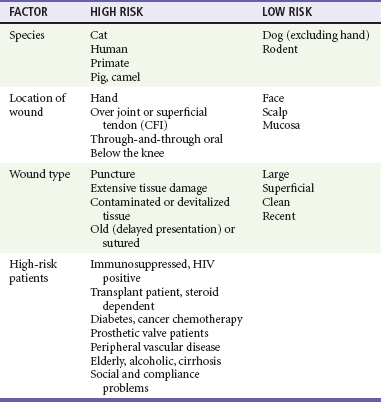
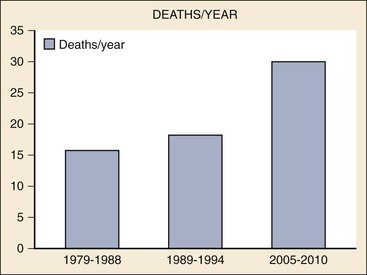
Chapter 61 Reliable statistics on animal bites are hard to come by, as many bites are not reported. The Centers for Disease Control and Prevention (CDC) in the United States currently estimates that 4.5 million dog bites occur per year, affecting nearly 1.5% of the population, but only 20% (885,000) of victims seek medical attention.1 Emergency department (ED) visits for dog bites decreased 14% between 2001 and 2008, but hospital admissions for dog bite–related injuries increased 86% from 1993 to 2008, with 9% of patients requiring some type of surgical repair.2 Fatalities from dog bites increased 92% from 1992 to 2010 to a rate of 30.2 deaths per year (Fig. 61-1).3–5 The majority of fatalities occur in children younger than 10 years, with children younger than 4 years at greatest risk of death; those older than 50 years also have a higher fatality rate.6 The breeds most frequently responsible for fatalities include pit bull (59%), Rottweiler (14%), American Bulldog and Siberian Husky (5% each), and German Shepherd Dog (3%), followed by 14 other breeds with one or two fatalities each year.1,7 The majority of fatalities involved an unrestrained dog on the owner’s property (59%).8 Figure 61-1 Fatal dog bites in the United States; 90% increase (40% corrected for population growth). The incidence of bites from species other than dogs is harder to ascertain. Some government reports combine statistics on mammalian bites with those on bites from reptiles and insects or marine envenomations. Geographic differences in incidence add to the challenge. The cat bite generally appears as the second most common animal bite injury in the United States,9,10 accounting for 5 to 15% of domestic animal bites.9 Most cat bites occur in or near the home, and the perpetrators are pets rather than strays (more than 80%). Whereas victims of dog bite injuries are more often male,1,11,12 females are twice as likely as males to be victims of cat bites, with a peak age incidence in the third decade.9 Rodent bites are probably the third most common animal bite, representing up to 7% of the total in the United States. Bites from other species combined (monkeys, ferrets, raccoons, foxes, livestock, bats, minks, and other wild animals) total less than 2% of all bites.13,14 Epidemiology changes with locale. In India, for example, dog bites (92%) are followed by monkey bites (3.2%), cat bites (1.8%), and fox bites (0.4%) in terms of frequency.14 Bites can cause damage to skin, muscle, blood vessels, nerves, tendons and tendon sheaths, joints and joint spaces, and bony structures. Some bites involve major trauma and fatalities.15 The head and neck are areas of particular vulnerability in children younger than 4 years.16 Less serious, but far more frequently, bite injuries involve contusions, abrasions, lacerations, avulsions, or puncture wounds. Secondary considerations in all of these animal bite wounds involve contamination with oral flora from the biting animal and local infection. The potential for tetanus or rabies exposure must also be considered. Tetanus is discussed in Chapter 59, and rabies is covered in Chapter 131. Dog bite force can exceed 310 pounds, although most bites use much less force.17,18 Total bite force generated increases as the size of the animal skull increases.17 Dog bites may cause relatively superficial tearing, or crush injuries that damage skin, subcutaneous tissues, and occasionally muscle and far less commonly tendons, bones, or joints. The wounds may be contusions or ecchymoses without a break in the skin but more commonly are abrasions, lacerations, avulsions, or large gaping crush wounds. A study of more than 2000 dog bites found that most injuries were superficial and most of the patients were treated with simple medication, dressing, or suturing.19 Face, scalp, and neck wounds occur most commonly in young children.6,19 In children up to 2 years old, there are case reports of dog bites that have perforated the skull, resulting in open depressed fractures, brain laceration, intracranial abscess, and meningitis.20 The trauma associated with dog bite injuries has led to residual post-traumatic stress disorder (PTSD) in children. In victims older than 15 years, more than 80% of dog bite injuries are on the extremities,16 with the lower extremities more frequently involved.6,19 In adults, dog bites rarely result in fracture, vascular injury, or tendon and nerve damage, but there have been cases of tendon lacerations and purulent tenosynovitis.21 Bites from police dogs that are trained to hold their grasp until given the release command have a much higher risk of causing damage to deeper structures, in particular vascular injury; tendon and nerve injury, as well as fracture and infection, are all more common in bites from police dogs than from civilian dogs.22 The incidence of infection from dog bites has historically been quoted as 5 to 15%,16,23 similar to the overall infection rate of 7% in nonbite lacerations. More recent work suggests a nonbite laceration infection rate of 3 to 4%,24 and a recent controlled study of dog bite lacerations showed a baseline infection rate of 2% in the control arm.25 The type of wound appears to influence infection rates, with avulsions at 3%, lacerations at 6%, and puncture wounds the highest at 7%.26 In one study of infected bite wounds, 60% were punctures, 10% lacerations, and 30% a combination of the two.27 Location on the body also affects risk; dog bites on the hand have a higher rate of infection, and bites of the face have a lower risk than bites elsewhere.23,26 Bacteriology: More than 100 different organisms have been isolated from infected dog bites. Most infected wounds are polymicrobial, with an average of five isolates per wound, including both aerobic and anaerobic species.16,27 No single organism was responsible for more than 30% of infections.28,29 Staphylococcus aureus, alpha-hemolytic and beta-hemolytic streptococci, Klebsiella, Bacillus subtilis, Pseudomonas, Enterobacteriaceae, and Capnocytophaga canimorsus are among the frequently isolated aerobic organisms.27,30 Anaerobic organisms isolated from infections include Bacteroides, Fusobacterium, Peptostreptococcus, Porphyromonas, and Prevotella species.16 Although much attention has been focused on Pasteurella multocida, its role in causing infections in dog bites may be overestimated.29,31 P. multocida is found in the oral flora of 77% of cats but only 13% of dogs.32 Pasteurella species are isolated in 25 to 50% of infected dog bite wounds, although one study of infected dog bites found no Pasteurella.27,33 The Pasteurella species that have been isolated from dogs, such as Pasteurella stomatis, Pasteurella canis, and Pasteurella dagmatis, are less virulent varieties.27,32 When P. multocida is isolated from infected dog bites, it is frequently found in mixed culture with other organisms; with infected cat bites, however, P. multocida is often the sole pathogen.33 Capnocytophaga canimorsus: C. canimorsus is a fastidious gram-negative rod that can cause overwhelming sepsis. It is part of the normal oral flora of both dogs and cats. More than 100 cases have been documented since the organism’s discovery in 1976.34,35 About 90% of cases are attributed to contact with a dog, primarily bites or scratches, but for approximately one quarter of infections, only dog contact (without a bite) is documented. A few infections have resulted from contact with cats. About 10% of cases appear unrelated to animal exposure. The disease tends to strike patients with alcoholic liver disease, functional or surgical asplenia, or lung disease or those taking corticosteroids. However, in 40% of victims, no underlying illness is identified.34,36 The illness usually begins within 3 days of exposure (range 1-10 days). Early manifestations include fever, chills, myalgias, and vomiting.37 The clinical picture on presentation is often that of sepsis, with hypotension, renal insufficiency, and disseminated intravascular coagulation (DIC). Purpura, particularly on the face, and petechiae are frequent findings and may progress to symmetrical peripheral gangrene.38 Cutaneous gangrene at the site of the bite strongly suggests C. canimorsus.39 Waterhouse-Friderichsen syndrome (adrenal hemorrhage) may occur, as well as metastatic infection, with endocarditis, meningitis, or peritonitis. The mortality rate is 30%, with 70% of deaths occurring in immunocompromised patients.37,39 C. canimorsus grows slowly and requires special media and growth conditions. In cases of sepsis without an obvious source when contact with a dog or cat has occurred, C. canimorsus should be considered, and the laboratory should be notified to prevent cultures from being misidentified or discarded prematurely.37 Although cultures may take up to 14 days, the organism can sometimes be identified in the patient’s blood smear at the time of presentation, or in blood culture media before macroscopic growth.39,40 Polymerase chain reaction (PCR) has recently proven valuable in C. canimorsus identification.41,42 Cat bite injuries contrast sharply with dog bites in their propensity for infection and injury to deeper structures. The typical cat bite is a puncture wound, but abrasions, lacerations, and avulsions may also occur. Cats have long, slender, pointed teeth that can penetrate tendons, joints, and bone, inoculating bacteria deep into these tissues. The majority of these bites involve the hand and upper extremity.9,23 The puncture wound itself often can be difficult to explore, irrigate, or débride. Cat bites are also more likely than dog bites to become infected.23,43 The incidence of infection in untreated cat bites is reported to be as high as 67%, although this probably represents an overestimate as many patients seek treatment only after infection has developed.26,44 One prospective ED study of patients with cat bites found an infection rate of 16%, and most infections were present when the patient first sought care.9 In addition to generally recognized patient risk factors for infection, predictive factors for cat bite infection also include wound type, depth of penetration, and delay in seeking care. Bacteriology: A bacteriologic analysis of infected cat bites found a median of five bacterial isolates per culture (range, 1-16), with mixed aerobic and anaerobic bacteria in 63%. Aerobic isolates alone grew in 32% of infected cat bites, and there were no infections caused solely by anaerobes. The most common pathogens were P. multocida and Pasteurella septica, found in 75%, but streptococci, staphylococci, Moraxella, and Bacteroides were also isolated among the aerobic pathogens. Anaerobes included Bacteroides, Fusobacterium, Porphyromonas, and Prevotella. Only 4% of the cat bite isolates included S. aureus, and no Streptococcus pyogenes isolates were detected, suggesting the wounds were more heavily contaminated with oral flora of the biting animal rather than the skin flora of the victim.27 Pasteurella multocida: An important factor contributing to the risk of infection after cat bites is the presence of P. multocida, a highly virulent, facultatively anaerobic, gram-negative rod found in the oral cavity or nasopharynx of 70 to 90% of healthy cats.32 Wound infections and abscesses caused by P. multocida have occurred after cat scratches as well as cat bites and less often after dog bites or open wounds that have been licked by dogs.31 P. multocida infections have also been reported after the bite of an opossum, rat, lion, rabbit, pig, wolf, monkey, and cougar.45–47 P. multocida wound infections often have an earlier onset than typical skin organisms, causing a rapidly progressive cellulitis apparent within 6 hours and easily identifiable within 24 hours.27 Presenting features include erythema, warmth, swelling, and tenderness, and often purulent drainage, lymphangitis, and adenopathy. In addition to cellulitis, P. multocida can cause abscess, tenosynovitis, joint infections, and osteomyelitis at the site and may seed arthritic joints and prosthetic valves, causing septic arthritis, endocarditis, and osteomyelitis at distant sites. Meningitis and pericarditis caused by P. multocida after a bite have also been reported.48,49 In vitro, P. multocida is sensitive to penicillin, ampicillin, tetracycline, fluoroquinolones, amoxicillin-clavulanate, second- and third-generation cephalosporins, and trimethoprim-sulfamethoxazole (TMP-SMX).50,51 For prophylaxis, Pasteurella species are considered susceptible to all of the agents previously listed, plus doxycycline, clarithromycin, and azithromycin.16,51 The organism is resistant to vancomycin, clindamycin, and oral first-generation cephalosporins and shows borderline susceptibility to aminoglycosides.52 Semisynthetic penicillins, such as dicloxacillin, have only minimal activity against P. multocida in vitro, and erythromycin is also a relatively poor choice.50,51 Primates: In the United States, monkey bites appear most commonly in university centers in laboratory workers who have sustained work-related injuries. Primate bites are said to have a high wound infection rate. The infecting organisms have not been well described, with the exceptions of one wound infection caused by Eikenella corrodens and a case of osteomyelitis caused by P. multocida.47,53 The major concern with monkey bites is B virus exposure. Only one of the 35 herpesviruses identified in nonhuman primates, cercopithecine herpesvirus 1, or B virus, causes disease in humans. Other terms for this virus include herpesvirus simiae, herpesvirus B, and monkey B virus. The virus has serologic cross-reactivity with herpes simplex virus (HSV) type 1 and type 2, which cause herpetic lesions in humans.54 Monkeys of the genus Macaca (macaques) can carry B virus throughout their lives, and B virus disease in monkeys resembles that of human herpes viruses. Asymptomatic infected monkeys harbor the virus in their conjunctiva, buccal mucosa, and genital areas55 and may shed virus but are more likely to do so when ill, under stress, immunocompromised, or breeding. More than 40 cases of B virus infection in humans have been reported, all in laboratory workers bitten or scratched by monkeys or sustaining local injury from animal cages. Many exposures were considered trivial at the time of injury.55,56 B virus can enter the victim host cells within 5 minutes, making immediate wound care at the scene (soap and water scrub) the most important step in prevention of transmission.16 The incubation period may range from 2 days to 5 weeks, but most human cases manifest within 5 to 21 days, with initial symptoms of paresthesias at the site of the bite, soon followed by a vesicular rash and, if untreated, by encephalitis and coma. The case fatality rate is approximately 70%.55 Treatment with intravenous acyclovir is most successful if begun when local vesicles first appear,56 but even after central nervous system symptoms develop, aggressive treatment may allow survival.55 Rodents: Rodent bites cause small puncture wounds with a low risk of local wound infection. These bites are frequently seen in laboratory workers, in children in lower socioeconomic areas who are bitten while sleeping, and occasionally in pet owners.57 A number of diseases may be transmitted by rodent bites or scratches, including rat-bite fever, leptospirosis, tularemia, sporotrichosis, murine typhus, and plague, although nonbite contacts are the more common routes of transmission of systemic disease to humans. Rat-bite fever, caused by Streptobacillus moniliformis or Spirillum minus, is rare. It usually manifests 1 to 3 days after the bite with abrupt onset of fever, chills, myalgias, and headache, followed by a rash. Abscesses form in many tissues, including brain, myocardium, and soft tissues. Involvement of joints occurs in 50% of patients, resulting in an asymmetrical migrating polyarthritis.58,59 Penicillin is the antibiotic of choice, and the organisms also have sensitivity to erythromycin, cephalosporins, tetracycline, carbapenems, aztreonam, clindamycin, and vancomycin. There is intermediate sensitivity to aminoglycosides, fluoroquinolones, and chloramphenicol, with resistance to TMP-SMX, polymyxin B, and nalidixic acid.58 Routine prophylaxis is unnecessary, as there is a low rate of wound infection.16 Ferrets: The European ferret (Mustela putorius furo) is the third most popular pet in the United States, with an estimated 5 to 7 million pet ferrets in 4 to 5 million households. The ferret is descended from the polecat, a member of the weasel, mink, and wolverine family. Hunters previously bred ferrets to hunt rats and rabbits. They are extremely ferocious and tenacious with their prey. Although domesticated for more than 2000 years, the ferret appears to retain its instinctive propensity for attacking suckling animals and an attraction to the neck of its victim. Ferrets are known to attack infants and young children suddenly and without provocation, even in the presence of an adult. They usually attack the face and neck and often have to be pried off the victim. Extensive cosmetic repair after such attacks has been required.60,61 Domestic Herbivores: The bites of horses may result in severe soft tissue contusions and abrasions, often involve the limbs, and may lead to soft tissue infections with Staphylococcus, Pasteurella, Yersinia, Actinobacillus, Burkholderia, and Rhodococcus species.62 Some 1800 patients per year visit EDs with horse bite injuries, and on rare occasions, these bites result in systemic infection.63 Streptococcus equi subsp. zooepidemicus is one of the group C streptococcal species that are common pathogens and is associated with the equine respiratory infection known as strangles but may also be carried by healthy animals.64 It has been reported to cause meningitis in humans. Cattle do not have upper incisors, so they virtually never bite. Pig bites, on the other hand, are often deep and may appear deceptively small on the surface.65 They require careful exploration and débridement. Pathogens include Pasteurella aerogenes, P. multocida, Escherichia coli, Bacteroides, Proteus, and alpha- and beta-hemolytic streptococci.45,65 Despite antibiotics and appropriate wound care, pig bites have a high risk of infection. Most domestic herbivores carry P. multocida. Bacterial isolates from these animals are often resistant to common antibiotics, which has been attributed to the practice of adding antibiotics to their feed. Camels are well known for biting their handlers, reportedly in sudden vengeance for offenses committed previously. Unlike most other herbivores, the camel has canine teeth and can cause deep wounds, fractures, and amputations, most involving the handler’s upper limbs. These wounds are reported to have a very high rate of infection.66,67 Wild Animals: Human encounters with large wild animals, such as wolves, coyotes, large cats, elephants, or bears, may result in massive trauma and death, from some combination of biting, goring, or trampling. Attacks by such animals may cause blunt or penetrating trauma, with major arterial blood loss, airway damage, intracranial penetration, broken ribs and vertebrae, pneumothoraces, and intraperitoneal bleeding.20,68 Hyenas are known for their tremendously strong jaws and for their attacks on humans in Africa. Hyenas target the face and can deglove a face or decapitate a human. Bites of bears usually result in multiple punctures, with crushing and tearing of soft tissues, and underlying fractures of facial bones and those of the upper extremity. Big cats tend to attack the nape of the neck; their teeth may enter the pharynx, esophagus, and intervertebral space. A common killing mechanism is to shake the victim by the neck.68 The organisms involved in wild animal bites include staphylococci, streptococci, and anaerobes, similar to bites from domestic animals.16 As with nonbite lacerations, the location, type of wound, time to treatment and patient factors contribute to the risk of wound infection.69,70 Dog bites in patients who delay care by as little as 6 hours have an increased risk of becoming infected.43,70 Certain patient comorbidities increase bite wound infection risk. Asplenia, cirrhosis, lung disease, and steroid use all increase the risk of Capnocytophaga infections. The risk of Pasteurella infections is increased in patients with alcoholism, rheumatoid arthritis, or diabetes mellitus, those taking steroids, and those who have residual lymphedema after radiotherapy70 (Table 61-1). Bite injuries, particularly those from monkeys with potential exposure to herpesvirus simiae (B virus), should be immediately cleansed with soap and water at the scene.16,54 Washing the wound with soap and water, ideally with the use of a fine-pore sponge to minimize additional tissue trauma, also substantially decreases the risk of rabies infection if done within 3 hours.71 Key elements of the history include the circumstances of the bite, type of animal, animal immunization status against rabies, animal behavior, and whether the animal is available for observation. Specifically ask about comorbidities with risk of poor wound healing (e.g., diabetes, peripheral vascular disease); use of immunosuppressive medications or steroids; history of splenectomy; chronic alcoholism, particularly with malnutrition; and parenteral recreational drug use. Assess the tetanus status, medication allergies, and primary care provider availability.72 Potential language, cultural, or economic barriers to compliance are additional considerations.14 Active bleeding is controlled with direct pressure. If necessary, a temporary 3-0 nylon suture on a large needle may be used. Intractable bleeding on an extremity may be controlled with a proximal blood pressure cuff inflated above the systolic pressure for up to 20 minutes. The general principles of wound management apply to these patients (see Chapter 59). Radiographs are usually not necessary but may be considered when there is the possibility of bony injury or foreign body. Infants and children up to 2 years old who sustain substantial bite wounds to the scalp may require computed tomography (CT) imaging.20 In most situations, exploration with local anesthesia or procedural sedation will be critical. The importance of adequate visualization of the depths of the wound cannot be overstated, as this may be the sole opportunity to detect a foreign body or a deep structure injury that could otherwise be missed and manifest later with increased morbidity. In the absence of deep structure injury, wound irrigation followed by conservative débridement is recommended. There is no evidence that extension of the wound to promote irrigation diminishes the chance of infection. Much controversy and few data surround the question of suturing animal bites. Sound practice dictates that when a wound is at high risk for infection, it should not be sutured unless there is evidence of its safety or other compelling reasons. One study of 145 sutured bite wounds (dog, cat, and human) found a rate of infection of approximately 6%. The use of antibiotics was not standardized.73 This infection rate may be acceptable in lacerations for which cosmesis is a primary concern. To date, only dog bites have had controlled studies to address the issue of primary closure.43 The infection rate in 169 wounds was the same for sutured bites as for those left to heal by secondary intention (7.7%). Dog bites on the hand had a higher infection rate (12%), but there was no significant difference between sutured and unsutured wounds. Other studies have demonstrated an equivalent infection rate for sutured dog bites and unsutured wounds.29,74 On the face, sutured dog bite wounds have a very low infection rate, even when punctures are sutured and no prophylactic antibiotics used.75 The following guidelines are suggested, even though data are limited (Table 61-2). Bite wounds of the face and scalp from any species that are less than 6 hours old may be irrigated and sutured. It is probably safe to suture most other uncomplicated dog bites. Lower extremity and hand wounds are at higher risk for infection and should rarely be sutured. Cat bites and primate bites should not be sutured in locations other than the face and scalp. Puncture wounds, contaminated wounds, wounds more than 12 hours old, or wounds infected at presentation should not be sutured. Patients at risk for infection or poor wound healing are best treated conservatively without suturing. See Chapter 59 for a discussion of wound healing with delayed primary closure. No current evidence shows that topical adhesive closure as opposed to sutures changes the rate of infection. Table 61-2 Recommendations for Bite Wound Closure and Prophylactic Antibiotic Consideration *High-risk wounds: hand wounds, deep structure involvement (tendon, joint, bone), delayed presentation (>12 hours), contaminated wounds with foreign bodies or devitalized tissue, deep puncture wounds, high-risk patients (see Table 61-1).
Mammalian Bites
Animal Bites
Epidemiology
Principles of Disease
Dog Bites
Cat Bites
Other Mammals
Infection Risk Factors
Management
SPECIES
SUTURING
PROPHYLACTIC ANTIBIOTICS
Dog
All (except hands)
High-risk wounds only* (all hand wounds)
Cat
Face only
All
Human
Face (as needed)
Hand, especially CFI
Monkey
No
Yes
Pig, camel
Face (as needed)
Yes
Rodent
Yes (rarely needed)
No
Hand bites
No
Yes
Other locations
Yes
High-risk wounds only*
Mucosa
Yes (as needed)
No
Oral through-and-through bite
Yes (as needed)
Yes
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Mammalian Bites
Only gold members can continue reading. Log In or Register to continue