INTRODUCTION
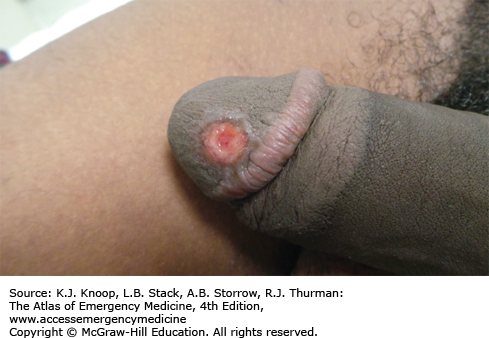
SEXUALLY TRANSMITTED INFECTIONS: SYPHILIS
Syphilis is a systemic illness caused by Treponema pallidum. The disease occurs in stages, with each stage having distinct physical findings. Primary syphilis is heralded by the development of a single lesion at the site of inoculation. This usually occurs within 2 to 6 weeks of exposure, but may take as long as 90 days. Patients often do not notice or seek care for the primary lesion. They may, however, present with a solitary, round, painless genital chancre or ulcer. The ulcer may also be slightly painful and multiple ulcers are sometimes seen. The base of the genital ulcer is typically dry in males and moist in females; purulent fluid in the base is uncommon. The borders of the ulcer are often indurated. Although genital ulcers are most common, ulcers may develop at any exposed site. Bilateral, nontender, nonfluctuant adenopathy is common. Without treatment, ulcers will resolve spontaneously within 3 to 12 weeks as the infection progresses to the secondary stage. Patients with primary syphilis are at risk for concurrent infection with other sexually transmitted infections.
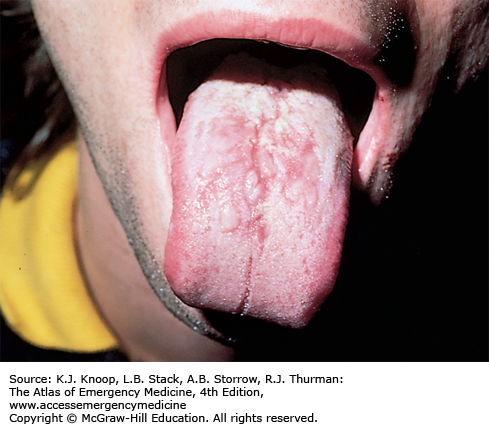
Secondary syphilis involves systemic dissemination of T pallidum and manifests first with the development of diffuse, nonpruritic macules. The macules develop within 2 to 10 weeks after resolution of the primary ulcers. The macules later evolve into a maculopapular eruption with small, round or annular lesions and involve primarily the trunk, palms, and soles. Diffuse, painless lymphadenopathy is also seen at this stage. Mucous patches may develop on the tongue and buccal mucosa. Condyloma lata and patchy alopecia can also be seen during this stage. The manifestations of this stage resolve without treatment in several months. Despite resolution of the symptoms, untreated syphilis will persist in the body and may become latent or later manifest as tertiary syphilis, a discussion of which is beyond the scope of this text.
To confirm the diagnosis, check an RPR or VDRL. Also test the patient for HIV and other sexually transmitted infections such as Neisseria gonorrhea and Chlamydia. Parenteral penicillin G is the preferred treatment for every stage of syphilis. For primary or secondary syphilis, treat with a single dose of benzathine penicillin G, 2.4 million units, intramuscularly. Treat penicillin-allergic patients with either doxycycline 100 mg orally twice daily or tetracycline 500 mg orally four times daily for 14 days. Refer pregnant patients with penicillin allergy for desensitization and subsequent treatment with pen G as the alternative treatments are both contraindicated in pregnancy.
Serum titers need to be followed in 6 to 12 months to confirm adequate response to treatment. Presumptively treat any sexual partners the patient has had within 90 days and recommend serologic testing for any partners outside of 90 days with subsequent treatment based on the results. All cases of syphilis must be reported to the appropriate public health agency.
Warn patients about the potential development of the Jarisch-Herxheimer reaction which is caused by the massive release of endotoxins from the dying spirochetes following antibiotic treatment. This reaction usually occurs within hours of treatment. It is characterized by fever, headache, malaise, and myalgias and is self-limited.
Consider dark-field microscopy examination of scrapings from the lesion of the primary stage or from the rash, mucocutaneous patches, or condyloma lata of the secondary stage to rapidly confirm the diagnosis.
Lesions of secondary syphilis are very infectious. Always wear gloves when examining a patient with a rash that may be due to secondary syphilis.
Pretreatment with nonsteroidal anti-inflammatory drugs may attenuate the Jarisch-Herxheimer reaction.
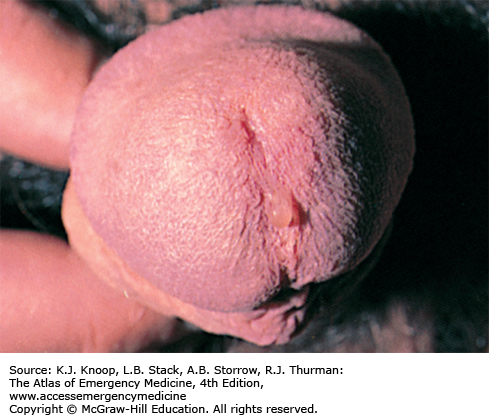
FIGURE 9.8
Mucous Patches. Oral involvement in secondary syphilis manifested by mucous patches. These lesions are very infectious, and dark-field examination is often positive for spirochetes. (Reproduced with permission from Morse SA, Holmes KK, Ballard RC, Moreland AA (eds). Atlas of Sexually Transmitted Diseases and AIDS. 4th ed. Saunders Elsevier; 2010. Copyright © 2010 Elsevier, Ltd.)
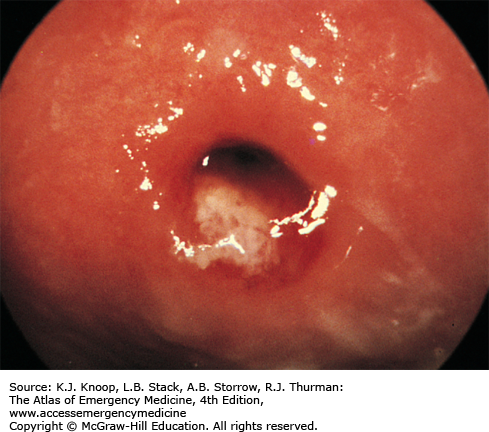
FIGURE 9.9
Condyloma Lata. Typical appearance of the smooth, broad-based, hypopigmented flat plaques of condyloma lata, a manifestation of secondary syphilis. (Photo contributor: H. Hunter Handsfield, MD. From Handsfield HH (ed): Atlas of Sexually Transmitted Diseases, 3rd ed. New York: McGraw-Hill; 2011.)
GONORRHEA
Infection with N gonorrhea may occur at any exposed site and has an incubation period of 2 to 7 days. Up to 10% of infections are asymptomatic in men as are as many as 80% in women. Urethritis is the most common manifestation of infection in men and is characterized by copious amounts of purulent urethral discharge and dysuria. Although women may also develop urethritis and dysuria, their infections more commonly manifest as cervicitis. If symptoms are present, they include vaginal irritation, discharge, or spotting, particularly with intercourse. On speculum examination, the cervix appears friable and a mucopurulent endocervical exudate may be present.
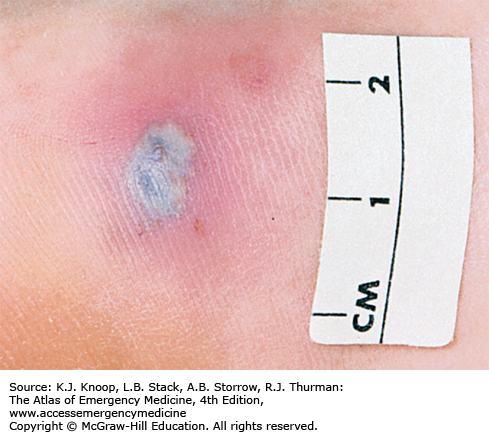
N gonorrhea infections can spread throughout the body. Disseminated gonococcal infections (DGI) occur more frequently in women. DGI most often present as a monoarticular septic arthritis of a knee, elbow, wrist, or ankle. Endocarditis and meningitis must be ruled out in any patient with DGI. A rash consisting of necrotic pustules on an erythematous base may also be present. The skin lesions may ulcerate, are more commonly found on the distal extremities, and may involve mucosal surfaces.
Ophthalmic gonococcal infections can occur in anyone but are seen most often in neonates exposed during birth. Gonococcal conjunctivitis develops within 2 to 7 days of birth and is characterized by chemosis and copious purulent exudate; untreated, these patients can develop endophthalmitis and perforation of the globe with permanent loss of vision.
Urethritis and cervicitis: Treat with a single dose of ceftriaxone 250 mg intramuscularly. Treatment with one dose of oral cefixime 400 mg orally is no longer recommended as an alternative and if used should be followed with a test of cure in 7 days.
Conjunctivitis: Treat adults with a single dose of ceftriaxone 1 g intramuscularly. Treat infants and children over 2 months of age with ceftriaxone 25 to 50 mg/kg once or use cefotaxime 100 mg/kg for those younger than 2 months; eye irrigation with normal saline as needed. All neonates should receive empiric treatment with ophthalmic erythromycin ointment at birth.
DGI: Preferred initial treatment is ceftriaxone 1 g intravenously or intramuscularly once daily for at least 7 to 10 days. Patients with suspected endocarditis or meningitis are treated with higher doses of ceftriaxone (1-2 g every 12 hours). Alternative agents for parenteral treatment are: cefotaxime 1 g intravenously every 8 hours, or ceftizoxime 1 g intravenously every 8 hours. Parenteral treatment is continued for 24 to 48 hours after symptoms improve and for a minimum of 7 to 10 days. Parenteral treatment is followed by a 7 to 10 course of oral antibiotics; cefixime 400 mg orally twice daily or cefpodoxime 400 mg orally twice daily. All sexual partners should be notified and treated empirically. Gonorrhea is a reportable disease.
Treat patients with gonorrhea for presumed concurrent infection with Chlamydia. Coinfection with these organisms is seen in 30% of men with urethritis and 50% of women with cervicitis.
Gonococcal arthritis is the most common cause of monoarticular arthritis in young, sexually active patients.
Suspect gonococcal conjunctivitis in patients with copious eye discharge and chemosis.
Cultures are the gold standard for confirming the diagnosis of DGI. Selective media should be used when specimens are obtained from the cervix, pharynx, urethra, or rectum. Nonselective medium (blood agar) should be used in culturing joint fluid, blood, or cerebrospinal fluid.
FIGURE 9.11
Female GC Urethritis. Gonococcal urethritis in a female patient. Note the purulent urethral discharge. (Reproduced with permission from Morse SA, Holmes KK, Ballard RC, Moreland AA (eds). Atlas of Sexually Transmitted Diseases and AIDS. 4th ed. Saunders Elsevier; 2010. Copyright © 2010 Elsevier, Ltd.)
CHLAMYDIA
Infections with Chlamydia trachomatis typically have an incubation period of 1 to 3 weeks. Men may develop urethritis and present with a thin, nonpurulent urethral discharge and/or dysuria. Up to 50% of men with urethritis may be asymptomatic. Men may also develop epididymitis which can cause sterility if untreated.
Women may also develop urethritis and present with dysuria. These infections can be misdiagnosed as urinary tract infection due to the presence of pyuria on urinalysis. Chlamydial cervicitis in women is usually asymptomatic and often goes undiagnosed. Chlamydial infections in women are more likely to spread to the upper genital tract and may result in pelvic inflammatory disease. This can lead to tubo-ovarian abscess formation with resultant fallopian tube scarring and other sequelae of infection that increase the woman’s risk for subsequent ectopic pregnancy. Chlamydial infections are a major cause of female infertility.
Preferred treatment is a single oral dose of azithromycin 1 g given in the emergency department. A 7-day course of doxycycline 100 mg taken orally twice daily is equally effective, but should not be used if there are any concerns about medication compliance with the longer course. Alternative treatments include a 7-day course of either ofloxacin 300 mg orally twice daily, or levofloxacin 500 mg orally once daily, or erythromycin 500 mg orally four times daily, or erythromycin ethylsuccinate 800 mg four times daily. Advise patients that their sexual partners should be examined and treated appropriately and, to reduce partner transmission, recommend sexual abstinence for 7 days.
Chlamydial infection often accompanies gonococcal infection. Empirically treat any patient being treated for gonorrhea for concurrent chlamydial infection and vice versa.
Women with chlamydial infections may be completely asymptomatic for long periods of time.
Consider syphilis serologic testing and HIV testing in patients presenting with any sexually transmitted infection.
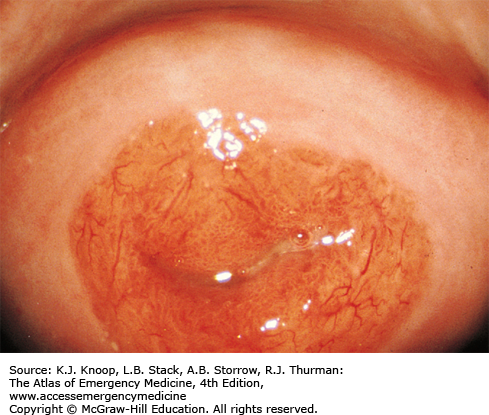
FIGURE 9.18
Chlamydia Conjunctivitis. Follicles (focal areas of conjunctival inflammation) and a thin watery discharge are seen typical of chlamydia conjunctivitis. This is usually an indolent course lasting weeks to months. Follicles and inflammation are best seen on the upper tarsal conjunctiva. (Photo contributor: Jeffrey Goshe, MD.)
GENITAL HERPES
Herpes genitalis refers to infection with the herpes simplex virus (HSV)—most commonly HSV-2. The patient may present with a symptomatic primary infection (PI), a first-episode nonprimary infection, or a recurrent episode. The majority of individuals with HSV, however, are unaware of their infection.
PI refers to the initial transfer of the virus. The patient may remain asymptomatic at this time, and may later present with a first-episode nonprimary infection. Patients who develop symptoms with the PI may experience a prodromal viral syndrome consisting of a low-grade fever and myalgias that start 1 to 3 days prior to the onset of the characteristic rash of genital herpes. This rash consists of multiple groups of small vesicles that quickly ulcerate into shallow, painful ulcers on an erythematous base. The ulcers may coalesce and form larger ulcers, especially in women. The lesions are typically intensely painful, last up to 3 weeks, and heal without scarring. Women may also experience urinary retention due to sacral autonomic dysfunction. Although the majority of PIs are relatively mild and self-limited, more serious infections can occur, especially in the immunosuppressed. Up to 10% of patients develop aseptic meningitis. Disseminated infections can also result in a diffuse rash, pneumonitis, hepatitis, and encephalitis.
The clinical presentation of first-episode nonprimary genital herpes and recurrent genital herpes is less dramatic. Systemic symptoms are usually absent and patients typically have only a single to a few painful lesions. First-episode nonprimary outbreaks resolve within 1 to 2 weeks, whereas recurrent episodes generally last less than a week. Recurrences of genital herpes are often heralded by a warning prodrome of tingling or numbness in the perineal area.
Counseling of patients with genital herpes that this is a sexually transmitted infection with a chronic and recurrent course is imperative. Evaluate all patients for other possible infections and recommend evaluation and appropriate treatment for all sexual partners. Definitive diagnostic testing includes cell culture, HSV polymerase chain reaction, and serologic testing.
Advise patients that treatment with antiviral agents can decrease the length and severity of symptoms but cannot completely eradicate the infection from the body. Antivirals may also be used for suppressive treatment for patients with frequent recurrences or immunosuppression, and decrease episodes by 70% to 80%.
Treat primary genital herpes with acyclovir, 400 mg orally three times daily, or 200 mg orally five times daily, for 7 to 10 days or until symptoms resolve. Alternatives include famciclovir 250 mg orally three times daily or valacyclovir 1 g orally twice daily for 7 to 10 days.
Figure 9.20
Herpetic Ulcerations—Female. Multiple coalescing vesicles and ulcers causing a deep ulcer. (Photo contributor: Lawrence B. Stack, MD.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree