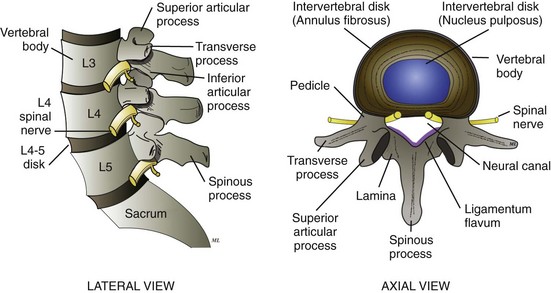
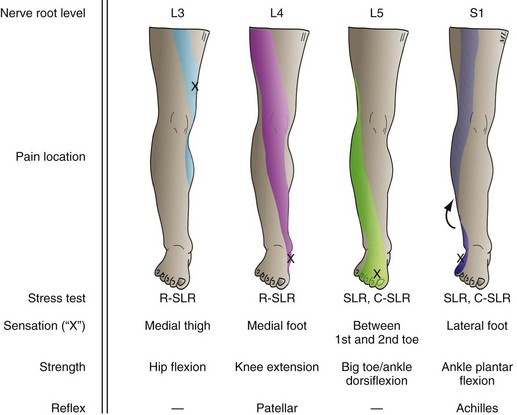
Chapter 54 Approximately 70 to 90% of adults during their lifetime experience acute low back pain, defined as pain lasting less than 6 weeks in duration.1,2 The cause of the back pain remains unknown in 85% of affected persons after appropriate initial investigation—a situation frustrating for both physician and patient.3 Frequent diagnoses in such cases include “acute lumbosacral strain,” “lumbago,” and “mechanical back pain.” These nonspecific, catch-all terms reflect the diagnostic challenge and lack of pathognomonic tests for low back pain. More accurately, these patients should be diagnosed with idiopathic low back pain. Regardless, most cases resolve spontaneously within 6 weeks. In recent studies on the management of acute low back pain, the most significant discovery—contradictory to traditional teaching from the 1980s—is the need for these patients, including those with sciatica symptoms, to avoid bed rest.4,5 Management recommendations for chronic back pain remain controversial, however, and the condition accounts for a significant proportion of costs to the health care system. In the ambulatory care setting the medical complaint of back pain is the fifth most common reason for a visit to a physician’s office, with 15 million annual visits in the United States, of which 7.3 million are to the emergency department (ED) at an average of 20,000 visits per day in 2008.6,7 Back pain was the leading cause of pain as reported in the 2010 National Health Interview Survey (NHIS), with 28.8% of the respondents reporting back pain lasting at least 1 day within the previous 3 months.8 Back pain primarily affects adults 30 to 60 years of age and has a tremendous impact on worker productivity, with significant economic consequences. It is the second leading cause of pain resulting in lost productive time from work, following headache.9 For aggregate hospitalization costs alone, it was the ninth most expensive condition in 2008 at more than $9.5 billion.7 Overall, patients with back pain account for billions of dollars in total direct and indirect costs in the United States.1,2,10 The natural history of most cases of low back pain follows a benign and self-limited course. In a large pooled analysis, patients reported a decrease in back pain by 58% within 1 month. If the pain did not resolve within 3 months, however, it was unlikely to resolve after 12 months. The recurrence rate for pain was 66 to 84% within the first 12 months.11 Risk factors for low back pain are continually being investigated. In a large systematic review, the presence of nonorganic signs of pain, poor pain-coping behaviors, great functional impairment, poor general health, and known psychiatric disease seem to predict patients who would develop chronic, disabling back pain in the future.12 Early evidence also points to a genetic predisposition to lumbar disk disease.13 Multiple other factors have been investigated, including body habitus, various occupations, deconditioning, tobacco smoking, stress levels, and psychological profile, with conflicting results.13–19 The lumbosacral spine consists of five lumbar vertebrae and the sacrum. Moving from anterior to posterior, each vertebra can be divided into the cylindrical vertebral body, two pedicles, two transverse processes, two overarching laminae, and a spinous process. These structures surround the neural canal, which houses the spinal cord and nerve roots and has a midsagittal anteroposterior diameter of 15 to 23 mm. The paired superior and inferior articulating processes join the articulating processes one vertebral level above and below. Each articulation site is called a facet joint. Intervertebral disks interpose between vertebral bodies, providing elasticity and stability to the vertebral column. Each disk consists of an inner colloidal gelatinous substance, the nucleus pulposus, and an outer capsule, the annulus fibrosus, which is thinner posteriorly than anteriorly (Fig. 54-1). Various ligaments and muscles also provide stability to the lumbosacral spine. The anterior and posterior longitudinal ligaments course along the anterior and posterior surfaces of the vertebral bodies. The posterior longitudinal ligament forms a border between the intervertebral disks and the neural canal. As expected, because this ligament thins as it runs inferiorly from L1 to S1, 95% of lumbar disk herniations occur at the L4-5 and L5-S1 levels, causing pain and neurologic deficit in the L5 and S1 distribution. Most herniations extrude posterolaterally to impinge on a nerve root asymmetrically.20 The ligamentum flavum courses just anterior to the laminae within the neural canal. With age, this ligament can thicken, potentially causing spinal stenosis. The spinal cord ends at the L1-2 interspace, and the lower cauda equina nerve roots extend inferiorly, exiting the sacral foramina as peripheral nerves to the lower extremity. Pain fibers supplying structures in the lumbosacral region primarily arise from the posterior rami and sinuvertebral nerves at each lumbar vertebral level. The nucleus pulposus and inner annular fibers of the intervertebral disk are unique in their lack of any pain fibers.21 This anatomic feature correlates consistently with magnetic resonance imaging (MRI) evidence of disk pathology in as many as 31% of asymptomatic patients. On follow-up, one study showed that abnormal disk findings in asymptomatic individuals did not predict the future development of back pain after 7 years. 21,22 Most conditions of low back pain have no proven cause. It is estimated that 85% of patients have no definitive diagnosis and are presumed to have pain originating from the soft tissue, including the muscles and ligaments.10,20 In the other 15% of patients with a known cause, the pain may originate in the nerve root, the articular facets, or the bone itself. In low back pain of nerve root origin, a spinal nerve root can become inflamed and painful with external impingement. Disk herniation, usually at the L4-5 and L5-S1 levels, is the most common cause of sciatica (i.e., pain radiating down the posterior leg from sciatic nerve root irritation). As the disk starts to desiccate and degenerate, starting in their 30s, patients are at increased risk for outward herniation of the nucleus pulposus with consequent nerve root impingement. With further aging, these disks progressively shrink in size. In keeping with these findings, symptomatic disk herniations typically are found in patients 30 to 50 years of age. Local nerve ischemia from physical compression also may contribute to the inflammation and pain. Studies also show that exposure of the nucleus pulposus during disk herniation may result in local neural inflammation, leading to pain.23 Nerve root impingement also can occur with spinal stenosis, a narrowing of the neural canal from congenital narrowing or, more often, from degenerative or hypertrophic changes of the disks, vertebrae, facet joints, and ligamentum flavum.24 The two most critical conditions that cause nerve irritation are cauda equina syndrome and a spinal epidural abscess. Cauda equina syndrome is most commonly a result of a massive central disk herniation, usually compressing multiple, bilateral nerve roots and causing back pain radiating to both legs, saddle anesthesia, and impaired bowel and bladder function (i.e., diminished rectal tone and urinary retention, respectively). Emergent surgical decompression is indicated to preserve neurologic function. An epidural abscess similarly results in nerve root impingement, commonly with spinal cord involvement, causing significant back pain and ultimately neurologic deficits. These rare infections develop most commonly from the hematogenous spread of both methicillin-sensitive and methicillin-resistant Staphylococcus aureus.20 Congenital and developmental spinal abnormalities also may cause back pain by nerve root inflammation in some cases, but much less frequently than was thought previously. Conditions such as kyphosis and scoliosis usually do not cause pain unless the degree of vertebral column misalignment is pronounced.25 Similarly, spondylolisthesis (slippage of one vertebral body on another) does not usually cause pain if the slippage is less than 25% of the vertebral body width. Even in patients with higher grades of anterior slippage (anterolisthesis), the development of severe back pain is rare. Although it is one third as common as anterolisthesis, backward slippage (retrolisthesis) is almost always associated with back pain. Multifactorial causes of spondylolisthesis include degenerative changes and trauma. Degenerative lumbar spondylolisthesis in older patients occurs most often at the L4-5 level (7.4% overall population prevalence), followed by the L5-S1 level (1.9%) and the L3-4 level (1.7%).26 Spondylolisthesis often is associated with bilateral pars interarticularis defects in the affected vertebra (spondylolysis). In low back pain of articular facet origin, as with any other joint in the body, degenerative changes in the synovial articular facets in the lumbosacral spine occur with age. Although the exact role and significance of articular facet joints in back pain are unclear, facet pathology has been suggested to contribute to 15 to 45% of chronic back pain cases.27 In low back pain originating from bone, direct irritation of the vertebral bone and its periosteum can cause back pain. The causes of spondylitis (osteomyelitis of the axial skeleton) can range from a slowly progressing tuberculosis infection (Pott’s disease) to a more acute bacterial infection. Typically, bacteria seed the bone from a hematogenous source, such as from a skin wound or urinary tract infection, or directly from intravenous drug use. The most common bacterial culprit is S. aureus. Primary and metastatic bone neoplasms can cause back pain from tumor infiltration into the bone. Primary bone tumors, such as multiple myeloma, chordoma, Ewing’s sarcoma, and osteosarcoma, occur 25 times less frequently than metastatic disease.28 Of the neoplasms, breast, lung, prostate, thyroid, and kidney cancers and lymphoma are the most likely to metastasize to bone. Inflammatory conditions, such as ankylosing spondylitis, other arthropathies, and osteoporosis also can cause back pain. In osteoporosis the generalized decrease in bone mineralization can cause pain from microfractures of the vertebral column. Referred pain, most commonly from intraperitoneal and retroperitoneal abdominal pathology, also is considered in patients with back pain. Chronic back pain is complex and multifactorial. Not only are the structural causes unclear, but the nonphysical factors are variable and difficult to determine. Functional factors range from fear, depression, and personality disorders to financial motivation. Although it is likely that many of these patients do experience some kind of chronic pain, it is unknown why their pain then triggers depression, drug dependence, and malingering in some people but not in others. One difference may be the degree of disruption that the condition causes in the patient’s lifestyle. A normally active and athletic person who is incapacitated is more profoundly affected than someone who is habitually sedentary. Psychological factors and potential compensation play a large role in the behavior of many patients with chronic back pain.12,17,29,30 It has traditionally been taught that pediatric back pain results in a diagnosis more often than adult pain; however, this axiom has been called into question as multiple studies have shown an increasing number of children being diagnosed with nonspecific back pain, accounting for at least 50% of cases, paralleling adults in pathophysiology.31–34 Children complaining of back pain require appropriate investigation. They may turn out to have spondylolysis with a variable degree of spondylolisthesis, Scheuermann’s disease (kyphosis and osteochondritis of the vertebral endplates), an infectious disease, or a neoplastic process. Disk herniation in children is comparatively rare, but when it does occur, the presentation is similar to that in adults.31 A thorough history and physical examination are crucial in evaluating all patients with acute low back pain. The classic historical (Table 54-1) and physical findings with various entities associated with low back pain are reviewed in this section. Although most of these causative disorders are benign, four such disorders have been identified by the Agency for Healthcare Research and Quality (AHQR) as “cannot miss” or “red flag” diagnoses: spinal fracture, cauda equina syndrome, spinal infection, and malignancy.5 A methodical and focused approach to the history and physical examination can help assess the patient’s pretest probability for each of these disease entities and determine whether further tests should be ordered. Table 54-1 Historical Clues to the Cause of Low Back Pain Uncomplicated Musculoskeletal Back Pain: Most patients with back pain can be classified in the category of those with uncomplicated musculoskeletal back pain. These patients have no red flag findings in their history and on physical examination. Often, patients are unable to recall an inciting incident. The pain usually is characterized as an “ache” or “spasm” and is localized asymmetrically in the lumbar paraspinous muscle, with radiation to the buttock or posterior thigh proximal to the knee. Movement exacerbates the pain, and rest relieves it. No associated deficit in sensation, strength, or bowel or bladder sphincter tone is identified in the history or on the clinical examination. The sole physical findings may be regional lumbosacral tenderness and a limited range of motion of the lower back. Radiculopathy: Approximately 1% of all patients with low back pain exhibit signs of lumbar radiculopathy (i.e., nerve root irritation).35 The most common causative process is herniation of a lumbar disk; other causes include spinal stenosis, malignancy, and infection. The most common type of lumbar radiculopathy is an L5 or S1 radiculopathy causing sciatica symptoms. Patients with sciatica describe their pain as radiating from the low back to the legs, distal to the knee. Such pain is characterized as “shooting,” “lancing,” “sharp,” or “burning.” Associated symptoms include focal numbness or weakness in one of the lower extremities. Exacerbating triggers include sitting, bending, coughing, and straining; relieving factors include lying supine and still. On physical examination the patient frequently exhibits tenderness to palpation in the sciatic notch. The straight leg raise (SLR) test is a fairly sensitive assessment tool to determine if the patient has sciatica. The SLR test is done with the patient supine and the legs extended. The symptomatic leg is passively raised while the knee is kept straight. The presence of back pain, which radiates past the knee when the leg is elevated 30 to 70 degrees, suggests an L5 or S1 radiculopathy. If the SLR test results in isolated low back pain without radiation symptoms to the legs, however, it is considered to be a negative finding. Through pooled analysis, the SLR test has a sensitivity of 91% but a low specificity of 26%, meaning that a negative result is fairly accurate in ruling out sciatica.36 Corroborative tests for sciatica include the “bowstring sign” (reproduction of pain with deep palpation of the taut “bowstring” posterior tibial nerve in the midline popliteal fossa) and reproduction of pain with foot dorsiflexion when the leg is elevated just short of the pain threshold during the SLR test. As an alternative to the SLR test, with the patient in a seated position, the knee can be extended (“flip test”), which also should stretch the sciatic nerve. Reproduction of the pain often causes the patient to lean backward reflexively from the pain, almost “flipping” back into a supine position. A crossed SLR test is done by passively raising the patient’s asymptomatic leg while keeping the knee straight. The presence of pain radiating from the back to the opposite affected leg has a sensitivity of only 29% but a high specificity of 88% for sciatica, meaning that a positive result on crossed SLR testing is almost pathognomonic for sciatica, whereas a negative result is nondiagnostic.36 In addition to stressing lumbar nerve roots, a thorough examination of the lower extremities detects subtle abnormalities associated with radiculopathies. This examination includes mapping the distribution of pain and assessing individual nerve root function, specifically strength, sensation, and reflexes. For the sensory examination, the earliest deficit can be detected by examining the most distal aspect of the dermatome. Specifically, light touch and pinprick sensation should be tested on the medial foot (L4), in the area between the great and second toes (L5), and on the lateral foot (S1) (Fig. 54-2). Herniated Disk: Patients with symptomatic herniated lumbar disks usually are 30 to 50 years of age and often have a long history of recurrent nonradicular low back pain, theoretically from irritation of the outer annular fibers of the disk. When the nucleus pulposus of the disk prolapses through the annulus fibrosus, local nerve root inflammation and radiculopathy result. Coughing, sitting, and any movement in general exacerbate the patient’s pain and radiculopathy symptoms. The severity of leg pain from radiculopathy often overshadows the back pain. Sciatica findings have a sensitivity of 95% for lumbar disk herniation, meaning that herniation is extremely unlikely in the absence of sciatica. The physical examination should focus on lower extremity neurologic function and signs of radiculopathy. Weakness of ankle dorsiflexion, great toe extension, ankle plantar flexion, and knee extension is associated with respective specificities of 70%, 70%, 95%, and 99% for lumbar disk herniation.20 Spinal Stenosis: Patients with spinal stenosis are typically older (mean age of 55 years) and constitute only 3% of all patients with low back pain.4,37 The classic history, identified in 60 to 75% of patients with spinal stenosis, is one of subacute or chronic pain and lower extremity radiculopathy that occurs with walking and is relieved with rest and, uniquely, bending forward at the waist.38 Because these symptoms mimic peripheral vascular claudication symptoms, pain from spinal stenosis is termed pseudoclaudication. Typically, vascular claudication lasts 5 minutes after resting, whereas pseudoclaudication lasts 10 to 15 minutes. Patients with spinal stenosis obtain symptom relief with spine flexion and bending forward, because these maneuvers increase spinal canal diameter and reduce spinal cord tension. Similarly, sitting also helps to relieve the symptoms in these patients, in contrast with patients with herniated disks. A typical patient describes walking uphill without pain but experiencing pain on walking downhill, when the back is extended. On physical examination, most patients are found to have a lumbar radiculopathy at one or multiple levels and increased back pain with extension.38 Classically, patients with spinal stenosis walk with a slightly bent-forward position. To help differentiate spinal stenosis from vascular claudication, peripheral pedal pulses and ankle-brachial indices should be checked. Degenerative Spondylolisthesis: Most cases of spondylolisthesis, forward displacement of one vertebral body over another, are caused by degenerative changes. This condition is most prevalent in adults older than age 50 and occurs most commonly at the L4-5 and L5-S1 junctions. Two thirds of older patients with radiographically documented degenerative spondylolisthesis are asymptomatic.39 For patients with pain, bending, twisting, and lifting activities aggravate the symptoms. Radiculopathies, spinal stenosis symptoms, or both may coexist. On physical examination, clinical findings may include a loss of lumbar lordosis causing a change in posture, a step-off along the midline spine if the spondylolisthesis is severe, tight hamstrings resulting in decreased mobility of the hamstrings and subsequent “waddling” gait, or a radiculopathy. Arthropathies: Inflammatory arthropathies, such as ankylosing spondylitis, rheumatoid arthritis, and psoriatic arthritis, all are associated with subacute and chronic low back pain. Patients with these conditions exhibit a decreased range of spinal flexibility. Commonly with ankylosing spondylitis, patients report morning back stiffness and pain relief with exercise. On physical examination, patients with an inflammatory arthropathy may have nonspecific manifestations, such as decreased spinal mobility, sacroiliac joint tenderness, and decreased chest expansion. Red Flag Diagnosis: Fracture: In all patients who have experienced significant blunt trauma to the back or only minimal trauma in the setting of osteoporosis, fractures of the spinal column are considered. Chronic corticosteroid users deserve special attention, because they typically have developed some degree of osteoporosis. In a 20-year observation study of 2631 collagen vascular patients, vertebral fractures occurred in 23.9% of patients on high-dose corticosteroids as compared with only 2.6% of patients on no corticosteroids.40 Thus providers should have a low threshold to assess this unique patient population for a fracture despite the absence of trauma. Red Flag Diagnosis: Cauda Equina Syndrome: Cauda equina syndrome results from a sudden compression of multiple lumbar and sacral nerve roots. Although it is an extremely rare presentation of back pain, it constitutes a neurosurgical emergency. The usual cause is a massive central disk herniation, but other potential causative disorders include spinal epidural abscess, hematoma, trauma, and malignancy. Patients with cauda equina syndrome have back pain and multiple-level radiculopathies, often involving both legs. Difficulty with bladder or bowel function, specifically urinary retention or decreased rectal tone, respectively, also may be a feature. Diagnostic dilemmas arise because the presentation can be atypical with equivocal neurologic compromise and only mild to moderate pain. The most consistent examination finding in cauda equina syndrome is urinary retention. Patients often complain of overflow incontinence owing to a neurogenic bladder. Given the high sensitivity of urinary retention of 90% and a negative predictive value of 99.99%, this disease process is extremely unlikely if the patient’s postvoid residual urine volume is less than 100 to 200 mL. This can be measured by urethral catheterization or estimated by ultrasonography.41 Saddle anesthesia—sensory deficit over the buttocks, upper posterior thighs, and perineal area—frequently is an associated finding, with a sensitivity of 75%. In 60 to 80% of cases, the rectal examination reveals decreased sphincter tone.20 Red Flag Diagnosis: Spinal Infection: Epidural abscess and spondylitis (osteomyelitis of the vertebral bone) are two types of dangerous spinal infections. Patients at higher risk include injection drug users, alcoholics, immunocompromised patients (e.g., patients with human immunodeficiency virus, diabetes mellitus, chronic renal failure, or long-term corticosteroid use), the elderly, patients who have sustained blunt trauma to the back, patients with an indwelling catheter or who have undergone recent dental instrumentation or instrumentation of the gastrointestinal or genitourinary tract or the spine, and patients with a recent bacterial infection.42–45 With spinal epidural abscess, however, approximately 20% of patients have no comorbid illnesses or risk factors. The most common bacterial culprit is S. aureus, spreading hematogenously from a remote site or from direct extension of a local infection, such as spondylitis or disk space infection. Less common culprits are streptococcal strains and enteric gram-negative bacilli. Patient history reveals back pain even at rest and subjective fevers. On physical examination, there is often tenderness to percussion over the spinous process near the abscess location. Spinal epidural abscess remains a diagnostic challenge despite the “triad” of fever, focal back pain, and neurologic deficit, because approximately 50% of the patients have no neurologic deficits, and 50% may be afebrile on initial presentation.46 With this subtle and often chronic presentation, many cases are misdiagnosed on initial presentation. Thus an awareness of this entity as a possible cause of low back pain is important for prompt diagnosis of this neurosurgical emergency, which carries a mortality rate as high as 15%.46–48 With spondylitis, infection often begins as a subtle hematogenous seeding of the disk space, causing diskitis. Subsequent contiguous spread of the disk space infection causes vertebral endplate erosion, leading to spondylitis. As with a spinal epidural abscess, the most common bacterial culprit is S. aureus. Less commonly, enteric gram-negative bacilli and Mycobacterium tuberculosis (in Pott’s disease) are the infecting organisms. Injection drug users also are at risk for Pseudomonas spondylitis. The history typically reveals a more indolent course of back pain, with subjective fevers. The physical examination findings can range from nonspecific tenderness of the spine to radiculopathy and cauda equina syndrome. Similarly nondiagnostic, the presence of fever has a sensitivity of only 27 to 50% for spondylitis.20 Red Flag Diagnosis: Malignancy: Vertebral infiltration with a tumor can be caused by either a primary or, more commonly, a metastatic malignancy. Classically, affected patients generally are older than 50 years and often complain of subacute or chronic back pain that is worse at night. In a systematic review, a history of known cancer, a moderately elevated erythrocyte sedimentation rate (ESR) (≥50 mm/hr), a significantly elevated ESR (≥100 mm/hr), hematocrit less than 30%, and clinical judgment yielded positive likelihood ratios for a vertebral malignancy of 23.7, 18.0, 55.6, 18.2, and 12.1.49,50 On examination, patients typically have mild to moderate spinal tenderness. Examination of the organs in which tumors are most likely to metastasize to bone, including breast, prostate, and lung, is indicated. Referred Back Pain: Referred pain often is difficult to differentiate from pain originating from the lumbosacral structures. It is vital, however, to make the distinction. A sudden onset of severe, “tearing” back pain is classically an aortic dissection. Abdominal pain radiating to the back may be caused by a ruptured abdominal aortic aneurysm in an elderly patient with atherosclerotic disease. Alternatively, abdominal pain radiating to the back could be from pancreatitis in a chronic alcoholic. Unilateral paraspinal pain associated with fever and nausea in a young woman could indicate pyelonephritis. Other examples of conditions radiating to the back include biliary diseases, pneumonia, pulmonary embolism, renal colic, and retroperitoneal hemorrhage. In all such cases, a thorough examination of the abdomen, genitourinary system, and cardiovascular system is essential. Pinpointing the primary cause of the pain may radically alter the therapy for the patient. Functional Back Pain: Distinguishing functional pain from “real” pain often is difficult, but several clues can be elicited from the history. A prolonged history of nonanatomic pain complaints, vague pain descriptions without localization, multiple lawsuits over similar problems, multiple prescriptions for narcotics from different providers, and lack of coordinated care for a problem that otherwise seems to dominate the patient’s life all suggest that a search for a physical cause would be fruitless. In such cases, secondary gain for the patient’s complaints often is likely. Fourth, a patient who generally overreacts during the examination probably is not giving a true reflection of the actual discomfort. All of these signs are believed to correlate well with psychopathology but have poor prognostic value. They are suggestive of malingering and functional complaints but are neither sensitive nor specific enough to rule out organic pathology.51,52
Musculoskeletal Back Pain
Low Back Pain
Background
Epidemiology
Principles of Disease
Pathophysiology
Clinical Features
QUESTIONS FOR PATIENT
POTENTIAL DIAGNOSIS
Does the back pain radiate down past the knees?
Radiculopathy and likely a herniated disk
Is the pain worse with walking and better with bending forward and sitting?
Spinal stenosis
Do you have morning back stiffness that improves with exercise?
Ankylosing spondylitis
Are you older than 50 years?
Osteoporotic fracture, spinal malignancy
Has there been any recent history of blunt trauma?
Fracture
Do you take long-term corticosteroids?
Fracture, spinal infection
Do you have a history of cancer?
Spinal metastatic malignancy
Does your pain persist at rest?
Spinal malignancy, spinal infection
Has there been persistent pain for longer than 6 weeks?
Spinal malignancy
Has there been unexplained weight loss?
Spinal malignancy
Is the pain worse at night?
Spinal malignancy, spinal infection
Are you immunocompromised (e.g., HIV infection, alcoholism, diabetes)?
Spinal infection
Have you had fevers or chills?
Spinal infection
Do you have pain, weakness, or numbness in both legs?
Cauda equina syndrome
Do you have bladder or bowel control problems?
Cauda equina syndrome
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal Back Pain
Only gold members can continue reading. Log In or Register to continue