Strategies of ventilation
Outlined below are two ventilation strategies that can be used in critically ill patients in the emergency department. Both of these strategies utilize the assist control (AC) volume cycled mode of ventilation.
Lung protective strategy (Figure 4.1)
- This strategy is designed for patients with acute lung injury (ALI) or acute respiratory distress syndrome (ARDS), or who are at risk for lung injury. The majority of patients fit into this category.
- It is believed that all intubated and mechanically ventilated patients are at risk for ALI. This strategy should therefore be employed on most critically ill patients that are on a ventilator.
- This ventilation strategy is derived from the ARDSNet study and has been shown to decrease mortality in patients with ALI/ARDS.
- It prevents VILI by avoiding over-distension of the alveoli and preventing atelectrauma.
- ARDSNet Protocol:
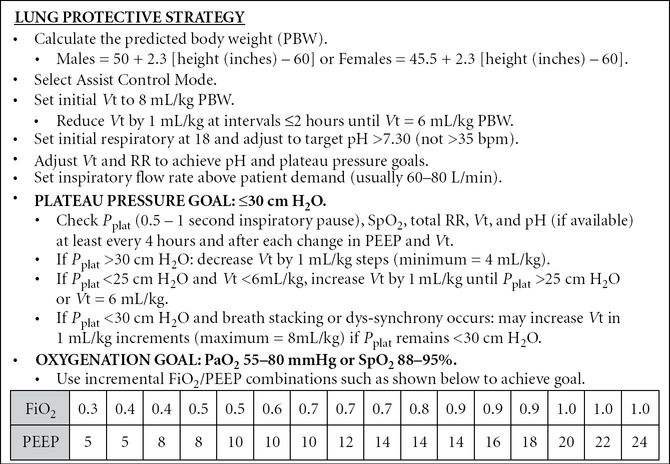
Figure 4.1. Ventilator settings for lung protective strategy. (Courtesy of Scott D. Weingart, MD.)
Obstructive strategy (Figure 4.2)
- This strategy is designed for patients with obstructive lung disease (i.e., asthma or COPD) whose airways are constricted and therefore require a longer time to fully exhale.
- They also require respiratory support for fatigued respiratory muscles during inspiration.
- The basis of this strategy is to decrease the RR and adjust the IFR to achieve a prolonged I:E ratio (1:4 to 1:5). This will allow the patient sufficient time to fully exhale and avoid auto-PEEP or breath stacking.
- Breath stacking is the phenomenon of delivering another breath before the lungs have completely exhaled. This results in an increased intrathoracic pressure and can cause a pneumothorax or hemodynamic instability secondary to a decrease in venous return.
- Decreasing the respiratory rate results in retention of CO2 which in turn leads to a respiratory acidosis. This is referred to as permissive hypercapnia and is tolerated to a certain extent (PaCO2 <85 mmHg and pH >7.20).
Figure 4.2. Ventilator settings for obstructive strategy. (Courtesy of Scott D. Weingart, MD.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







