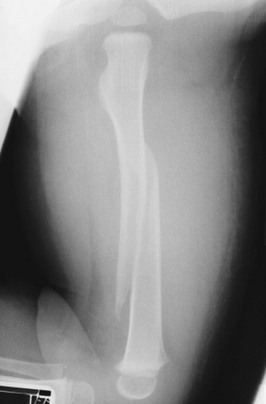
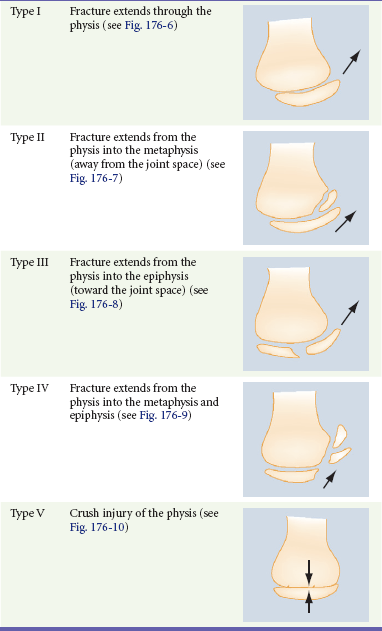
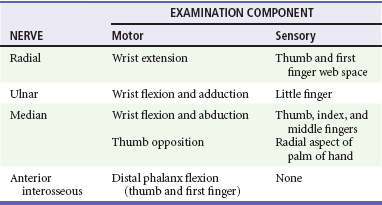
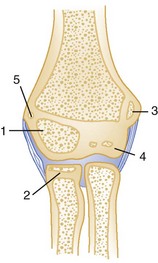
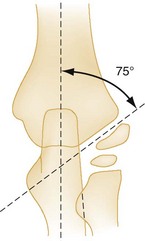
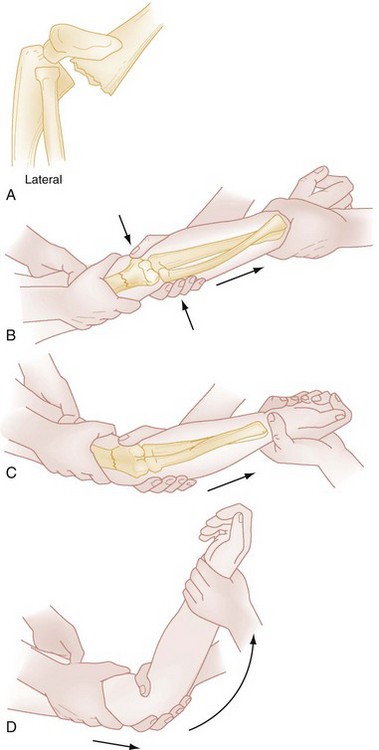
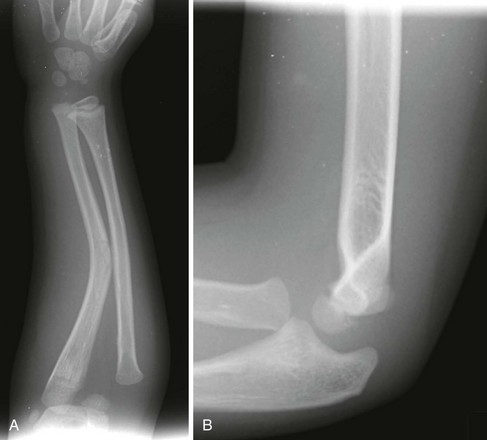
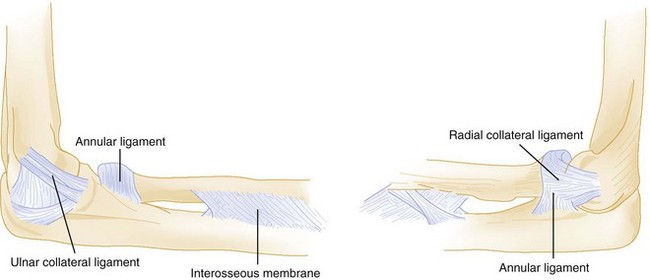
Chapter 176 Each year there are more than 11 million pediatric injury-related emergency department (ED) visits, 14.3% of which are due to fractures and dislocations.1 • Plastic deformation: Bone is bowed with no obvious cortical disruption. • Torus fracture (buckle fracture): Buckling of bone without cortical disruption tends to occur because of compression failure of the bone at the metaphyseal-diaphyseal junction (Fig. 176-1). These fractures may be immobilized with a splint or cast or, if they involve the distal end of the radius, a Velcro wrist splint2 or backslab.3 The splint or backslab can be removed by the family or primary care provider in 3 to 4 weeks, thereby obviating the need for orthopedic follow-up. Children treated with removable splints also had less pain, improved function, and fewer unscheduled ED visits because of problems with the cast.4 Buckle fractures also may be treated with a soft cast5,6 or a plaster splint.7 Figure 176-1 Buckle fracture of the distal end of the radius. Treatment consists of immobilization for 3 to 6 weeks. • Greenstick fracture: Bone and one cortex are disrupted; the periosteum on the fracture’s compression side remains intact (Fig. 176-2). Some authors recommend immobilization of minimally angulated (<15 degrees) distal radius greenstick fractures with splints8; others contend that casting is necessary because of continued fracture displacement during the first 2 weeks of healing.9 Figure 176-2 Greenstick fracture of the radius. This fracture may need to be completed for an anatomic reduction to be achieved. • Complete fracture: The fracture propagates completely through the bone; included are transverse (Fig. 176-3), spiral (Fig. 176-4), oblique, and comminuted (Fig. 176-5) fractures. The relatively weak cartilaginous physis in growing bone makes physeal injury common in the skeletally immature. Although injuries to the physis can occur at any age, they are more common during rapid skeletal growth. The Salter-Harris classification system is the most frequently used tool to describe physeal injuries. This classification system is based on the extent of involvement of the physis, epiphysis, and joint (Table 176-1). Types I and II Salter-Harris injuries (Figs. 176-6 and 176-7) do not involve the germinal layer of the growth plate; therefore, the risk for growth arrest is small. In general, the higher the Salter-Harris classification (Salter-Harris types III to V), the greater the damage to the growth plate and the greater the likelihood of growth arrest or limb-length abnormalities (Figs. 176-8 to 176-10). Type II fractures are the most common Salter-Harris injury and account for approximately three fourths of all growth plate injuries. An anteroposterior (AP) radiograph of the clavicle (Fig. 176-11) confirms the diagnosis. If clinical suspicion is high and the AP view does not reveal a fracture, a 30-degree cephalic view can be helpful. Specialized imaging studies are rarely needed, although computed tomography (CT) and duplex ultrasonography may be considered with proximal, posteriorly displaced fractures or dislocations to evaluate for the aforementioned complications.10 Supracondylar fractures are classified as flexion or extension according to mechanism of injury. The extension type of fracture constitutes 95% of all supracondylar fractures and typically results from a hyperextension injury to the elbow incurred in a fall onto the outstretched arm. In this injury, the olecranon is forcefully driven into the olecranon fossa, and the forces are concentrated in the supracondylar area. This mechanism results in failure of the anterior cortex and displacement of the distal fragment posteriorly. With extension-type supracondylar fractures, the degree of displacement and continuity of the cortex are further defined by the Gartland classification11 (Table 176-2). In the less common flexion type of supracondylar fracture, the elbow is flexed when it hits the ground, and energy is transferred from the posterior aspect of the proximal end of the ulna to the distal end of the humerus. This mechanism results in a supracondylar fracture with anterior displacement of the distal fragment and failure of the cortex posteriorly. Table 176-2 Gartland Classification of Extension-Type Supracondylar Fractures Modified from Gartland JJ: Management of supracondylar fractures of the humerus in children. Surg Gynecol Obstet 109:145, 1959. Children with supracondylar humerus fractures may present with anything from mild swelling and elbow pain to a grossly displaced humerus. Gentle palpation is useful to determine the site of injury; however, manipulation should be avoided because movement may cause further neurovascular damage. Children with extension-type supracondylar fractures hold the affected arm in extension with an S-shaped configuration of the elbow and exhibit a prominence at the olecranon. Children with flexion-type supracondylar fractures hold the arm in flexion and exhibit an empty space where the olecranon should be. In all cases it is important to carefully assess distal neurovascular status. Motor and sensory function should be evaluated by assessment of the radial, ulnar, and median nerves (Table 176-3). Two-point discrimination on the fingers provides a sensitive means of assessing sensory status: an abnormal value (>5 mm) indicates a deficit. Vascular assessment should include evaluation of radial and brachial pulses and capillary refill of the hand. Patients with displaced fractures should have ongoing assessment for the development of compartment syndrome of the forearm. With pain on flexion or extension of the fingers, forearm swelling, tenseness or tenderness, or pain that is disproportionate to the injury, compartment pressures should be measured immediately. Unrecognized ischemic injury can result in Volkmann’s ischemic contracture, which is characterized by fixed elbow flexion, forearm pronation, wrist flexion, metacarpophalangeal joint extension, and interphalangeal flexion. Radiographic evaluation of any elbow injury should include an AP view of the extended elbow and a lateral view of the flexed elbow. If these views do not show a fracture but clinical suspicion is high, oblique views are helpful. Even with proper radiographs, diagnosis of a pediatric elbow fracture can be difficult. The elbow is largely cartilaginous during early childhood, and the six secondary centers of ossification around the elbow can camouflage or be mistaken for fractures (Fig. 176-12). These ossification centers can be remembered by the mnemonic CRITOE: capitellum, radius, internal (medial) epicondyle, trochlea, olecranon, and external (lateral) epicondyle. The approximate ages at which these sites ossify may be estimated at 1, 3, 5, 7, 9, and 11 years, respectively (Table 176-4). Table 176-4 Sequence of Ossification around the Elbow: CRITOE Bone relationships are helpful in evaluation of a radiograph for a supracondylar fracture (Fig. 176-13). A true lateral view should demonstrate a figure-of-eight appearance of the distal humerus with bisection of the capitellum by the anterior humeral line. If the capitellum falls posterior to this line, an extension-type supracondylar fracture is likely. In all views, the proximal end of the radius and radial neck should point to the capitellum. Baumann’s angle also is helpful in diagnosis of subtle supracondylar fractures12 (Fig. 176-14). This angle is formed by a line drawn to follow the growth plate of the capitellum transected with a line that runs perpendicular to the axis of the humerus. The angle should be approximately 75 to 80 degrees. Baumann’s angle should be the same in both elbows, and differences between elbows can be used to detect subtle supracondylar fractures. In children younger than 3 years, difficult-to-distinguish bone landmarks limit the utility of Baumann’s angle. Postreduction alterations in Baumann’s angle reliably predict the final carrying angle.13 Fat pads also provide a means for detection of occult supracondylar fractures. A lateral radiograph with the elbow flexed at 90 degrees may show an anterior fat pad protruding from the coronoid fossa. This finding is normal unless the pad is bulging or in the shape of a ship’s sail. This “sail sign” may indicate fluid in the joint, although alone it may not be a reliable predictor of a fracture. The posterior fat pad, however, sits snugly within the olecranon fossa and should never be seen unless there is a fracture around the elbow. In this case, blood pushes the fat pad laterally, thereby making it visible on a lateral radiograph of the elbow. Accordingly, visualization of a posterior fat pad suggests the presence of an occult fracture around the elbow. The presence of a posterior fat pad without an obvious fracture warrants oblique views of the elbow (Fig. 176-15), splinting, and follow-up. Figure 176-15 Lateral radiograph of a supracondylar fracture with an anterior fat pad “sail sign” and a posterior fat pad. Plain radiographs usually are sufficient for diagnosis of supracondylar fractures. However, if the diagnosis remains in question after AP, lateral, and oblique radiographs are obtained, ultrasound imaging may be useful in infants,14 and magnetic resonance imaging (MRI) may be useful in older children.15 ED treatment of supracondylar humeral fractures is determined by displacement and neurovascular status. A pale, pulseless cold hand mandates emergency consultation with an orthopedic surgeon. If an orthopedic surgeon is unavailable and the vascular supply has not been restored, reduction should be attempted (Fig. 176-16). If necessary, reduction can be performed by a single operator. With the patient supine, the shoulder held in 90 degrees of forward flexion, and the elbow slightly flexed, both hands are placed on the arm proximal to the fracture, and both thumbs are placed on the posterior aspect of the fracture fragment. Then, while the thumbs are directed distally, the fragment is lifted onto the distal metaphysis. The return of blood supply is marked by the hand’s becoming warm and pink. If perfusion does not improve, another reduction may be attempted, with care taken to not entrap the brachial artery and median nerve. Multiple attempts at reduction increase the likelihood of neurovascular injury and swelling; therefore, no more than two reductions should be attempted. If perfusion is not reestablished, the child requires urgent operative intervention. A supracondylar fracture with a pulseless hand that is warm and pink does not need to be reduced immediately and should be splinted as it lies so that vascular status is not further compromised. The elbow should be splinted in relative extension because too much flexion in conjunction with swelling may obstruct the brachial artery and contribute to limb ischemia. The primary complications of supracondylar fractures are related to neurovascular injury. Type III fractures are at greatest risk, with neurovascular compromise occurring in as many as 49% of patients.16 Neurovascular compromise, however, can occur with any displaced fracture. The median nerve is involved in half of the cases and is associated with posterolateral displacement. The radial nerve is involved in almost one third of patients and is associated with posteromedial displacement. Brachial artery injuries, including arterial entrapment, laceration, intimal tears, thrombosis, and compression from compartment syndrome, occur in approximately 40% of patients and are found with either type of displacement. Fortunately, the brachial artery has many branches around the elbow, and flow to the forearm and hand can be maintained even when the brachial artery is injured. Despite the frequency of neurovascular deficits immediately after the injury, most nerve palsies are caused by stretching or contusion and resolve spontaneously. The typical course for nerve injuries is complete resolution. Although motor function usually returns within 12 weeks, sensory function may not return for 6 months or longer.17 If clinical or electromyographic evidence of nerve recovery is lacking after 5 months, exploration and neurolysis are indicated.18 Volkmann’s ischemic contracture (contracture deformity of the fingers, hand, and wrist) and permanent limb disability are the end result of untreated vascular injury. This complication is extremely rare and easily prevented by close observation and evaluation for the development of compartment syndrome. A few supracondylar fractures heal with a “gunstock” deformity; however, the combination of varus, hyperextension, and medial rotation of the limb is not a functional problem and, except in severe cases, requires no treatment. Severe cases can be corrected by humeral osteotomy. Monteggia’s fracture-dislocations are characterized by a fracture of the proximal third of the ulna plus dislocation of the radial head. The radiographic evidence can be subtle, with only a minor greenstick fracture or bowing of the ulna. Isolated ulna fractures are rare in children; therefore, with all such fractures, AP and lateral radiographs of the elbow should be obtained to rule out dislocation of the radial head. The radial head should align with the capitellum on all radiographs of the elbow; if it does not, a Monteggia injury should be suspected (Fig. 176-17). In one study, radial head subluxation, or nursemaid’s elbow, was the most common upper extremity injury in children younger than 6 years presenting to a pediatric ED.19 It typically occurs when axial traction is placed on an extended and pronated arm, as when the child is pulled up or swung by the arms. It also may occur when the child falls onto the outstretched arm, sustains minor direct trauma to the elbow, or simply twists the arm. In infants, radial head subluxation can occur when an extended arm is caught beneath the infant’s body while being rolled over. In pathoanatomic terms, subluxation occurs when the annular ligament becomes loosened from the head of the radius and slips into the radiocapitellar joint, where it becomes entrapped (Fig. 176-18). Nursemaid’s elbow occurs in children a few months to 5 years of age and has a peak incidence between 2 and 3 years of age.20 It has been reported in children younger than 6 months20 and has been seen in children as old as 9 years. This injury has a slight predilection for girls. The diagnosis of nursemaid’s elbow is made clinically, and radiographs are not necessary. If, however, significant point tenderness, swelling, or ecchymosis is present or if the history suggests another injury, such as a supracondylar fracture, radiographs should be obtained. Although it is not commonly used as a diagnostic procedure, ultrasound imaging may demonstrate a widened space between the radial head and the capitellum.21 Radial head subluxation is an orthopedic injury that is easily reduced without sequelae. Classically, the affected elbow is gripped with the clinician’s thumb over the radial head, and with the other hand, the clinician flexes and supinates the patient’s arm. As the radial head relocates, the clinician feels it click or “clunk” under the thumb. Hyperpronation of the forearm also is effective in reducing radial head subluxation. As is done in the flexion-supination maneuver, the child’s affected elbow is held with the clinician’s thumb over the radial head, but then flexion-supination is replaced with hyperpronation of the forearm. Success rates range from 8020 to 92%22 with supination and from 9323 to 98%24 with pronation. Pronation also may be less painful to the patient24,25 and is the reduction method of choice.24 After successful reduction, the child typically uses the arm normally within 10 minutes. This may be delayed in younger children and when the injury occurred more than 4 to 6 hours before reduction. Neither splinting nor orthopedic referral is required after a successful reduction. Parents should be cautioned to avoid traction on the forearm and elbow because recurrence rates of radial head subluxation range from 5 to 39%, depending on the referral population studied.20,22,24 With recurrent subluxations, immobilization in a posterior splint with the elbow maintained at 90 degrees and the forearm supinated may be warranted. The need for open reduction or repair of the annular ligament is exceedingly rare. AP and lateral radiographs may reveal a spiral or oblique fracture extending downward and medially through the distal third of the tibia (Fig. 176-19). An internal oblique radiograph is helpful if evidence of fracture is absent on the AP or lateral view. If findings on all views are normal, consideration should be given to fractures elsewhere in the limb. If no fracture is apparent, the child should be splinted for comfort and radiographs repeated in 10 days, at which time periosteal new bone or sclerosis of the fracture edges will make the fracture visible. If findings on these radiographs are normal and the child is still limping, further evaluation should be undertaken to rule out osteomyelitis and malignant neoplasm. Bone scans often are helpful in the assessment of a limping toddler and are more sensitive than plain radiographs for detection of fractures. Ultrasonography is also emerging as an imaging option in the detection of occult fractures in toddlers as well as in older children.26 Treatment of a toddler’s fracture consists of a below-knee walking cast for approximately 3 weeks. Fractures are the second most common manifestation of child physical abuse, second only to soft tissue injury, and are present in up to 70% of physically abused children. Fractures associated with child abuse occur in the very young, 50% in children younger than 12 months27 and 94% in children younger than 3 years.28 With child abuse, a timely and accurate diagnosis is imperative because children who are returned to an abusive home face a 35% chance of repeated abuse and a 10% chance of death; more than 20% of children who were diagnosed with a fracture from nonaccidental trauma had at least one previous physician visit at which abuse was missed.29 No fracture is pathognomonic for abuse, but certain fracture patterns are more worrisome than others. Any fracture in a child younger than 1 year, fractures at different stages of healing, and bilateral or multiple fractures indicate a need for thorough assessment for nonaccidental trauma (see Chapter 66). Injuries that are especially concerning include complex skull fractures, rib fractures, metaphyseal fractures, and vertebral fractures or subluxations. Midshaft humeral and scapular fractures are nearly always associated with abuse, as are approximately 70% of femoral fractures in children younger than 1 year. Diaphyseal Fractures: Although multiple fractures at different stages of healing are strongly suggestive of child abuse, the most common manifestation is an isolated diaphyseal fracture, which occurs four times as often as classic metaphyseal fractures. The humerus, femur, and tibia are the most frequently fractured long bones; the radius and ulna are the most infrequently fractured. With the exception of supracondylar fractures, all fractures of the midshaft of the humerus in children younger than 3 years are strongly suggestive of abuse. Metaphyseal Fractures: Although less common than diaphyseal fractures, metaphyseal fractures are more specific for child abuse. Metaphyseal fractures most commonly affect the tibia, femur, and proximal end of the humerus. Corner fractures and bucket-handle fractures, which are probably the same fracture viewed in two different projections, result from violent shaking or forceful pulling or twisting of an infant’s limb. The diagnosis is made by careful evaluation of high-quality plain radiographs. The tight adherence of the periosteum at the metaphysis precludes an active periosteal response, making these fractures difficult to diagnose even in the healing stages. In addition, after healing, these fractures may not be visible because of rapid bone remodeling. Bone scans, although sometimes helpful, are difficult to interpret because of the normally increased radionuclide uptake in the metaphyseal area. Rib Fractures: Rib fractures are present in 5 to 27% of cases of child abuse; 90% of such fractures occur in children younger than 2 years. The young pediatric rib cage is compliant, and considerable force is required to break a rib. Accordingly, rib fractures are seldom seen in unintentional injury and are almost never seen after cardiopulmonary resuscitation.30 When present, postresuscitation rib fractures are anterior and also may be multiple.30 In a child younger than 3 years, the positive predictive value of a rib fracture as an indicator of intentional trauma approaches 100%.31 Skull Fractures: Skull fractures are the second most frequent injury in abuse and occur more commonly in abuse cases than from unintentional trauma.26 Eighty percent occur in infants younger than 1 year, and although complex skull fractures are more suspicious for abuse, linear skull fractures are the most common type. Standard skull radiographs may not be adequate for diagnosis and are reported to miss more than 25% of head injuries. Children who meet high-risk criteria (the presence of rib fractures, multiple fractures or facial injury, or age younger than 6 months) should undergo CT or MRI for assessment of occult head injury.32 Periosteal New Bone Formation: Periosteal new bone formation, which is one of the most common findings in cases of abuse, reflects separation of the periosteum from the bone and may be the only manifestation of orthopedic trauma related to child abuse. It may be present with or without a fracture. It results from shaking, from acceleration-deceleration forces applied to an unsupported limb, or from forceful gripping. Diagnostic Strategies: Radiology.: Conventional skeletal radiography is the screening examination of choice in cases of suspected physical abuse. Unsuspected fractures are found in 22% of physically abused children and are more common in the very young. A complete skeletal survey is recommended for all physically abused children younger than 3 years and for all infants younger than 1 year with evidence of abuse or neglect. Complete skeletal surveys are rarely indicated in children older than 5 years; in children between 3 and 5 years of age, the need for a skeletal survey is determined on a case-by-case basis. Although standard practice has been to obtain skeletal surveys in infants with skull fractures without intracranial injury or suspicious clinical findings, their routine use has come into question as they have been found to find additional fractures in only 1.4% of patients.33
Musculoskeletal Disorders
Perspective
Principles of Disease
Fracture Patterns


Specific Disorders
Supracondylar Fractures of the Humerus
Type I
Nondisplaced fracture
Type II
Displaced fracture with intact posterior cortex
Type III
Displaced fracture with no cortical contact
A: Posteromedial rotation of the distal fragment
B: Posterolateral rotation of the distal fragment
OSSIFICATION CENTER
AGE AT APPEARANCE
AGE AT CLOSURE
Capitellum
6-12 months
14 years
Radial head
4-5 years
16 years
Medial (Internal) epicondyle
5-7 years
15 years
Trochlea
8-10 years
14 years
Olecranon
8-9 years
14 years
Lateral (External) epicondyle
9-13 years
16 years

Monteggia’s Fracture-Dislocation
Nursemaid’s Elbow
Toddler’s Fracture
Skeletal Aspects of Nonaccidental Trauma
Specific Disorders and Injuries
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal Disorders
Only gold members can continue reading. Log In or Register to continue