67 Nosocomial Pneumonia
 Definitions
Definitions
Nosocomial pneumonia is an infection of the pulmonary parenchyma caused by pathogens predominantly present in hospital settings.1 Nosocomial pneumonia develops in patients admitted to the hospital for more than 48 hours, and usually the incubation period of this infection is no longer than 2 days. Nosocomial pneumonias include ventilator-associated pneumonia (VAP), which commonly develops in intensive care unit (ICU) patients who have been tracheally intubated and mechanically ventilated for at least 48 hours. Ventilator-associated tracheobronchitis (VAT) has not been as extensively studied as VAP in patients undergoing mechanical ventilation, but this disorder is characterized by signs of respiratory infection such as an increase in the volume and purulence of respiratory secretions, fever, and leukocytosis. However, in contrast to VAP, radiologic infiltrates suggestive of consolidation on chest x-ray are not observed.1 Healthcare-associated pneumonia (HCAP) is a new clinical entity that has recently been defined in the latest guidelines of the American Thoracic Society1 for the diagnosis and treatment of nosocomial pneumonia. Patients who develop HCAP are not hospitalized, but they present several risks for being colonized by pathogens present in hospital settings, including multiresistant microorganisms. Risk factors for developing HCAP are hospitalization for 2 days or more within the preceding 90 days, residence in a nursing home or extended care facility, home infusion therapy (including antibiotics), chronic dialysis within 30 days, home wound care, and a family member with multidrug-resistant (MDR) pathogen colonization or infection. Interestingly, there is still controversy about the etiology and definition of HCAP. Indeed, several North American studies have reported that HCAP is mostly caused by multiresistant microorganisms; conversely, European data show larger similarities between etiology of HCAP and community-acquired pneumonia.
Nosocomial pneumonia can also be classified based on the presence of microorganisms isolated through respiratory surveillance cultures and includes the following categories2:
The time of onset for nosocomial pneumonia also has important implications for possible etiology, empirical antimicrobial treatment, and outcomes. Langer et al.3 first differentiated between nosocomial pneumonia at early onset (developing within the first 4 days after hospital admission) and late onset (5 days or more). However, there are no well-designed trials supporting these time cutoffs. An interesting trial performed by Trouillet et al.4 found that three variables were significant for predicting infection with MDR VAP: duration of mechanical ventilation (MV) ≥ 7 days (odds ratio [OR] = 6.0), prior antibiotic use (OR = 13.5), and prior use of broad-spectrum drugs (third-generation cephalosporin, fluoroquinolone, and/or imipenem) (OR = 4.1).
 Epidemiology
Epidemiology
Incidence
Nosocomial pneumonia is the second most common nosocomial infection and the leading cause of death from nosocomial infections for critically ill patients. The incidence of nosocomial pneumonia is age dependent, with 5 of every 1000 cases affecting hospitalized patients younger than 35 years of age and up to 15 of 1000 in hospitalized patients older than 65.5 In earlier reports, nosocomial pneumonia increased hospital stay by 7 to 9 days per patient, accounting for up to 25% of all ICU infections and for more than 50% of the antibiotics prescribed.6 A Spanish report by Sopena et al.7 in 2005 studied the epidemiology of nosocomial pneumonia in 186 non-ICU patients from 12 hospitals and found that nosocomial pneumonia was observed mostly in elderly patients with underlying diseases and was primarily caused by S. pneumoniae, Legionella pneumophila, Aspergillus spp., and P. aeruginosa. The mortality rate was 26%, with an attributable mortality of 13%. Cook et al.8 estimated that the risk of VAP is 1% per day on mechanical ventilation8; they also demonstrated that the risk changes over time, being 3% the first 5 days on mechanical ventilation, 2% from the 5th to 10th day, and 1% for the remaining days. Considering that most invasively ventilated patients are intubated for less than a week, nearly half of VAP cases occur during the first days of mechanical ventilation.
Mortality
The crude mortality from nosocomial pneumonia may be as high as 30% to 70%, although several cofactors influence mortality during critical illness and make it extremely difficult to determine attributable mortality.9 Mortality caused by VAP has been defined as the percentage of deaths that would not have occurred in the absence of the infection. Several case-matching studies have estimated that one third to one half of all VAP-related deaths are the direct result of the infection, with a higher mortality rate in cases caused by P. aeruginosa or Acinetobacter spp. and associated with bacteremia.10 The development of VAP is accompanied by a 1.8- to 4-fold increase in the risk of death. A multicenter French study9 evaluated the attributable mortality and risk factors for death for late-onset pneumonia. They evaluated 764 patients admitted to the ICU for more than 96 hours and found a 47% mortality in patients with VAP versus 22% in the total population. Moreover, mortality was inversely related to adequacy of the initial empirical therapy. Similarly, Luna et al.11 assessed the appropriateness and delay of antibiotic therapy in 76 mechanically ventilated patients with bacteriologically confirmed VAP and found an overall mortality of 52.6%. Based on current evidence, nosocomial pneumonia is associated with a high mortality rate, but precise estimates of mortality attributable to this condition are not possible, owing to heterogeneity between patient populations, microbial patterns, antibiotic treatment, and diagnostic methods.12
 Pathogenesis
Pathogenesis
Role of Tracheal Tube in the Pathogenesis of ventilator-associated pneumonia
Pulmonary aspiration of colonized oropharyngeal secretions across the tracheal tube cuff is the main pathogenic mechanism for development of VAP. The endotracheal tube (ETT), commonly used in the ICU for long-term mechanically ventilated patients, includes a high-volume, low-pressure (HVLP) cuff. HVLP cuffs were originally designed to control pressure exerted against the tracheal wall and prevent tracheal injury.13–15 However, the potential diameter of the HVLP cuff is two to three times larger than the tracheal diameter, so when the tracheal cuff is inflated within the trachea, folds invariably form along the cuff surface, causing consistent micro- and macroaspiration of oropharyngeal secretions.16
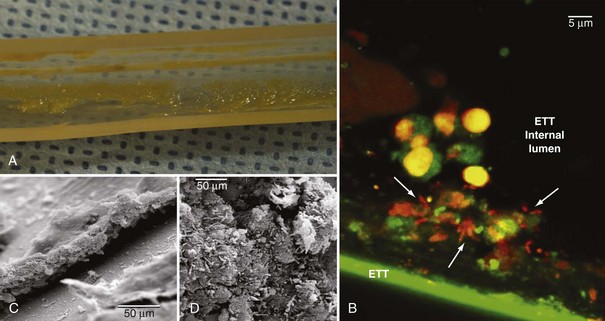
Pathogens may also grow on the internal surface of the ETT and ultimately translocate into the lungs. The ETT is commonly made of polyvinyl chloride (PVC), and bacteria easily adhere to its internal surface to form a complex structure called biofilm17,18 (Figure 67-1). Biofilm is composed of sessile bacteria embedded within a self-produced exopolysaccharide matrix.19 Biofilm on the internal surface of an ETT can be identified early following tracheal intubation.20,21 Sessile bacteria undergo phenotypic differentiation from their planktonic counterparts, and most of such differentiation constitutes a survival advantage. Indeed, bacteria within the biofilm are difficult to eradicate, and antibacterial efficacy of the host’s immune response and antibiotics are largely reduced. During mechanical ventilation, biofilm particles may dislodge into the airways as a result of inspiratory airflow17 and invasive medical interventions such as tracheal aspiration22 and bronchoscopy. Several studies have assessed the role of bacterial biofilm on pathogenesis of VAP and confirmed that the ETT biofilm is difficult to eradicate and constitutes a persistent source of colonization. Adair et al.23 studied 40 tracheal tubes obtained from critically ill patients with and without VAP and compared the genotype of bacteria retrieved from the lower airways and the ETT. In 70% of the samples obtained from patients with VAP, the authors found the same genotype in bacteria from ETT biofilm and the patients’ airways. Moreover, they confirmed that antibiotic susceptibility was lower in pathogens isolated from within the biofilm.
Sources of Colonization
Tracheally intubated patients in the ICU can be colonized either exogenously or endogenously. Patients are colonized exogenously by contaminated respiratory equipment, the ICU environment, and the hands of the ICU staff. Several reports have described ICU outbreaks due to colonized bronchoscopes,24,25 water supply,26,27 respiratory equipment,28,29 humidifiers,30 ventilator temperature sensors,31,32 respiratory nebulizers,33,34 and contaminated environment.35 Several factors play a significant role in reducing risks for cross-transmission of pathogens. Indeed, in every ICU an adequate ratio of single rooms to open beds should be provided; healthcare personnel should be adequately trained on infection control and preventive strategies; strict sterilization protocols and hand washing with alcohol-based solutions should be implemented, and finally, lower patient-to-nurse ratios are advantageous.
Endogenous colonization is believed to be the primary pathogenic mechanism for VAP development. In the critically ill patient, the oral flora shifts early to a predominance of aerobic gram-negative pathogens,36,37 Pseudomonas aeruginosa, and methicillin-resistant Staphylococcus aureus (MRSA). Therefore, pulmonary aspiration of oropharyngeal contents increases the risk for airway colonization and infection. Following aspiration and colonization of the airways, the occurrence of VAP primarily depends on the size of the inoculum, functional status, and the competency of host defenses. There is still controversy regarding the exact sequence of colonization and sources of infection in the pathogenesis of VAP. Early studies by Feldman et al.38 found that in patients undergoing mechanical ventilation, the oropharynx is the first site to be colonized by pathogens (36 hours), followed by the stomach (36-60 hours), the lower respiratory tract (60-84 hours), and thereafter the tracheal tube (60-96 hours).
Dental Plaque
In the healthy human, oral colonization with pathogens is prevented by the physical-chemical properties of the oral mucosa surface, the salivary enzymatic content, and specific proteases and immunoglobulins. ICU patients are at higher risk for dental plaque colonization due to difficulties in oral hygiene, changes in salivary properties during critical illness, and change of oral flora by antibiotic therapy. An early study by Scannapieco et al.39 showed that ICU patients are often colonized by aerobic pathogens on admission. More recently, Fourrier and collaborators40 found that prolonged ICU stay increases risks for colonization of dental plaque by aerobic pathogens. Moreover, the authors found that colonization of dental plaque was highly predictive of concurrent or subsequent nosocomial infection. Azarpazhooh et al.41 found evidence of an association of pneumonia with oral health (OR = 1.2 to 9.6, depending on oral health indicators). The authors reported that improved oral hygiene and frequent professional oral health care reduces the progression or occurrence of respiratory infection among high-risk elderly adults living in nursing homes and especially those in ICUs (number needed to treat [NNT] = 2-16; relative risk reduction [RRR] = 34%-83%). During critical illness and extensive antibiotic therapy, the oral flora may rapidly change; unfortunately, standard culture-based microbiological assays determine neither the dominant bacterial species nor the range of bacterial diversity within the community. In a study by Heo,42 18 ICU patients who developed VAP were studied, comparing genetic features of strains obtained from oral, tracheal, and bronchoalveolar lavage (BAL) samples. The authors found that oral respiratory pathogens were often genetically identical to pathogens recovered from the lower airways, and rapid changes of bacterial species in both oral and pulmonary sites appeared to occur.
Sinuses
The association between sinusitis and VAP has long been debated. Several studies have confirmed that orotracheal as compared to nasotracheal intubation is associated with a decreased incidence of sinusitis,43–45 and that incidence of VAP is lower in patients who do not develop sinusitis.46 A study by Holzapfel et al.47 evaluated the incidence of nosocomial maxillary sinusitis and pneumonia in patients who underwent either nasotracheal or orotracheal intubation. The authors found that sinusitis increased the risk of nosocomial pneumonia by a factor of 3.8.
Stomach
According to the gastropulmonary hypothesis of colonization, the stomach of ICU patients is often colonized by pathogens as a consequence of alkalinization of gastric contents by enteral nutrition and drugs. Continuous gastroesophageal reflux facilitates translocation of microbes into the oropharynx, which are then aspirated across the ETT cuff. Several trials have investigated the benefits of selective gut decontamination and stress ulcer prophylaxis and confirmed that preventing gastric alkalinization and reducing the bacterial burden of the stomach is associated with a lower incidence of nosocomial respiratory infections.48 Early studies have shown that in tracheally intubated patients, gastric pH higher than 4 is consistently associated with gastric colonization with pathogens.49,50 However, the association between gastric colonization and VAP found in early studies51–53 has been challenged by more recent studies.54–57 Overall, this area remains highly controversial, and several studies38,54,58–63 have not found a relationship with bacteria causing VAP as first originating in the stomach.
Impairment of Respiratory Defense During Critical Illness and Tracheal Intubation
In healthy subjects, the physiologic adduction of the true and false vocal folds provides full closure of the airways, and efficiently prevents aspiration of pathogen-laden oropharyngeal contents. The airways are additionally protected by the epiglottis, which moves over the top of the larynx to divert any fluid or solids from passing into the airways. Following intubation, the tracheal tube completely bypasses these anatomic barriers and creates a direct conduit for bacteria to be aspirated and reach lower airways. Cough is one of the most efficient mechanisms to prevent further translocation of pathogens that may have gained access into airways. In the healthy human, cough begins with an inspiratory effort followed by a forced expiratory effort against a closed glottis and ultimately, opening of the glottis to generate rapid expiratory airflow. Tracheal intubation prevents closure of the glottis, hence it fully hinders cough; moreover, intubated patients are often sedated and unable to generate high expiratory flows. Mucociliary clearance is the primary innate airway defense mechanism to clear pathogens. In young, healthy nonsmokers, the mucociliary velocity ranges between 10 and 15 mm/min. Studies in animals have consistently shown that inflation of the tracheal tube cuff within the trachea lowers mucociliary velocity by 37% within an hour, and 52% after 2 hours.64 Clinical studies65 in critically ill, tracheally intubated patients have confirmed those results and found that mucociliary velocity is very low (0.8-1.4 mm/min); lower mucociliary clearance has been associated with higher risks for pulmonary complications.
Although many ICU patients develop tracheal bacterial colonization during the course of mechanical ventilation, only a small proportion subsequently develop VAP. As previously mentioned, the daily hazard rate for developing VAP is higher during the first days of mechanical ventilation.8 Investigators have found that a temporary immunoparalysis can be found early in the course of the critical illness and admission to the ICU.66 In particular, researchers have focused on assessing human leukocyte antigen DR (HLA-DR) expression on peripheral monocytes as a marker of immune function.67–69 According to the rationale that impaired immune function may predispose to the development of VAP, low levels of HLA-DR expression have been found in patients who subsequently developed nosocomial pneumonia.70
Etiologic Agents
Nosocomial pneumonia may be caused by a variety of pathogens and, in many patients, more than one pathogen may be isolated. Microorganisms responsible for nosocomial pneumonia differ according to the ICU population, the duration of hospital and ICU stays, and the specific diagnostic method(s) used. VAP is commonly caused by aerobic gram-negative bacilli such as P. aeruginosa, Escherichia coli, Klebsiella pneumoniae, or Acinetobacter species, while S. aureus is the predominant isolated gram-positive pathogen.1,71–74 Data from 7087 infected patients (63.5% with respiratory tract infection) from the Extended Prevalence of Infection in Intensive Care (EPIC II) study75 have confirmed that Pseudomonas spp. and S. aureus are the most common isolated pathogens in intensive care units.
Few studies have assessed whether the pathogens that cause pneumonia in ventilated patients differ from those in patients who are not mechanically ventilated. Weber et al.76 evaluated 158,519 patients admitted to a single center over a 4-year period and identified 327 episodes of VAP and 261 episodes of nosocomial pneumonia. The infecting flora in ventilated patients mostly included MRSA (17.75%) and gram-negative bacilli such as P. aeruginosa (59.0%), Stenotrophomonas maltophilia (17.50%), and Acinetobacter species (6.75%). Similarly, in 20.37% of the patients not requiring mechanical ventilation, MRSA was identified, while a lower incidence of nosocomial pneumonia due to P. aeruginosa, Acinetobacter spp., and S. maltophilia was found. Nevertheless, the overall frequency of infection with these gram-negative pathogens was sufficiently high to warrant the use of empirical therapy likely to be active against them.
The high rate of polymicrobial infection in VAP has been shown repeatedly. Combes and colleagues77 studied 124 ICU patients, of whom 65 (52%) had monomicrobial VAP and 59 had (48%) polymicrobial VAP. In most patients, two different bacteria were isolated (42 patients, 34%); however, up to four different bacteria coexisted in 7 patients (6%). Interestingly, no differences were detected in mortality rate at 30 days between patients with polymicrobial or monomicrobial infection. A study by Teixeira et al.78 investigated risk factors for inadequate empirical antimicrobial therapy in 151 ICU patients and found that 69 (45.7%) patients with a clinical diagnosis of VAP received inadequate empirical antimicrobial treatment. Multiple logistic regression analysis revealed that inadequate antimicrobial treatment was associated with polymicrobial VAP (OR, 3.67; 95% confidence interval [CI], 1.21-11.12; P = 0.02), and importantly, inadequate antimicrobial treatment was associated with higher mortality for patients with VAP.
Underlying diseases may predispose patients to infection with specific organisms, Patients with chronic obstructive pulmonary disease (COPD), for example, are at increased risk for Haemophilus influenzae, Moraxella catarrhalis, P. aeruginosa, or Streptococcus pneumoniae infections.79,80 Patients with acute respiratory distress syndrome (ARDS) are at higher risk for developing VAP caused by S. aureus, P. aeruginosa, and Acinetobacter baumannii, and often in these patients, VAP is caused by multiple pathogens.81,82 Finally, trauma and neurologic patients are at increased risk for S. aureus, Haemophilus, and S. pneumoniae infections.83–85
It is important to identify MDR pathogens in order to guide appropriate antibiotic treatment. Causative pathogens of VAP that are potentially multiresistant are P. aeruginosa, MRSA, Acinetobacter spp., S. maltophilia, Burkholderia cepacia, and extended-spectrum β-lactamase (ESBL+) Klebsiella pneumonia. Conversely, S. pneumoniae, H. influenzae, methicillin-sensitive S. aureus (MSSA), and antibiotic-sensitive Enterobacteriaceae are not considered MDR pathogens. Patients at risk of being colonized by MDR pathogens are extremely heterogeneous, often present several comorbidities, and many receive antibiotics prior to and during the course of their hospitalization. Therefore, it is extremely challenging to accurately define risk factors for carrying MDR pathogens. Langer et al.3 tried to better classify patients who develop VAP, in order to provide data for guiding empirical antibiotic treatment. They compared early-onset and late-onset pneumonia and found that early-onset pneumonia is rarely caused by MDR pathogens, is less severe, and is associated with better outcome. However, recent reports are challenging such conclusions and demonstrate no association between MDR pathogens and time of onset of pneumonia.86,87 Those data suggest the need for additional studies to accurately identify risk factors for harboring MDR pathogens, rather than risk stratification based on nonspecific factors such as severity of pneumonia and time of onset. The incidence of MDR pathogens is also closely linked to local factors and varies widely from one institution to another. Consequently, each ICU has to continuously collect accurate epidemiologic data. Rello et al.88 analyzed variations of VAP etiology among three Spanish ICUs and compared them with data collected in Paris. The authors concluded that VAP pathogens varied widely among the four clinical centers, with marked differences in the microorganisms isolated from VAP episodes in Spanish centers as compared with the French site. Therefore, clinicians must be aware of the common microorganisms associated with both early-onset and late-onset VAP in their own hospitals to avoid the administration of inadequate initial antimicrobial therapy.
Legionella pneumophila as a cause of nosocomial pneumonia should be considered, particularly in immunocompromised patients.89 Often the source of legionellosis outbreaks within the hospital is a water system that has become colonized by the microorganism.90
The role of anaerobes in the pathogenesis of VAP requires further assessment, since the primary mechanism for VAP development is through aspiration of oropharyngeal contents, and the oropharynx is highly colonized by anaerobes. Robert et al.91 studied 26 mechanically ventilated patients and found that 15 patients became colonized with 28 different anaerobic strains. Similarly Dore et al.92 found anaerobic bacteria in 30 (23%) of 130 patients diagnosed with VAP, but always in association with aerobic pathogens. Importantly, empirical antibiotic therapy active against anaerobic bacteria appears to improve short-term outcomes in patients with VAP.93 Nevertheless, several authors94,95 were unable to reproduce those data, and the role of anaerobes in VAP is still considered controversial. In particular, Marik et al.95 studied microbiology of 185 episodes of suspected VAP through blind protected specimen brush sampling and mini-BAL and were unable to identify anaerobes as the causative pathogens of VAP.
Rarely, the causative organism of VAP is a fungus. Candida spp. and Aspergillus fumigatus are the most common isolated fungi, predominately in immunocompromised patients. In mechanically ventilated patients, the clinical significance of respiratory tract colonization by Candida is controversial. In a retrospective analysis of 639 patients from a Canadian study or VAP, 114 patients had Candida colonization of the respiratory tract.96 Interestingly, patients with Candida colonization had a significant increase in hospital mortality (34% versus 21% in patients without Candida colonization, P = 0.003). However, it is still unclear whether Candida colonization is associated with or responsible for worse outcomes. Moreover, a recent report showed that in ICU patients, isolation of Candida species in respiratory samples demonstrates only colonization rather than Candida pneumonia.97
It is commonly reported that VAP is infrequently due to viruses; however, it should also be acknowledged that patients with clinical suspicion of VAP are rarely screened for viruses. Daubin et al.98 studied 139 patients mechanically ventilated for more than 48 hours, of which 39 (28%) developed VAP. Although P. aeruginosa and MRSA still accounted for most of the VAP cases, herpes simplex virus type 1 was found in 12 cases of VAP and cytomegalovirus (CMV) in 1 case. Several studies have reported a high incidence of active CMV infection in mechanically ventilated patients.99–101 Recently, Chiche et al.102 studied 242 immunocompetent ICU patients and found active CMV infection in 39 (16%). At 28 days, only 15% of the patients with active CMV infection were weaned and alive, in comparison to 52% of patients free of CMV infection (P < 0.001).
 Prevention
Prevention
Nosocomial pneumonia is associated with high morbidity and mortality and constitutes an important burden for the healthcare system1,103; therefore, preventive strategies should be implemented to reduce overall incidence of the disease (Box 67-1). Strategies have focused on reducing cross-transmission, the likelihood of aspiration across the ETT cuff, and the bacterial load in the oropharynx. The Institute for Healthcare Improvement recommends that approaches with proven efficacy for reduction of morbidity and mortality related to infection control should be grouped and implemented together as a bundle, because together they are expected to result in a better outcome than when implemented individually. Designing a preventive bundle is just the first step and must be followed by continuous assessment of healthcare personnel compliance and improvements to implement interventions. Several reports104–106 have found drastic reductions in the incidence of VAP following implementation of VAP preventive bundles.
Box 67-1
Preventive Strategies for Nosocomial Pneumonia
General Prophylactic Measures
Maintaining high levels of education among ICU personnel relating to VAP pathophysiology and preventive strategies can be effective in reducing incidence of this problem.107–110 Respiratory care practitioners and nurses should be the primary recipients of education programs, and frequent performance feedback and compliance assessment should be undertaken.111 Interestingly, Needleman et al.112 studied administrative data from 799 hospitals in 11 states (covering 5,075,969 discharges of medical patients and 1,104,659 discharges of surgical patients) and found that a higher proportion of hours of care per day provided by registered nurses, compared to licensed practical nurses and nurses’ aides, were associated with lower incidence of pneumonia.
Adherence to simple infection-control measures such as alcohol-based hand disinfection effectively reduces cross-transmission of pathogens and incidence of VAP.113 The World Health Organization has endorsed hand hygiene as the single most important element of strategies to prevent healthcare-associated infections.114 Overall, most studies conducted in ICUs have shown consistent results and temporal association between implementation of alcohol-based hand hygiene and reduction of nosocomial infections.115–117
Kollef et al.118 demonstrated that patient transport outside the ICU was associated with increased risks for VAP. Clinicians and nursing staff should carefully carry out transport of intubated patients. In particular, the internal pressure of the ETT cuff should be always kept within the recommended range, particularly when the patient is expected to be maintained supine during diagnostic or therapeutic procedures; ventilator circuits should be carefully manipulated in order to prevent aspiration of colonized fluids from within the circuit.
Daily interruption or lightening of sedation to avoid constant impairment of respiratory defenses, as well as avoidance of paralytic agents, is highly recommended. It is well acknowledged that prolonged tracheal intubation is associated with VAP.8 A report by Kress et al.119 was recently confirmed by Schweickert et al.,120 who studied 128 mechanically ventilated patients randomized to continuous infusions of sedation with or without daily interruption. The authors demonstrated reduction of duration of mechanical ventilation and length of stay in the ICU when patients were allowed to wake up daily. Moreover, a trial by Schweickert et al.121 has shown that early physical and occupational therapy during critical illness is associated with more ventilator-free days. In a study by Strøm et al.,122 140 critically ill adult patients expected to be intubated for more than 24 hours were randomized to receive no sedation or sedation with daily interruption until awake. Both groups were treated with bolus doses of morphine. In that study, patients receiving no sedation had significantly more days without ventilation and shorter stay in the ICU. Results from these clinical trials are challenging standard sedation protocols for intubated patients and hold promise for reducing length of stay on mechanical ventilation and, ultimately, risks for VAP.
There is evidence of shorter length of mechanical ventilation, reduced rate of failed extubation, and decreased incidence of VAP when protocol-driven weaning from the ventilator is implemented.123,124 Marelich et al.123 randomized 385 patients to receive either a protocol-driven weaning procedure or standard care and found that duration of mechanical ventilation was decreased from a median of 124 hours for the control group to 68 hours in the protocol-driven weaning group (P = 0.0001). Moreover, a trend toward less VAP was found in the treatment group (P = 0.061).
Noninvasive Ventilation
Tracheal intubation and mechanical ventilation account for the main risk for nosocomial pneumonia and therefore should be avoided whenever possible. Noninvasive ventilation (NIV) is an attractive alternative for patients with acute exacerbations of COPD or acute hypoxemic respiratory failure and for some immunocompromised patients with pulmonary infiltrates and respiratory failure.125–128 NIV can also be safely used to facilitate early extubation and avoid continued invasive weaning. A meta-analysis129 evaluated 12 trials enrolling 530 participants, mostly with chronic obstructive pulmonary disease, and confirmed that noninvasive weaning is significantly associated with reduced mortality, VAP, and length of stay in the ICU and hospital. Another report130 emphasized the role of NIV in preventing reintubation in recently extubated patients at risk for relapse and respiratory failure. Kohlenberg et al.131 pooled data of 400 ICUs in Germany and found mean pneumonia incidence of 1.58 and 5.44 cases per 1000 ventilator days for NIV and invasive mechanical ventilation, respectively. Therefore, when indicated, NIV should be attempted to avoid tracheal intubation and reduce overall duration of tracheal intubation.
Tracheal Tube Cuff
Several strategies have been applied to improve the design of tracheal tubes and reduce the likelihood of aspiration of pathogen-laden secretions across the cuff. Novel ETT cuffs made of new materials such as polyurethane,16 silicone,132 and latex133,134 have been developed and tested in laboratory and clinical trials. Particularly, the polyurethane cuff has a thickness of 5 to 10 µm in comparison to 50 µm of PVC cuffs; hence, upon inflation, smaller folds form, and aspiration of secretions above the cuff can be prevented or reduced. Lorente et al.135 compared a standard ETT to an ETT incorporating an ultrathin polyurethane cuff and intermittent aspiration of subglottic secretions and found a reduction of incidence of VAP from 22.1% to 7.9% between the standard and new tubes, respectively (P = 0.001). A single-center study by Miller et al.136 tested the use of a polyurethane-cuff ETT versus a standard PVC cuff ETT, with a before and after design, and found that VAP rates decreased from 5.3 per 1000 ventilator days before the use of the polyurethane-cuffed ETT to 2.8 per 1000 ventilator days during the intervention year (P = 0.0138). The polyurethane-cuffed ETT has also shown benefits in reducing early postoperative pneumonia in cardiac surgical patients. Poelaert et al.137 studied 134 cardiothoracic surgery patients and demonstrated that the incidence of early postoperative pneumonia was significantly lower in the polyurethane group than in the polyvinyl chloride group (23% versus 42%, P < 0.03). Silicone132,138 and latex133,134,139 cuffs are low-volume, low-pressure cuffs and are promising alternatives to PVC cuffs. Upon inflation, folds are never formed, yet compliance of those materials is extremely high; thus they allow reliable control of the pressure exerted against the trachea. In a clinical trial on patients undergoing anesthesia or admitted to the ICU, Young et al.132 demonstrated high effectiveness of a silicone cuff in reducing pulmonary aspiration.
The shape of the cuff plays an important role in prevention of aspiration.133,140 In comparison to standard cuffs with cylindrical shapes, cuffs designed with a smooth, tapering shape allow elimination of folds for a full circumference of the trachea/cuff contact zone, irrespective of the cuff material.
It is important to maintain the internal pressure of ETT cuff pressure between 25 and 30 cm H2O, particularly when no positive end-expiratory pressure (PEEP) is applied; this serves to prevent either macroleakage of contaminated secretions into the lower airways or tracheal injury. A recent study141 demonstrated that frequently the ETT cuff was deflated or hyperinflated using standard management.
Ventilatory settings may play a role in pathogenesis of VAP. In particular, PEEP may decrease the incidence of VAP by counteracting hydrostatic pressure exerted by oropharyngeal secretions above the ETT cuff, hence reducing pulmonary aspiration.142 A recent report143 assessed effects of 5 to 8 cm H2O in normoxemic ventilated patients and showed reduction of the rate of VAP (PEEP group 9.4%, control patients 25.4%, relative risk, 0.37; 95% CI = 0.15-0.84; P = 0.017).
Tracheal Tubes Coated with Antimicrobial Agents
Coating the ETT with antimicrobial agents such as silver is a promising strategy to prevent biofilm formation within its internal surface and VAP. Olson et al.144 examined a silver-coated tracheal tube in comparison to standard tube in intubated dogs. The dogs were challenged with P. aeruginosa into the oropharynx. Using the new tube, the investigators were able to postpone colonization of the ETT inner surface (3.2 ± 0.8 versus 1.8 ± 0.4 days; P = 0.02) and reduce bacterial burden in the lung parenchyma (4.8 ± 0.8 versus 5.4 ± 9 log colony-forming unit [CFU]/g lung tissue; P = 0.01). Similarly, Berra et al.20 randomized 16 sheep to be intubated with a standard ETT or a silver sulfadiazine/chlorhexidine–coated ETT. After 24 hours of mechanical ventilation, all eight ETTs and ventilatory circuits in the control group were heavily colonized, and biofilm was found within the ETT. Pathogenic bacteria colonized the trachea and the lungs in five of eight sheep (up to 109 CFU/g). In the study group, seven of eight ETTs and ventilator circuits showed no growth and no biofilm; moreover, there was no bacterial growth in the lungs and bronchi, except for one bronchus in one sheep. Interestingly, the efficacy of silver-based coatings seems to decrease over time. Indeed, animal studies consistently reported no colonization and biofilm formation after 24 hours of mechanical ventilation. However, heavy ETT colonization was reported when studies were prolonged after 72 hours. To date, only one laboratory study145 has reported the absence of ETT colonization and biofilm formation following up to 168 hours of mechanical ventilation. In that study, the authors used ETTs internally coated with silver-sulfadiazine that were regularly cleaned with a novel concentric inflatable silicone device, the Mucus Shaver,146 devised to keep the ETT lumen free of mucus. The North American Silver-Coated Endotracheal Tube (NASCENT) randomized trial72 studied 1509 patients expected to require mechanical ventilation for more than 24 hours and randomized to be intubated with either a silver-coated or a conventional tube. The silver-coated ETT was associated with a lower incidence of microbiologically confirmed VAP (37/766 (4.8%) versus 56/743 (7.5%); P = 0.03), for a relative risk reduction of 35.9%. More importantly, the silver-coated tube had its greatest impact during the first 10 days of tracheal intubation. A retrospective cohort analysis by Afessa et al.,147 based on the NASCENT study, showed that the silver-coated ETT was associated with reduced mortality in patients with VAP (silver ETT versus control, 5/37 [14%] versus 20/56 [36%], P = 0.03), but mortality was higher in those without VAP (silver versus control, 228/729 [31%] versus 178/687 [26%], P = 0.03). In conclusion, there is promising evidence that ETTs coated with antimicrobial agents could reduce incidence of VAP. Nevertheless, clinicians should carefully consider benefits and limitations of these new ETTs and properly direct the use of silver-coated tubes to patients expected to be ventilated for longer periods of time and with higher associated risks for nosocomial pneumonia.
Shorr et al.148 analyzed cost-effectiveness of the silver-coated ETT as a preventive tool for VAP. Based on the NASCENT trial, the authors assumed a reduction in the relative risk of VAP from 35.9% to 24%. Assuming marginal VAP costs of $16,620 and costs of $90.00 for coated and $2.00 for uncoated ETTs, the authors found that savings per case of VAP prevented were $12,840.
Aspiration of Subglottic Secretions
Aspiration of colonized subglottic secretions through dedicated ETTs reduces hydrostatic pressure exerted above the cuff and potentially prevents macroleakage across the cuff. A meta-analysis149 comprising data from five studies and 896 patients has shown that subglottic secretion drainage reduced the incidence of VAP by nearly half (risk ratio [RR] = 0.51; 95% CI, 0.37-0.71), primarily by reducing early-onset pneumonia. Likewise, in the trial by Bouza et al.150 of 690 patients undergoing major cardiac surgery and on mechanical ventilation for more than 48 hours, the use of ETT tubes with aspiration of subglottic secretions was able to reduce incidence of VAP, median length of ICU stay, and antibiotic use and led to overall cost savings. In the multicenter trial by Lacherade et al.,151 333 patients were randomized to be intubated with either an ETT that allowed drainage of subglottic secretions or a standard ETT. Microbiologically confirmed VAP occurred in 14.8% of the patients in the treatment group, compared to 25.6% of the patients intubated with standard tube (P = 0.02). Importantly, this was the first trial reporting efficacy of subglottic secretions aspiration in reducing both early- and late-onset VAP in comparison to earlier studies (late onset VAP in 18.6% of patients in treatment group versus 33.0% of the patients in control group, P = 0.01). In more recent studies, aspiration of subglottic secretions was performed intermittently.135,151 The benefits of intermittent subglottic suction were similar to studies in which continuous aspiration of subglottic secretions was used. Hence, based on current evidence, intermittent aspiration (every 4-6 hours) is advisable to avoid potential risks for tracheal injury using continuous aspiration.152
Tracheostomy
Tracheostomized patients present the same risks for aspiration of pathogen-laden secretions pooled above the cuff153,154 as do orotracheally intubated patients. An observational study by Ibrahim et al.155 on 880 mechanically ventilated patients demonstrated an association between tracheostomy and higher incidence of VAP (adjusted OR, 6.71; 95% CI, 3.91-11.50; P < 0.001). Conversely, a case-control study by Nseir et al.156 on 354 patients mechanically ventilated for more than 7 days showed a lower rate of nosocomial pneumonia associated with tracheostomy (4.8 versus 9.2 episodes per 1000 ventilator days in patients with or without tracheostomy, respectively). Meta-analyses have assessed outcomes of early versus late tracheostomy.157–159 Unfortunately, all included studies were highly heterogeneous owing to differences in studied populations and no clear classification of “early” versus “late” tracheostomy. Nevertheless, the meta-analyses failed to demonstrate benefits of early tracheostomy on reduction of VAP incidence. To date, the latest multicenter randomized trial160 enrolled 419 mechanically ventilated patients to undergo either early or late tracheostomy. Patients in the early tracheostomy group underwent tracheostomy after a mean of 7 days, whereas patients in the late tracheostomy group underwent tracheostomy after a mean of 14 days. Although the authors found shorter length of mechanical ventilation and ICU stay with early tracheostomy, they were able to demonstrate only a trend toward a lower incidence of pneumonia and no difference in survival. Clinicians should consider that early tracheostomy may offer several benefits for mechanically ventilated patients: improved patient comfort, ability to communicate, capability for oral feeding, less need for sedation and analgesia, and reduced airway resistance in comparison to standard ETTs, which could be extremely important during the weaning period to shorten the duration of tracheal intubation.
Ventilator Circuit Management
Decreased frequency of ventilator circuit changes, replacement of heated humidifiers by heat and moisture exchangers, decreased frequency of heat and moisture exchanger changes, and closed suctioning systems have been tested as measures for preventing VAP. Results from clinical trials in adults161–167 and meta-analyses168,169 yield consistent evidence that routine change of the ventilator circuit does not decrease risks for VAP and costs. Therefore, circuits should not be changed unless the circuit is soiled or damaged. Importantly, inadvertent flushing of the contaminated condensate into the lower airways or nebulizers should be always avoided by careful emptying of ventilator circuits and water traps.170–172
Two meta-analyses assessed the effects of heated humidifiers (HH) and heat and moisture exchangers (HME) on prevention of nosocomial pneumonia. Kola et al.173 pooled data from nine clinical trials on 1378 patients and found that the use of HME decreased the rate of VAP (relative risk = 0.7; 95% CI = 0.50-0.94). Conversely, a meta-analysis by Siempos et al.174 including 13 studies on 2580 patients found no difference between HME and HH patients in the prevention of VAP and secondary outcomes such as ICU mortality, length ICU stay, duration of mechanical ventilation, or episodes of airway occlusion. Hence, to date there are no consistent data showing reduction in the incidence of VAP and better outcome using either HME or HH. Based on the ongoing controversy, neither humidification strategy can be recommended as a pneumonia prevention tool. However, it is rational to deliver inspiratory gases at body temperature or slightly below and at the highest relative humidity in order to prevent loss of heat and moisture from the airways and, more importantly, change in rheologic properties of secretions and impairment of mucociliary clearance.175 Therefore, the use of HH is indicated particularly in patients with hypothermia, prolonged mechanical ventilation, thick secretions, and chronic respiratory disorders. Finally, studies that have evaluated the effect of less frequent changes of heat and moisture exchangers on the development of VAP have found no increased risks.176–180 However, it is important to emphasize that when HMEs are used for prolonged periods of time, the technical performance of the devices should be periodically checked.
Closed tracheal suctioning systems have been introduced in clinical settings to avoid adverse events associated with ventilator disconnection during open tracheal suctioning and exogenous contamination of suction catheters entering the ETT. Three meta-analyses181–183 have compared the closed tracheal suction system to the open tracheal suction system in mechanically ventilated patients and found no benefits on VAP prevention. One meta-analysis182 evaluated nine randomized trials comprising 1292 patients and found no difference in the incidence of VAP between patients suctioned with closed or open systems (OR = 0.96, 95% CI 0.72-1.28). Moreover, data pooled from four of these nine studies showed a higher incidence of respiratory tract colonization in the group managed with a closed system (OR = 2.88, 95% CI 1.50-5.52).
The use of a saline solution instilled into the tracheal tube before tracheal suctioning remains controversial. Caruso et al.184 published a report on 262 patients randomized to receive either isotonic saline instillation before tracheal suctioning or no treatment. The authors found a lower incidence of microbiologically proven VAP (saline instillation versus no treatment: 23.5% versus 10.8%; P = 0.008), and no significant differences were found in secondary outcomes such as the incidence of ETT obstruction, pulmonary and lobar atelectasis, mortality, and duration of mechanical ventilation and ICU stay. Theoretically, in sedated patients in the semirecumbent position and with the internal surface of the ETT highly colonized, saline instillation may increase risks for translocation of pathogens into the airways, so current limited evidence suggests that routine saline instillation should not be recommended.
Body Position
Early studies clearly demonstrated that intubated patients are at higher risk for gastropulmonary aspiration when placed in the supine position (0 degrees) as compared with a semirecumbent position (45 degrees).185,186 One randomized trial187 demonstrated a reduction in the incidence of VAP in patients positioned in the semirecumbent position compared with patients treated completely supine. Moreover, the trial confirmed increased risk for VAP in patients enterally fed. A later randomized trial188 studied the feasibility of maintaining the head of the bed oriented 45 degrees during mechanical ventilation. This study found that patients were positioned on average only 28 degrees above horizontal, and no difference on VAP incidence was found. Thus, as strongly suggested by the American1 and European189 guidelines, intubated patients should be preferentially kept in the semirecumbent position (30-45 degrees) rather than supine (0 degrees) to prevent aspiration, especially when receiving enteral feeding.
Laboratory reports190,191 challenge the role of the semirecumbent position in patients with oropharyngeal colonization due to tracheal intubation or during the course of mechanical ventilation. Theoretically, in such patients a tracheal orientation above horizontal, as in the semirecumbent position, might facilitate aspiration across the tracheal tube cuff. Laboratory studies in animals190,191 consistently found that tracheal orientation and body position to avoid aspiration across the ETT cuff enhance mucus drainage and decrease risks for VAP; however, such results need to be confirmed in humans.
Rotating Bed
Normal healthy people change body position, even during sleep, every few minutes. Conversely, when critically ill patients are tracheally intubated and on mechanical ventilation, they are maintained in the supine, semirecumbent position for days with few or no changes in body position. Several ICU beds allow rotation of patients in the longitudinal axis from one lateral position to the other and seem to reduce extravascular lung water, improve ventilation-perfusion ratio, and enhance mobilization of airway secretions.192 Several studies have evaluated the effects of rotational therapy on VAP; however, most of these studies present limitations. For example, most studies used a clinical diagnosis of pneumonia, lack of standardization of VAP preventive measures, and included heterogeneity on the duration and type of rotation therapy. Three meta-analyses193–195 showed significant reduction in the incidence of VAP in patients undergoing rotation therapy, but they consistently failed to show beneficial effects on secondary outcomes such as duration of mechanical ventilation, length of stay, and mortality. An article by Staudinger et al.196 studied the effects of continuous lateral rotation therapy on the incidence of microbiologically confirmed VAP in 3 medical ICUs and found an incidence of 11% in the rotation group and 23% in the control group (P = 0.048), respectively. The authors also found that the duration of ventilation (8 ± 5 versus 14 ± 23 days, P = 0.02) and length of stay (25 ± 22 days versus 39 ± 45 days, P = 0.01) were significantly shorter in the rotation group. In conclusion, in patients at higher risk for prolonged immobilization and respiratory infection, continuous lateral rotation therapy should be considered as a feasible method exerting additive effects to other preventive measures for VAP.
Stress Ulcer Prophylaxis and Enteral Feeding
There is clear evidence that in intubated and mechanically ventilated patients, the stomach is often colonized by pathogens. Early studies showed that in tracheally intubated patients, gastric pH higher than 4 was consistently associated with gastric colonization.49,50 Alkalinization of gastric contents due to drugs for stress ulcer prophylaxis and continuous enteral nutrition were the main risk factors for gastric colonization.
In the ICU, stress ulcer prophylaxis is usually achieved with either sucralfate, histamine type 2 blockers (H2 blockers), or proton pump inhibitors (PPI). Sucralfate is the only treatment that potentially prevents stress GI ulceration without raising gastric pH. Several randomized studies have compared the effects of drugs that alkalinize gastric contents to sucralfate.52–57,197,198 Two studies compared either H2 blockers51 or sucralfate199 to placebo. Nine studies assessed gastric pH and colonization and consistently found lower pH and gastric colonization with regular use of sucralfate. Conversely, studies conducted by Bonten et al.54 and Thomason et al.56 found gastric luminal alkalinization and colonization, irrespective of the use of sucralfate. Finally, Eddleston et al.199 found no differences in gastric colonization when sucralfate was compared to placebo.
Randomized trials reported inconsistent results regarding stress ulcer prophylaxis and the incidence of VAP. In particular, early studies found a higher incidence of pneumonia in patients with alkalinized gastric contents,51–53 while more recent studies have not found such an association.54,55,124 Cook et al.55 studied 1200 patients randomized to receive either H2 blockers or sucralfate for stress ulcer prophylaxis. The authors found a higher risk for GI bleeding using sucralfate and no significant difference in VAP incidence, 19.1% and 16.2% in patients treated with H2 blockers or sucralfate, respectively. A recent meta-analysis200 on the efficacy and safety of PPIs in comparison with H2 blockers pooled data by seven randomized controlled trials on 936 patients and found no difference between PPI and H2-blocker therapy on the risk for pneumonia and ICU mortality. In conclusion, GI bleeding is a serious complication in critically ill patients at high risk for stress ulcers (i.e., patients with coagulopathy, need for prolonged mechanical ventilation, and history of GI ulceration or bleeding). The actual risk for VAP is unknown when accurate methods of enteral feeding (i.e., avoiding large gastric residual volumes) or other preventive measures are used in combination with stress ulcer prophylaxis. Therefore, clinicians must weigh the potential benefit of sucralfate (with potentially less VAP and more GI bleeding) versus H2 blockers/PPI (with potentially more VAP and less GI bleeding) and probably limit stress ulcer prophylaxis to high-risk patients.
Enteral nutrition has been considered a risk factor for the development of nosocomial pneumonia, mainly because of increased risks for alkalinization of gastric contents, gastro-esophageal reflux, and gastropulmonary aspiration. However, its alternative, parenteral nutrition, is associated with higher risks for catheter-related infections, complications of line insertions, higher costs, and loss of intestinal villous architecture, which may facilitate enteral microbial translocation. A large meta-analysis201 of 15 studies comprising 753 patients admitted to the ICU for trauma, head injury, burns, and abdominal surgery found a significantly lower incidence of infections and a reduced length of hospital stay associated with early enteral feeding. Conversely, studies in medical ICU patients have proven higher risk for VAP with early enteral feeding.202,203 Nonetheless, in a study by Artinian et al.202 the increased risk of VAP associated with early enteral feeding did not translate into an increased risk of death. Therefore, in medical ICU patients, the benefits of early nutrition should be balanced with associated increased risks for VAP.
A large number of studies have evaluated the risks for ICU-acquired pneumonia in patients randomized to either gastric or postpyloric feeding. Theoretically, many ICU patients present impaired gastric emptying; hence placement of the feeding tube beyond the pylorus has the potential to achieve nutrition goals without increased risks for gastropulmonary aspiration. A meta-analysis by Heyland et al.204 found that small-bowel feedings were associated with a lower incidence of pneumonia (RR, 0.77; 95% CI, 0.60-1.0); conversely, a meta-analysis by Ho et al.205 found no significant benefit on the risk of diarrhea, length of ICU stay, mortality, or risk of pneumonia. Therefore, ICU physicians should preferentially indicate postpyloric feeding in critically ill patients who have impaired gastric emptying.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree