INTRODUCTION
URINALYSIS
To evaluate for the presence of cells, casts, and crystals.
Freshly collected urine specimen, centrifuge, graduated centrifuge tubes, glass microscope slide, and coverslip.
Pour 10 mL of freshly collected urine into a graduated centrifuge tube.
Centrifuge at ×400 to ×450 gravity for 5 minutes.
Decant 9 mL of supernatant, leaving 1 mL in the tube.
Resuspend the centrifuged pellet in the remaining 1 mL of urine by stirring with a pipet.
Place one drop of resuspended urine on a glass microscope slide.
Overlay with a coverslip.
Examine initially using scanning ×10 power, emphasizing the periphery of the coverslip, since urinary elements tend to gather at the edges.
Switch to ×40 power to focus on specific urinary elements such as cells, casts, and crystals. Use ×100 power as needed for specific identification.
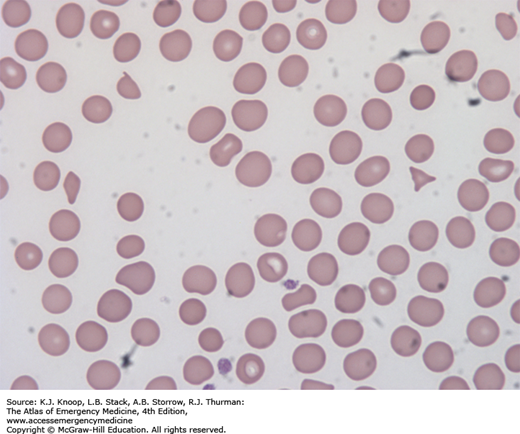
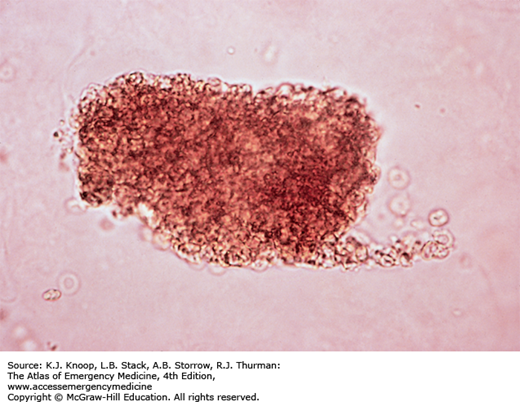
FIGURE 25.1
Calcium Oxalate Crystals. Calcium oxalate crystals come in two shapes. The classically described octahedral, or envelope-shaped, crystals are made of calcium oxalate dihydrate. Calcium oxalate monohydrate crystals are needle-shaped. They are seen in acid or neutral urine. They may be found in the urine of patients with ethylene glycol ingestion. In addition, the urine of patients with ethylene glycol ingestion may also fluoresce under a Wood lamp. (Reproduced with permission from Strasinger SK, Di Lorenzo MS. Urinalysis and Body Fluids. 4th ed. Philadelphia: F.A. Davis Company; 2001, p. 97.)
SYNOVIAL FLUID ANALYSIS FOR CRYSTALS
To determine the presence of uric acid crystals (in patients with gout) or calcium pyrophosphate crystals (in patients with pseudogout) in joint fluid.
Freshly collected joint fluid, glass microscope slide, coverslip, and polarizer.
To prevent interference from polarizing artifacts, clean the slide and coverslip with alcohol prior to using them.
Using freshly collected unspun joint fluid, place a drop of joint fluid on the glass microscope slide.
Overlay coverslip.
View the slide using the polarizer.
Scan at ×10 power; ×100 power is needed to see intracellular crystals.
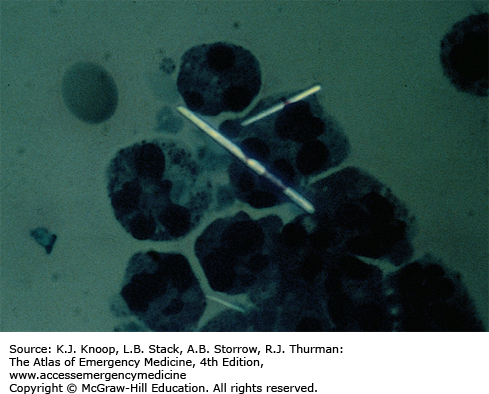
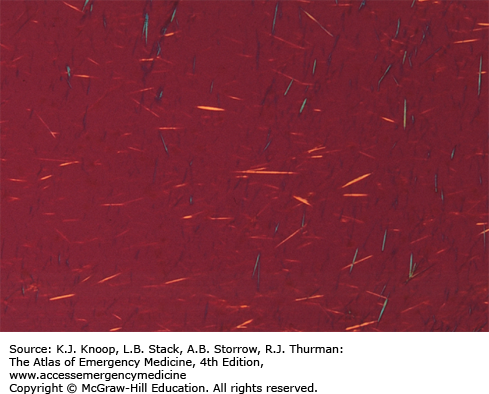
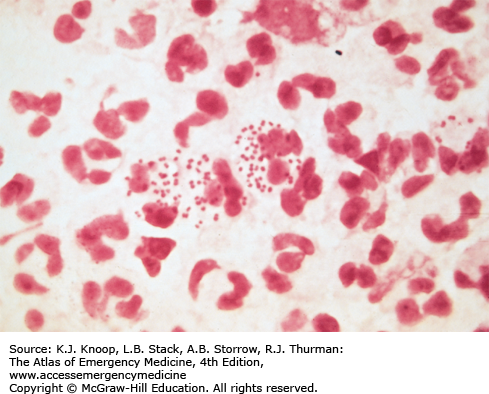
FIGURE 25.6A
Polarized Uric Acid Crystals (×500). Intracellular needle-like uric acid crystals are seen within the polymorphonuclear cells from the joint fluid in a patient with gout, using a direct polarizing light. (Reproduced with permission from Strasinger SK, Di Lorenzo MS. Urinalysis and Body Fluids. 5th ed. Philadelphia: F.A. Davis Company; 2008, p. 216.)
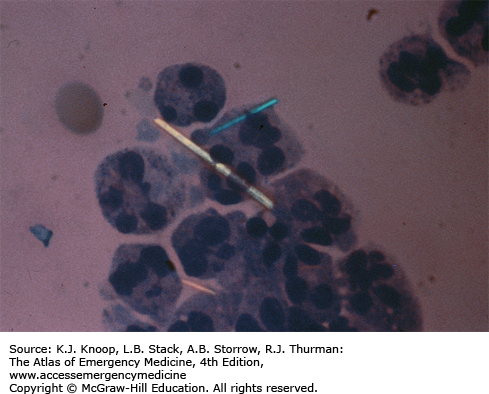
FIGURE 25.6B
Compensated Polarized Uric Acid Crystals (×500). Once crystals are found with a direct polarizing light, identification is made by using a compensated polarized light. The yellow crystal is aligned parallel to the slow vibration component of the compensator (negatively birefringent). The blue crystal is perpendicular (crossed urate blue). (Reproduced with permission from Strasinger SK, Di Lorenzo MS. Urinalysis and Body Fluids. 5th ed. Philadelphia: F.A. Davis Company; 2008, p. 217.)
FIGURE 25.6C
Extracellular Uric Acid Crystals (×100). Extracellular uric acid crystals are seen under compensated polarized light. Notice the change of color with crystal alignment. (Reproduced with permission from Strasinger SK, Di Lorenzo MS. Urinalysis and Body Fluids. 5th ed. Philadelphia: F.A. Davis Company; 2008, p. 216.)
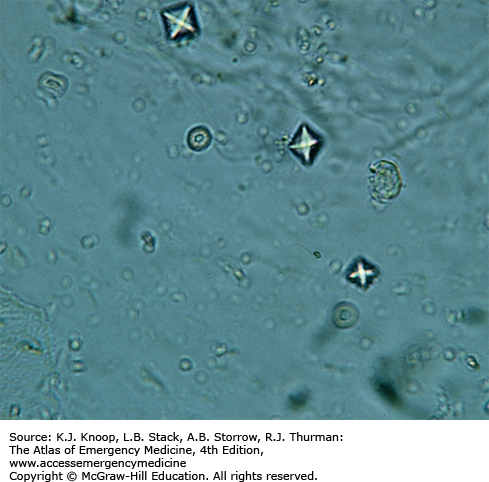
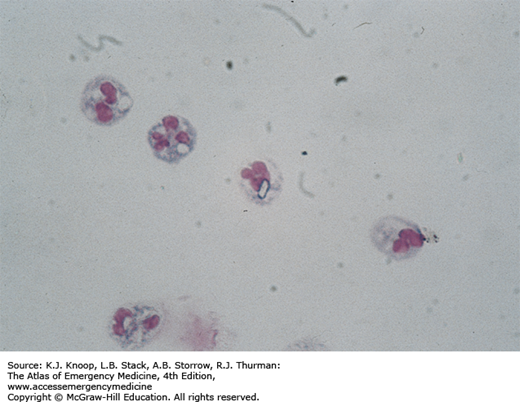
FIGURE 25.7A
Polarized Calcium Pyrophosphate Crystals (×1000). Intracellular rhomboid crystals in the joint of a patient with pseudogout. They may also appear as rods. (Reproduced with permission from Strasinger SK, Di Lorenzo MS. Urinalysis and Body Fluids. 5th ed. Philadelphia: F.A. Davis Company; 2008, p. 216.)
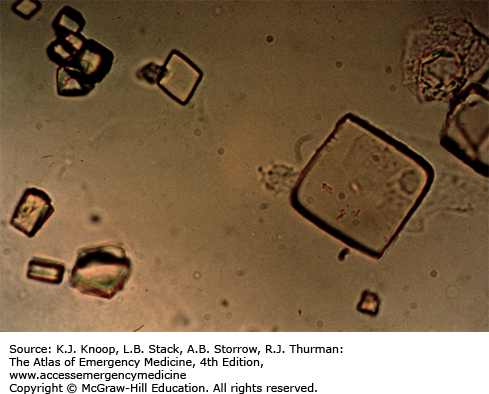
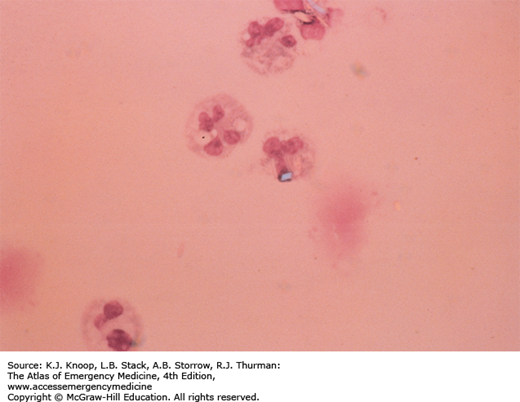
FIGURE 25.7B
Compensated Polarized Calcium Pyrophosphate Crystals (×1000). The blue calcium pyrophosphate crystal is aligned parallel to the slow vibration component of the compensator (positively birefringent). (Reproduced with permission from Strasinger SK, Di Lorenzo MS. Urinalysis and Body Fluids. 5th ed. Philadelphia: F.A. Davis Company; 2008, p. 217.)
GRAM STAIN
The first step in the identification of a predominant bacterial organism in a specimen. Classifies an organism by its cell wall’s ability to retain crystal violet dye during solvent treatment. Morphology of the organism is also identified.
Freshly collected specimen to be examined, glass microscope slide, crystal violet, Gram iodine, acetone-alcohol (acetone, 30 mL, and 95% alcohol, 70 mL), safranin, and Bunsen burner.
Put specimen on dry, clean glass microscope slide and allow to air dry.
Heat-fix specimen by gently passing over flame.
Cover specimen with crystal violet for 1 minute.
Rinse off completely with water; do not blot.
Cover specimen with Gram iodine for 1 minute.
Rinse off completely with water; do not blot.
Decolorize for 30 seconds with gentle agitation in acetone-alcohol.
Rinse off completely with water; do not blot.
Cover with safranin for 10 to 20 seconds.
Rinse off completely with water and let air dry.
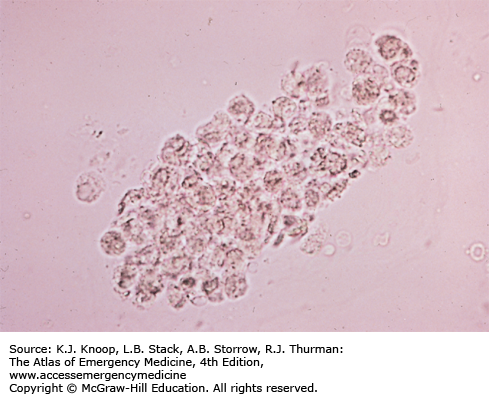
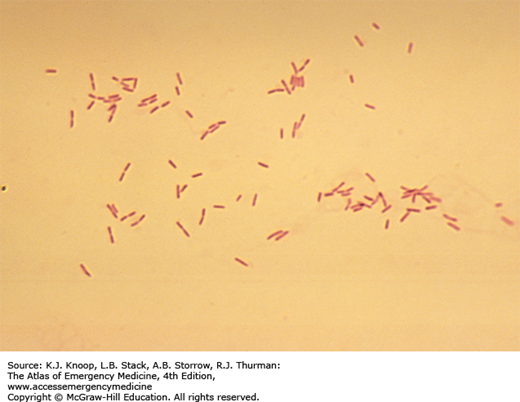
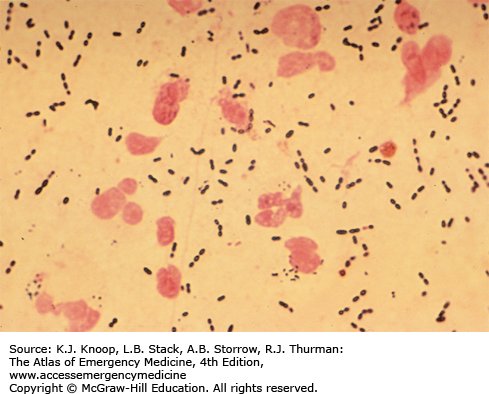
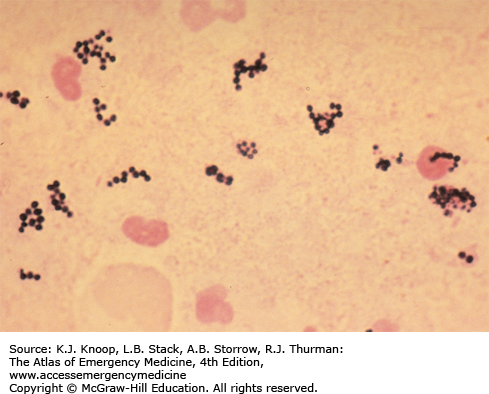
FIGURE 25.11
Gram Stain—Neisseria gonorrhoeae. Multiple gram-negative, intracellular diplococci from a patient with N gonorrhoeae. (Reproduced with permission from Morse SA, Holmes KK, Ballard RC, Moreland AA (eds). Atlas of Sexually Transmitted Diseases and AIDS. 4th ed. Saunders Elsevier; 2010. Copyright © 2010 Elsevier, Ltd.)
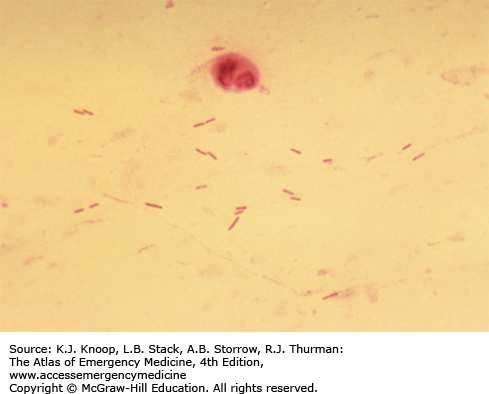
DARK-FIELD EXAMINATION
To evaluate a lesion (chancre, mucous patche, condyloma lata, skin rash) for the presence of Treponema pallidum.
Compound microscope with dark-field condenser (dark-field microscope), glass microscope slide, coverslip, and physiologic saline.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree