics such as amoxicillin clavulanate 875 mg bid for 10 days, and ice packs to the orbit for 48 hours. Some ophthalmologists use steroids to reduce swelling. Surgical repair is performed only for persistent diplopia or to address cosmetic concerns and generally not until swelling subsides in 7 to 10 days. Patients can usually be discharged to be reevaluated by an ophthalmologist in 1 to 2 weeks. Figure 71-3 A, Facial computed tomography scan showing left inferior orbital fracture with blood in maxillary sinus. B, Lateral canthotomy. C, (1) Preoperative view of orbit. (2) Incision for lateral canthotomy. (3) Identification and incision of inferior canthal tendon, completing cantholysis. (4) View after lateral canthotomy and inferior cantholysis, creating maximal immediate decompression by allowing eyeball and orbital contents to move anteriorly. (A, Courtesy University of Iowa Department of Ophthalmology, http://webeye.ophth.uiowa.edu/eyeforum/Images/floorfx_08232004.jpg. C, From Ramakrishnan VR, Palmer JN: Prevention and management of orbital hematoma. Otolaryngol Clin North Am 43:789-800, 2010.) Medial orbital wall fractures, through the lamina papyracea of the ethmoid bone, involve entry into the ethmoid sinus. Clinical features include orbital emphysema and epistaxis. Diplopia from medial rectus impingement can occur. The finding of orbital emphysema prompts a search for associated injury. Rarely is orbital emphysema significant enough to compress the optic nerve and result in acute visual loss. In most cases, orbital emphysema is a benign finding that resolves with time. Prophylactic antibiotics are not needed unless the fracture involves an infected sinus.5 Retrobulbar Hemorrhage.: Orbital hemorrhage in the potential space surrounding the globe may occur after blunt trauma and injury to the orbital vessels. Significant hemorrhage results in an acute rise in intraorbital pressure that is transmitted to the globe and optic nerve. This may result in occlusion of the central retinal artery and optic nerve ischemia. Clinical findings include proptosis, limitation of ocular movement, visual loss, and increased intraocular pressure. An orbital CT scan demonstrates a hematoma; however, treatment should not be delayed by waiting for imaging to be performed. When a retrobulbar hematoma compromises retinal circulation, immediate ophthalmologic consultation for decompression is warranted. Treatment of increased intraocular pressure includes a carbonic anhydrase inhibitor, a topical beta-blocker, and 1 to 2 g of intravenous mannitol per kilogram. A lateral canthotomy can be performed in the ED as a temporizing measure before definitive decompression6 (see Fig. 71-3B and C). Clinical Features and Management: Chemical Burns.: Exposure of the eye to chemicals is a true ocular emergency. Exposure to strong alkaline chemicals, found in drain cleaners, in chemical detergents, in industrial solvents, and as lime in plaster and concrete, produces a liquefactive necrosis that penetrates and dissolves tissues until the alkaline agent is removed. Acid burns tend to be less devastating than alkali burns because acidic exposure causes coagulation necrosis and the precipitation of tissue proteins limits the depth of the injury. Treatment should begin at the scene with immediate irrigation with copious amounts of water continued for at least 30 minutes before transport. Any particulate matter should be removed from the fornices with a cotton swab. On hospital arrival, irrigation should continue. There is evidence that buffered eye wash solutions might be significantly better for irrigation of ocular caustic injuries than standard intravenous solutions. There are human case series reports demonstrating that an amphoteric, hypertonic chelating solution, Diphoterine (Prevor, Valmondois, France), provides faster correction of pH as well as improved outcomes.7,8 Cederroth Eye Wash (Cederroth Industrial Products, Upplands Vasby, Sweden) is a borate-based buffering solution that has demonstrated faster pH correction in exposed eyes in an animal model.9 Use of irrigation devices, such as a Morgan Lens (MorTan, Missoula, Mont.), can assist in delivering continuous irrigation to the affected eye. Topical anesthetics and manual lid retraction may be needed for proper irrigation. Irrigation is needed until the pH of the tear film is neutral as tested with nitrazine paper dipped into the inferior conjunctival fornix. If the pH tested immediately after irrigation is still alkaline, irrigation is reinstituted and the pH checked again after 10 minutes and periodically thereafter. Treatment after irrigation consists of a cycloplegic (phenylephrine is avoided), topical antibiotics such as 0.5% erythromycin eye ointment applied every 4 to 6 hours to the affected eye, and pain management. Intraocular pressure should also be measured because high intraocular spikes in pressures can be seen immediately after an alkali burn.10 Ophthalmologic consultation is indicated in all significant chemical exposures. Identification of the substance and its pH value is important. In general, alkaline substances with a pH less than 12 and acidic substances with a pH greater than 2 do not cause significant injury, although high concentration and prolonged contact time can alter this general rule (Fig. 71-4). Miscellaneous Irritants, Solvents, Detergents, and Glues.: Unknown exposures are best treated as though they were from an alkali or acid substance, prompting immediate irrigation. Detergents generally cause conjunctival irritation only. More irritating substances may denude the corneal epithelium and cause anterior chamber inflammation. After copious irrigation, these injuries are treated as corneal abrasions. Super Glue (cyanoacrylate adhesive) exposure is also common. Cyanoacrylate adhesive is used in many industrial and domestic settings but is considered to have relatively little toxicity.11 These glues harden rapidly, and typically the eyelids are sealed shut. Misdirected lashes and the hardened glue may act as foreign bodies and cause corneal defects. Gentle traction on the eyelids and separation of glued eyelashes may open the eyelids. If the eyelids are sealed shut in a normal anatomic position and cannot be opened with gentle traction, the eye may be left alone, allowing time for the glue to dissolve by physiologic mechanisms over several days. If the eyelids are inverted and sealed shut, surgical intervention may be needed. Attempts to dissolve the glue with other substances should be avoided. Ophthalmic consultation and arrangements for follow-up are recommended for Super Glue exposures. Thermal Burns.: Thermal burns affect the eyelids more than the globe because of reflex blinking and Bell’s phenomenon. Superficial eyelid burns can be treated by copious irrigation, application of a cold compress to decrease the thermal injury, and topical antibiotic ophthalmic ointment. Second- or third-degree eyelid burns require ophthalmic consultation. Hot liquid splashes and cigarette ashes to the cornea usually result in a superficial corneal epithelial injury and are treated as corneal abrasions. Molten metals and other hot objects may result in globe perforation. The severity of the burn is related to the duration of exposure as well as the nature of the causative agent. Radiation Burns (Ultraviolet Keratitis).: Ultraviolet light from sun lamps, tanning booths, high-altitude environments, snow or water reflection, or a welder’s arc results in direct corneal epithelial damage. After a latent period of 6 to 10 hours, patients develop a foreign body sensation, tearing, intense pain, photophobia, and blepharospasm. Topical ophthalmic anesthetics facilitate physical examination. Examination reveals decreased visual acuity, injected conjunctiva, and diffuse punctate corneal lesions, often with a discrete lower border defining the cornea protected by the inferior lid. Treatment consists of a short-acting cycloplegic and a topical broad-spectrum antibiotic ointment, although evidence for the latter is scant. Oral opioids are commonly needed. Patients should also not routinely be prescribed traditional topical anesthetics because use has been shown to inhibit the migration of corneal epithelial cells, resulting in severe corneal scarring and keratopathy.12 One recent study demonstrated that dilute proparacaine 0.05% can be used as an analgesic for acute corneal injuries; however, this study enrolled a small number of patients and was not powered for safety outcomes.13 Patients should be counseled on the adverse effects of ultraviolet radiation, and education provided regarding the use of various protective devices. Ophthalmologic follow-up in 24 hours is recommended if symptoms have not resolved. Biologic Exposures.: Exposure of the eye to any human blood or body fluid (e.g., semen, urine, saliva) may result in infection with a blood-borne pathogen. The risk of infection through mucous membrane exposure (e.g., conjunctiva) is less than that via a needle-stick and is dependent on the volume and concentration (e.g., viral load) of the body fluid. Copious irrigation of the affected eye is begun immediately after the exposure; the immunization status of the patient and, if known, the source patient should be determined. Postexposure prophylaxis should be discussed with the patient and arrangements made for follow-up with occupational health or the patient’s primary care provider. Mechanical Corneal Abrasions.: Patients with a corneal abrasion may complain of a foreign body sensation, pain, photophobia, and decrease in visual acuity. The degree of relief afforded by topical anesthesia can differentiate corneal injury from other causes of acute eye pain.14 Physical examination reveals injected conjunctiva, decreased visual acuity if the defect is large or lies in the visual axis, and demonstration of the epithelial defect with slit-lamp examination and fluorescein (Fig. 71-5). Aqueous humor leaking from the anterior chamber during fluorescein examination (Seidel’s test) suggests a corneal perforation. Multiple vertical abrasions suggest a foreign body, and a thorough examination of the area under the eyelid should be performed. Treatment consists of cycloplegia and topical antibiotics. There is evidence that treatment with topical nonsteroidal anti-inflammatory medications, ketorolac 0.5% four times daily, or diclofenac 0.1% four times daily reduces the pain associated with corneal abrasions, and therefore these medications are adjuvant therapy for patients with traumatic corneal abrasions.15 Patients with contact lenses should be treated with topical antibiotics with pseudomonal coverage such as tobramycin 0.5% solution 1 or 2 drops every 4 hours to the affected eye.16 Eye patching, especially with injuries involving vegetable matter or contact lens use, is avoided. A 2006 Cochrane review concluded that use of an eye patch does not improve healing rates and does not reduce pain for simple corneal abrasions and is not recommended for routine use.17 Patients with corneal abrasions should not wear their contact lenses. Oral pain medications may be needed. There are no known cases of clinical tetanus developing from a simple corneal abrasion18; however, updating a patient’s tetanus immunization status is part of emergency care and should be considered in any tetanus-prone injury such as corneal perforation or injuries containing dirt and organic matter. Figure 71-5 Corneal abrasion demonstrated by slit-lamp examination. (Image courtesy http://www.perret-optic.ch/optometrie/symptomes_diagnostiques/symptomes/opto_symfor_gb.htm#abrasion.) Corneal Foreign Bodies.: Patients with corneal foreign bodies experience pain, foreign body sensation, injected conjunctiva, tearing, and blepharospasm. Administration of a topical ophthalmic anesthetic facilitates physical examination. Diagnosis may be facilitated by use of a slit lamp (Fig. 71-6). After a topical anesthetic is applied, the initial attempt at removing corneal foreign bodies is made with a stream of sterile saline solution. Alternatively, a moistened cotton-tipped applicator can be used to gently roll over the foreign body and lift it off the corneal surface. If this fails, an attempt can be made to remove the foreign body through use of a 25-gauge needle with a 1- to 3-mL syringe as a handle and magnification, generally the slit lamp. The patient should be totally cooperative, with his or her head firmly stabilized within the slit lamp. Alternatively, a short plastic 20-gauge catheter can be placed on a syringe, and with slit-lamp visualization the foreign body can sometimes be irrigated out of the cornea. Figure 71-6 Corneal foreign body seen on slit-lamp examination. (Image courtesy www.tedmontgomery.com.) Iron-containing corneal foreign bodies leave a residual rust ring (Fig. 71-7). Removal of the rust ring is best left to the ophthalmologist or for a return visit to the ED in 24 hours, because the affected cornea gradually softens and the rust migrates toward the corneal surface, making removal easier. Figure 71-7 Corneal rust ring after removal of iron-containing foreign body demonstrated by slit-lamp examination. (Image courtesy www.tedmontgomery.com.) Use of high-speed drills, saws, grinders, and pounding objects and involvement in explosions are risk factors for perforation. Any concern for ocular perforation warrants immediate ophthalmologic consultation. If there is no evidence of ocular penetration on a thorough ophthalmic examination, then imaging is not required. If there is any evidence or concern for ocular penetration and a metallic foreign body is visualized, plain-film radiographs can be used to ensure that multiple intraocular foreign bodies are not present. CT scan is used if there is suspected ocular penetration but an intraocular foreign body is not visualized on plain-film radiographs or if there are multiple intraocular foreign bodies. If a nonopaque foreign body is suspected after CT imaging, the clinician may consider ultrasound or magnetic resonance imaging (MRI).19 Conjunctival Foreign Body.: Conjunctival foreign bodies can be removed under topical anesthesia with a cotton-tipped applicator or fine forceps. Topical phenylephrine can be used to reduce the conjunctival bleeding. Subconjunctival Hemorrhage.: Rupture of small subconjunctival blood vessels is common and occurs as a result of trauma or the Valsalva maneuver or often without an identified cause. Pain, diminished visual acuity, or photophobia suggests a more serious pathologic condition. Subconjunctival hemorrhage is flat, bright red, smooth, limited to the bulbar conjunctiva, and sharply demarcated at the limbus (Fig. 71-8). If there is a history of blunt or penetrating trauma, a thorough examination is indicated to exclude an underlying scleral penetration. Subconjunctival hemorrhage should be distinguished from bloody chemosis, which is indicative of more serious globe pathology. Bilateral or recurrent subconjunctival hemorrhage may require workup for bleeding diathesis. Treatment consists of local cold compresses for 24 hours, with resolution in 2 to 3 weeks. Clinical Features and Management: Traumatic Hyphema.: Disruption of blood vessels in the iris or ciliary body results in a hyphema, blood in the clear aqueous humor in the anterior chamber. If the patient is sitting, the blood often layers and forms a meniscus with the aqueous humor. Hyphemas range from minimal blood seen only with the slit lamp to the “eight ball” or a total hyphema with blood that has clotted (Fig. 71-9). Patients report pain, photophobia, and decreased visual acuity. Intraocular pressure is elevated in approximately 27% of patients acutely but is usually mild and is self-limited. Pressures greater than 35 mm Hg with durations greater than 5 to 14 days are more likely to be associated with optic atrophy.20 Hyphemas are usually not associated with an afferent pupillary defect (or Marcus Gunn pupil). An afferent pupillary defect occurs when the abnormal eye paradoxically dilates rather than constricts when light is directed to that eye during the swinging flashlight test. If the hyphema is large enough to result in increased intraocular pressure, an afferent pupillary defect may be seen. Management of hyphema is individualized for a given patient. Selected low-grade hyphemas in reliable patients may be managed on an outpatient basis. Patients with hyphemas greater than 50%, decreased vision, increased intraocular pressure, and sickle cell disease are candidates for admission. Interventions such as elevating the bed 30 to 45 degrees, bed rest, and eye protection with an eye shield have been recommended in the past for the management of hyphema. However, a recent Cochrane review showed that the beneficial effect of these interventions is still unclear and evidence is inconclusive owing to the small number of studies and participants.21 Analgesics are appropriate, but the patient should avoid taking aspirin and other platelet inhibitors. Antiemetics and sedatives should be used cautiously. Increased intraocular pressure occurs as a result of aqueous flow blockage from the blood present. In patients without sickle cell disease, initial treatment is a topical beta-blocker; a topical alpha-agonist or topical carbonic anhydrase inhibitor is added if needed. Oral acetazolamide 20 mg/kg/day in four divided doses or 1.5 g/kg of intravenous mannitol every 8 hours may also be used. There is limited evidence regarding the benefit of cycloplegics and steroids; thus their use varies depending on the specific clinical situation and is best left to the ophthalmologist. Antifibrinolytics, such as aminocaproic acid, also may be considered in the treatment of traumatic hyphema. Both systemic and topical aminocaproic acid reduce the rate of recurrent bleeding but do not affect final visual acuity.21 Failure of medical therapy to control high intraocular pressure, failure of a large clot to resolve, and corneal blood staining are indications for surgical intervention. The major complication of hyphema is rebleeding, which occurs after 2 to 5 days when the initial clot retracts and loosens. The reported incidence of rebleeding is 6% to 33%.22,23 Rebleeding is more common in those with visual acuities of 20/200, initial hyphema covering more than one third of the anterior chamber, medical attention delayed more than 1 day after injury, and elevated intraocular pressure at the initial examination. Other complications include corneal blood staining, acute or chronic glaucoma, and anterior or posterior synechia formation. Traumatic Iridocyclitis (Uveitis).: Blunt injury of the globe may contuse and inflame the iris and ciliary body, resulting in ciliary spasm. Patients report photophobia and deep, aching eye pain. Examination reveals perilimbal conjunctival injection (ciliary flush), cells (white or red blood cells) and flare (protein content) in the anterior chamber, and a small, poorly dilating pupil (Fig. 71-10A). Patients may also experience direct photophobia when the light is directed to the affected eye and consensual photophobia when light is directed to the uninvolved eye. Traumatic Mydriasis and Miosis.: Blunt injury may result in either pupillary dilation or constriction and may persist for days. For significant head trauma and altered mental status, a cranial nerve palsy should be ruled out before pupillary mydriasis is ascribed to local contusion. Iridodialysis.: Traumatic iridodialysis is a tearing of the iris root from the ciliary body, leading to the formation of a “secondary pupil.” This injury is often the cause of a hyphema. If no associated hyphema is present, no specific ED treatment is needed. Large tears can lead to monocular diplopia and may require surgical correction. Immediate ophthalmologic consultation is warranted when iridodialysis has caused a hyphema or a decrease in visual acuity. Clinical Features and Management: Cataract.: If the lens capsule is disrupted by either blunt or penetrating trauma, the relatively dehydrated stroma absorbs fluid, swells, and becomes cloudy. Acute glaucoma may develop from blockage of the aqueous humor flow through the pupil, necessitating surgical intervention. Bilateral cataract formation may also develop after electrical injury or lightning injury. In less severe injury, cataract formation may occur over weeks to months. Definitive treatment of cataract is lens replacement. Lens Subluxation and Dislocation.: Complete disruption of the lens zonule fibers by blunt trauma may result in anterior or posterior dislocation of the lens (see Fig. 71-10B). Incomplete disruption of the lens zonule fibers results in subluxation of the lens. Lens dislocation may occur with minor trauma in patients with Marfan syndrome, homocystinuria, tertiary syphilis, and other predisposing conditions. Patients report monocular diplopia or visual distortion with subluxation and marked visual blurring with dislocation. Examination reveals decreased visual acuity. The edge of a subluxated lens can be seen when the pupil is dilated. Iridodonesis is a trembling or shimmering of the iris after rapid eye movements and is a helpful sign of lens dislocation. Secondary glaucoma can also result after traumatic lens dislocation. The dislocated lens can cause pupillary block by preventing the flow of aqueous humor from the posterior chamber through the pupil into the anterior chamber, resulting in increased intraocular pressure.24 Treatment ranges from observation to surgical removal and is dictated by the location of the dislocated lens and associated eye injury. Immediate ophthalmologic consultation is warranted. Scleral (Globe) Rupture.: Penetrating or blunt trauma to the eye can result in scleral rupture. Significant blunt force can result in globe compression with resultant globe rupture. Ruptures are most common at the insertions of the intraocular muscles or at the limbus, where the sclera is thinnest. The diagnosis of scleral rupture is obvious when intraocular contents are visualized; however, occult global rupture can be difficult to diagnose. Patients report eye pain and decreased vision. Examination may reveal a bloody chemosis or severe subconjunctival hemorrhage overlying the scleral rupture site. When the rupture occurs at the limbus, an irregularly shaped (teardrop) pupil may also be seen. Uveal prolapse through the scleral wound, appearing as a brownish black discoloration, can also be seen (Fig. 71-11A). Blunt globe injuries associated with an afferent pupillary defect, retinal detachment, poor initial visual acuity, or absence of a red reflex carry a poor prognosis with a higher rate of subsequent enucleation.25 Although a lower-than-normal intraocular pressure is a good indication of rupture, tonometry should not be performed in patients with suspected globe rupture. Any maneuvers that increase intraocular pressure need to be avoided. CT scan is increasingly being used to evaluate ocular trauma and possible globe rupture. However, CT has limited sensitivity and specificity (75% and 93%, respectively) in diagnosing open globe injuries. CT scan should be used as a complement to clinical findings (e.g., globe contour and volume loss) in diagnosing globe rupture.26 Theoretic classic teaching states that the use of succinylcholine is contraindicated in the presence of a penetrating ocular injury because of the rise in intraocular pressure and potential for ocular extrusion, but a search of the literature does not identify a single case report. One study reported on the use of succinylcholine after pretreatment with nondepolarizing agents in 100 patients with penetrating eye injury; no adverse events were found.27 Given the need for rapid airway management in a patient with penetrating ocular injury, rapid sequence intubation with succinylcholine and an induction agent is appropriate. Succinylcholine may be preceded by pretreatment with a defasciculating dose of a nondepolarizing neuromuscular blocking agent (e.g., 0.01 mg/kg of vecuronium or pancuronium), but there is no evidence that this improves outcome. Ophthalmologic consultation is required for all patients with suspected or proven globe rupture. Clinical Features and Management: Vitreous Hemorrhage.: Bleeding into the vitreous may occur from injuries to the retina and uveal tract and their associated vascular structures. Causes include diabetic retinopathy, posterior vitreous detachment, retinal vein occlusion, and trauma such as shaken baby syndrome in infants. Patients note decreased visual acuity and floaters. Floaters, described by the patient as dark dots or strands moving in the visual field in the direction of the preceding eye movement, are caused by vitreous blood. There is a diminished red reflex and an inability to visualize the fundus clearly with the direct ophthalmoscope (see Fig. 71-11B). Ocular ultrasound has shown to be an effective diagnostic tool in patients with vitreous hemorrhage and can help identify the cause.28 Treatment of vitreous hemorrhage includes elevating the head of the bed to allow settling of the blood and avoiding platelet-inhibiting drugs and the Valsalva maneuver. If the patient is receiving warfarin, the international normalized ratio (INR) should be checked. Ophthalmologic consultation is warranted for acute traumatic vitreous hemorrhage, and a vitrectomy is generally performed when the vitreous hemorrhage is associated with a retinal detachment. Retinal Injuries.: Blunt injury to the retina may result in hemorrhage, a tear or detachment, or commotio retinae. Hemorrhage can occur in the preretinal (subhyaloid), superficial retinal, or deep (subretinal) spaces. Preretinal hemorrhage appears as boat shaped, superficial retinal hemorrhage as flame shaped, and deep retinal hemorrhage as rounded and grape-purple in color. Tears and detachments from blunt trauma are common. Trauma is responsible for approximately 10% of all retinal detachments in the general population.2 Symptoms include floaters from bleeding, flashing lights from stimulation of retinal neurons, and visual field cuts or decreased visual acuity. Retinal tears or detachments do not cause pain. Examination may reveal the hazy gray membrane of the retina billowing forward (Fig. 71-12A), but many tears are peripherally located and not seen via direct ophthalmoscopy. Bedside ocular ultrasound can be a useful and rapid test in the detection of retinal detachment (Fig. 71-12B).29 Visual acuity may be normal unless the macula is involved. Indirect ophthalmoscopy is warranted if historical clues to the presence of retinal tears are present. Figure 71-12 A, Retinal detachment. Note large portion of retina billowing forward. B, Bedside emergency department ultrasound showing retinal detachment (white arrow). (A, Image courtesy www.tedmontgomery.com. B, Image courtesy Nicholas Connors, MD and Sophia Lin, MD, New York Presbyterian-Weill Cornell Medical Center.) Commotio retinae, also known as Berlin’s edema, occurs after ocular trauma. A study showed that it was present in approximately 6% of patients who had surgically treated orbital blowout fractures.30 Patients may have decreased visual acuity or may be asymptomatic. Examination reveals a cloudy whitening of the involved area that subsides in a few weeks with no specific treatment. Serial follow-up is necessary to ensure that retinal tear or detachment has not occurred. Optic Nerve Injury.: Significant blunt force to the orbital contents may avulse, transect, compress, or contuse the optic nerve. Fractures may extend into the orbital canal and cause optic nerve damage. Patients note visual field cuts or decreased visual acuity. Examination reveals an afferent pupillary defect, assorted visual field cuts, a decrease in visual acuity, or total blindness. The optic disk is normal initially, but pallor eventually develops. An orbital CT scan can help define the location and extent of injury. Management of traumatic optic neuropathy with steroids has been controversial. A 2011 Cochrane review looking at the use of steroids for traumatic optic neuropathy concluded that there is a high rate of spontaneous visual recovery in traumatic optic nerve damage and that steroids do not provide any additional benefit over observation.31 Surgical decompression may be considered when decreasing visual acuity is occurring from a known orbital canal fracture. However, this procedure should be considered on a case-by-case basis and the decision left to the ophthalmologist because there does not appear to be any clear evidence that surgical decompression of the optic nerve provides any additional benefit.32 Clinical Features and Management.: Any laceration involving the eyelids prompts a search for penetrating globe injury and, if indicated, a thorough search for a foreign body. The use of soft eye pads is avoided to prevent increases in intraocular pressure. 1. Lacerations involving the lid margins. 2. Lacerations involving the canalicular system (suspected in any laceration involving the medial eyelid area) (Fig. 71-13). 3. Lacerations involving the levator or canthal tendons. 4. Laceration through the orbital septum. Orbital fat protrudes through septal lacerations into the wound. Because eyelids have no subcutaneous fat, the appearance of fat in a lid laceration confirms this diagnosis. These wounds are associated with a high incidence of globe penetration and intraorbital foreign bodies. Clinical Features and Management.: Lacerations of the bulbar conjunctiva commonly involve intraocular foreign bodies or underlying scleral perforation. Slit-lamp examination can distinguish superficial from deeper lacerations. Small, superficial lacerations require no suturing and heal quickly. Topical prophylactic ophthalmic antibiotics are advisable. Larger (>1 cm) and deeper lacerations may require repair by an ophthalmologist. Clinical Features and Management: Corneal Lacerations.: Signs of corneal perforation (full-thickness corneal lacerations) include loss of anterior chamber depth, teardrop-shaped pupil caused by iris prolapse through the corneal laceration, and blood in the anterior chamber (Fig. 71-14). Small corneal lacerations can be difficult to diagnose. If aqueous humor is leaking from the corneal wound, it appears as streaming fluorescent dye surrounded by an orange pool of solution on slit-lamp examination (Seidel’s test). Full-thickness corneal lacerations are managed as described for blunt traumatic globe rupture.
Ophthalmology
Perspective
Ocular Trauma
Nonpenetrating Trauma
Cornea and Conjunctiva

Anterior Chamber and Iris
Scleral and Lens Injuries
Posterior Segment Injuries


Penetrating Trauma
Conjunctival Lacerations
Corneal and Scleral Lacerations
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree