Fig. 21.1
Prefilled dental local anesthetic cartridges. 2.2 mL, 1.8 mL, 1.0 mL

Fig. 21.2
Dental local anesthetic syringes
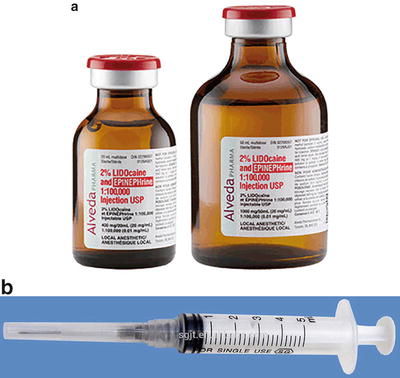
Fig. 21.3
(a) Lidocaine 2 % with epinephrine 1–100,000 multidose vial. (b) Plastic disposable syringe
Local anesthetic techniques vary according to the site of the planned treatment. In the maxilla, the cortical plate of bone overlying the teeth is usually quite thin, permitting the use of ‘infiltration’ anesthesia (also known as ‘supraperiosteal ’). Infiltration of a small volume of local anesthetic (0.6 mL) at or above the apex of the tooth to be treated effectively blocks nerve conduction. Infiltration is the most common dental injection and is recommended when one maxillary tooth is to be treated. Nerve blocks, such as the anterior superior alveolar and posterior superior alveolar, may be administered when multiple maxillary teeth are to be treated. A local anesthetic nasal mist often tracaine and oxymetazoline (Kovanaze) allows for treatment of maxillary anterior teeth (preolars, canine and incisors) without the need for injection [6].
The adult mandible presents a different situation. The cortical plate of bone overlying the mandibular teeth in the adult is usually quite dense, preventing the simple infiltration injection from proving effective. Nerve block administration is the ‘norm.’ The traditional inferior alveolar nerve block (IANB ), as described by Halsted in 1885, remains the most commonly used mandibular technique , providing anesthesia to all eight teeth in the quadrant. The incisive (mental) nerve block may be used when treating teeth anterior to the mental foramen (premolars, canine, and incisors). Other techniques include the Gow-Gates mandibular nerve block [7], Akinosi–Vazirani (closed mouth) nerve block [8, 9], periodontal ligament (PDL) injection [10], and intraosseous (IO) [11].
As with any technique, complications—though rare—can and do occur. Within dentistry localized complications associated with intraoral injections include needle breakage, paresthesia, facial nerve paralysis, and self-inflicted soft tissue injury, among others. Systemic complications include allergy and overdose (toxic reaction). Fortunately, the incidence of true, documented, and reproducible allergy to amino-amide local anesthetics is exceedingly rare. However, overdose is a potential problem seen most often in the younger, lighter weight (<30 kg) patients undergoing multiple quadrants of treatment in a single visit [12]. The following sections of this chapter will discuss these topics in greater detail.
Dental Local Anesthetic Formulations
In the United States, there are five different local anesthetic formulations available in a total of nine preparations which are used in dentistry and packaged in single use, disposable dental cartridges [13]. They are as follows:
- 1.
Articaine
- 2.
Bupivacaine
- 3.
Lidocaine
- 4.
Mepivacaine
- 5.
Prilocaine
Articaine
It is available as a 4 % solution in dental cartridges with 1:100,000 epinephrine and 1:200,000 epinephrine. This drug is an amide-ester hybrid unlike all other local anesthetics used in dentistry that are pure amides. As such, articaine possesses a degree of hepatic biotransformation which leads to a beta (elimination) half-life that is significantly shorter (27 min) than other amide anesthetics (≥90 min) [14]. Since local anesthetic manufacturers have adjusted the concentration of each local anesthetic such that 1 mL of drug “A” is equipotent to 1 mL of drug “B,” articaine represents the least potent local anesthetic available in dental cartridges as it is available as a 4 % concentration [13]. Articaine provides pulpal anesthesia of about 1 h and soft tissue anesthesia of 3–5 h duration, making it a reasonable choice for most dental procedures [15]. Articaine is approved for use in patients age 4 years and older [16].
Bupivacaine
It is available in dental cartridges as a 0.5 % solution with 1:200,000 epinephrine [17]. As a 0.5 % solution, bupivacaine is the most potent local anesthetic routinely used in dentistry. Being 95 % protein bound, it is a long-acting local anesthetic with pulpal anesthesia, following nerve block, in the 4–6 h range and soft tissue anesthesia that may exceed 12 h. Bupivacaine has the highest pKa of all of the local anesthetics used in dentistry making it the local anesthetic with the slowest onset of action [14]. While it is true that bupivacaine is four times as toxic as lidocaine , as packaged in dental cartridges they are equitoxic and equipotent per mL injected [17, 18]. Because the maximum recommended dose of bupivacaine in dentistry is significantly less than in medicine (Table 21.1) and because local anesthetics in dentistry are never intentionally injected into a vein (careful aspiration should always be performed), the cardiotoxic concerns that are present in medicine are not an issue in dentistry.
Table 21.1
Maximum dosages for local anesthetics
Maximum dosages for local anesthetics (all local anesthetic data derived from the associated package insert and FDA approved) | |||
|---|---|---|---|
Agent | MG/cartridge | Maximum dose (mg/kg) | Maximum dose (mg) |
2 % lidocaine (Xylocaine ®) with 1:100,000 or 1:50,000 epinephrine | 36 | 7 | 500 |
2 % mepivacaine with 1:20,000 levonordefrin (Carbocaine®, Polocaine, Scandanest, Isocaine®) | 36 | 6.6 | 400 |
3 % mepivacaine plain (Carbocaine®, Polocaine, Scandanest, Isocaine®) | 54 | 6.6 | 400 |
0.5 % bupivacaine with 1:200,000 epinephrine (Marcaine®, Vivacaine®)a | 9 | – | 90 |
4 % articaine with 1:100,000 or 1:200,000 epinephrine (Septocaine®, Zorcaine®, Articadent®, Orabloc®)b | 72 | 7 | – |
4 % prilocaine with 1:200,000 epinephrine (Citanest Forte®) | 72 | 8 | 600 |
4 % prilocaine plain (Citanest®) | 72 | 8 | 600 |
Lidocaine
It is the most used local anesthetic in dentistry and since its introduction in 1948 has remained the “gold standard” for dental local anesthetics [19]. It was this drug that displaced the mighty “Novocain ®” (procaine) almost 70 years ago. As a side note, no formulation containing procaine has been available in dental cartridges since the 1990s [20]. In the United States, lidocaine is available in dental cartridges as a 2 % solution with 1:100,000 epinephrine and 1:50,000 epinephrine. Lidocaine without a vasoconstrictor (“plain”) was manufactured for quite some time but has not been available in dental cartridges for a number of years. Lidocaine is intermediate in both potency and duration of action; it provides pulpal anesthesia for about 1 h and soft tissue anesthesia of 3–5 h making it very similar in duration to articaine but twice as potent [18].
Mepivacaine
It is different than all other local anesthetics used in dentistry for two significant reasons. First, it is the only local anesthetic available in two different concentrations, 2 and 3 %. Second, it is the only local anesthetic marketed in the United States in dental cartridges with a vasoconstrictor other than epinephrine. Two percent mepivacaine is available with 1:20,000 levonordefrin (NeoCobefrin®) [21]. Levonordefrin has a different profile than epinephrine with respect to receptor pharmacology. Epinephrine has roughly a 50:50 affinity between alpha (α) and beta (β) receptors. Levonordefrin is roughly 75:25 weighted toward alpha with significantly less beta effect. Additionally, levonordefrin is roughly 1/6 as potent as epinephrine [14]. Three percent mepivacaine is only available without a vasoconstrictor (“plain”). Mepivacaine plain is a short duration drug where mepivacaine with vasoconstrictor is intermediate, similar to articaine and lidocaine . Mepivacaine has the lowest pKa of all local anesthetics used in dentistry making it the local anesthetic with the fastest onset of action [21].
Prilocaine
It is available as a 4 % solution in dental cartridges, either with 1:200,000 epinephrine or plain (without vasoconstrictor). Prilocaine plain competes with mepivacaine plain with respect to duration of action, albeit with a slightly slower onset of action, though this is not clinically significant. Prilocaine with vasoconstrictor has a similar onset of action and duration of action of articaine , lidocaine , and mepivacaine [22].
Techniques of Dental Local Anesthesia
Maxillary Injection Techniques
Supraperiosteal (Infiltration) Injection
The supraperiosteal (or infiltration) technique can be used to anesthetize teeth and the surrounding soft tissue adjacent to the injection site. Penetration is the height of the mucobuccal fold parallel to the tooth to be treated. The depth of penetration is approximately 2–5 mm (the needle tip is located at or above the apex of the tooth). After careful aspiration, 0.6 mL of solution is slowly deposited. This technique is recommended for procedures limited to the treatment of one or two teeth [23].
Anterior Superior Alveolar Nerve Block
The anterior superior alveolar (ASA) nerve block (NB) will anesthetize the buccal soft tissue and teeth from the canine to the midline [24] (Fig. 21.4). The depth of penetration is about 16 mm in the mucobuccal fold over the maxillary first premolar. Slow deposition of 1.0 mL of solution after aspiration is generally sufficient [23–26]. Crossover innervation must always be considered in case of inadequate anesthesia near the midline.
Fig. 21.4
Anterior superior alveolar nerve block ((a) area anesthetized; (b) needle placement)
Middle Superior Alveolar Nerve Block
The middle superior alveolar (MSA) NB will anesthetize the mesiobuccal aspect of the maxillary first molar, both premolars, along with the soft tissue lateral to this area [24] (Fig. 21.5). Penetration for the MSA NB is at the height of the buccal vestibule lateral to the maxillary second premolar. The needle tip should approximate the apex of the tooth, which usually requires a penetration of about 5 mm. After careful aspiration, 1.0 mL of anesthetic solution is slowly deposited [23–26]. Note: The MSA nerve is absent in approximately 28 % of patients. If this is the case, the anterior superior alveolar (ASA) NB will anesthetize the premolar region.
Fig. 21.5
Middle superior alveolar nerve block
Posterior Superior Alveolar Nerve Block
The posterior superior alveolar (PSA) NB will anesthetize the three maxillary molars except for the mesiobuccal aspect of the first molar (Fig. 21.6) and the buccal soft tissue adjacent to these teeth [24]. The PSA NB is administered with the insertion point at the height of the buccal vestibule at a point just distal to the malar process. The needle is inserted distally and superiorly at approximately 45° to the mesiodistal and buccolingual planes. The depth of insertion is approximately 15 mm, and following careful aspiration, 1.0 mL of solution is slowly deposited [23, 26].
Fig. 21.6
Posterior superior alveolar nerve block ((a) area anesthetized; (b) technique)
Greater Palatine Nerve Block
The greater palatine (GP) NB will anesthetize the tissues of the hard palate anteriorly to the distal of the canine and laterally to the midline (Fig. 21.7) [24]. The entrance to the greater palatine foramen may be palpated as a depression or soft spot in the posterior area of the hard palate. It is usually located halfway between the gingival margin and the midline of the palate, approximately opposite the distal of the maxillary second molar [23–26]. Anatomically, this is generally 5 mm anterior to the junction of the hard and soft palates. The most comfortable way to perform this injection is to first deposit 0.3 mL of local anesthetic in the soft tissue around the location of the greater palatine foramen. Penetration will occur through the epithelium, and the needle will appear to “fall into” a space of less resistance. The needle should be inserted until bone is contacted. The depth of penetration is variable, but usually less than 5 mm is sufficient. After aspiration, 0.5 mL of anesthetic solution is very slowly deposited.
Fig. 21.7
Greater (anterior) palatine nerve block ((a) area anesthetized; (b) technique)
Nasopalatine Nerve Block
The nasopalatine (NP) NB will anesthetize the tissues of the palatal aspect of the upper anterior teeth [24] (Fig. 21.8). The entrance to the nasopalatine foramen is at the incisive papilla, which may be visualized posterior to the maxillary central incisors. The needle tip should contact soft tissue at the lateral aspect of the incisive papilla with a depth of penetration of <5 mm and bony endpoint. Approximately 0.25 mL may be very slowly introduced after aspiration [22–24, 26]. Note: Some patients also have a contribution from this nerve to the pulpal tissue of the maxillary incisors.
Fig. 21.8
Nasopalatine nerve block ((a) area anesthetized; (b) technique)
Maxillary (V2) Nerve Block
The entire maxillary (second) division of the trigeminal nerve (cranial nerve V) is anesthetized most frequently via the greater palatine canal (Fig. 21.9). The V2 nerve block anesthetizes the maxillary teeth and periodontium, hard and soft palates, sinuses, and portions of the nose, orbit, upper cheek, lower eyelid, and side of the face on the ipsilateral side [24]. The entrance to the foramen is located at the distolateral aspect of the same depression felt during palpation before the greater palatine injection. This foramen generally is located halfway between the gingival margin and the midline of the palate, approximately 5 mm anterior to the junction of the hard and soft palates. After 0.3 mL of local anesthetic is given in the soft tissue, a long needle is used to probe the canal entrance gently. Angulation is mostly superior, with slight distal and lateral components [23–26]. The most effective position of the needle for administration of the V2 block injection generally is such that a 45-degree angle exists between the needle and the soft tissue. The needle is inserted to a depth of approximately 30 mm. After aspiration, the contents of the cartridge (1.8 mL) are slowly deposited [27]. Up to 15 % of patients have anatomical deviations that make this approach ineffective , because the needle cannot physically be manipulated up the canal to the proper depth.
Fig. 21.9
Maxillary (V2) nerve block. Greater palatine canal approach ((a) area anesthetized; (b) anatomy; (c) technique)
Mandibular Injection Techniques
Inferior Alveolar Nerve Block
The inferior alveolar (IA) NB will anesthetize the mandibular teeth from the third molar to the midline, the buccal soft tissue from the premolars anteriorly, the body of the mandible, the periosteum, the PDL, and the skin and subcutaneous tissues of the chin and lower lip, all on the ipsilateral side (Fig. 21.10) [28]. In an IA block, a long needle is positioned parallel to the mandibular occlusal plane from the contralateral premolar area to a point on the soft tissue approximately 1.5 cm above the mandibular occlusal plane. Traditionally, the IA injection is described with an insertion point 1.0 cm above the mandibular occlusal plane. The use of a 1.5 cm puncture point should increase the success rate from approximately 84 % to 96 % [29]. The mucosa is pierced at a point between the pterygomandibular raphe and the deep tendon of the temporalis muscle, and the needle is advanced until bone is contacted, usually about 25 mm [24–26, 28]. The best way to visualize the lateral positioning of the needle prior to penetrating soft tissue is to look for the depression seen on the immediate lateral aspect of the pterygomandibular raphe. This is sometimes termed the “poke me line” (Fig. 21.11). Once the needle is advanced and bone contacted, the tip should now be located just superior to the lingula. The needle should be withdrawn 1–2 mm so it is no longer in contact with periosteum. After careful aspiration, 1.5 mL of solution is deposited. As the needle is being removed, when it is approximately halfway out, the lingual nerve is injected with the remaining solution, unless a buccal nerve block needs to be done. In that case, a few drops of local anesthetic should be reserved. Frequently, even without this last step, the lingual nerve will be anesthetized. A potential complication of this nerve block is an intravascular injection because it has the highest frequency of positive aspiration of all intraoral injections (10 %-15 %). Careful aspiration can avoid this complication.
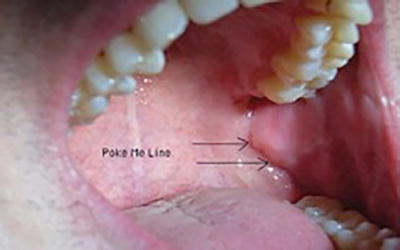
Fig. 21.10
Inferior alveolar nerve block ((a) area anesthetized; (b) technique)
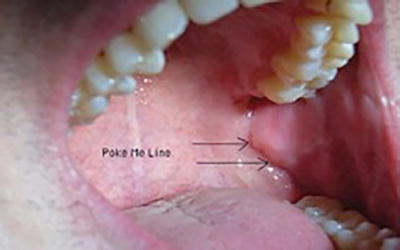
Fig. 21.11
‘Poke Me Line” for inferior alveolar (mandibular) nerve block
Gow-Gates Mandibular Nerve Block
George A. E. Gow-Gates first published this technique in 1973 (Fig. 21.12) [7]. Significant advantages of the Gow-Gates mandibular NB over the IA NB include its higher success rate, its lower incidence of positive aspiration (2 %), and the absence of problems with accessory sensory innervation to the mandibular teeth. The Gow-Gates mandibular NB anesthetizes the inferior alveolar, lingual, auriculotemporal, buccal (75 % of the time), and mylohyoid nerves. The injection blocks the nerves at a point that is proximal to their division into inferior alveolar, buccal, and lingual nerves. The needle endpoint is the lateral aspect of the anterior portion of the condyle, just inferior to the insertion of the lateral pterygoid muscle. The injection is administered by having the patient open their mouth as widely as possible to rotate and translate the condyle forward. The condyle is palpated with the fingers of the nondominant hand while the cheek is retracted with the thumb. Beginning from the contralateral canine, the needle is positioned so that a puncture point is made approximately at the location of the distobuccal cusp of the maxillary second molar. A 25-gauge long needle is inserted slowly to a depth of 25–30 mm; the endpoint is inferior and lateral to the condylar head. The injection must not be performed unless bone is contacted to ensure proper needle placement. After the needle is withdrawn 1–2 mm, the clinician aspirates and injects the contents of the cartridge. This injection is unique among intraoral injections because the operator does not attempt to get as close as possible to the nerve to be anesthetized. In fact, the needle tip should be approximately 1.0 cm directly superior to the nerve, in the superior aspect of the pterygomandibular space.
Fig. 21.12
Gow-Gates mandibular nerve block ((a) area anesthetized; (b) technique
Vazirani–Akinosi Nerve Block
This form of injection, also known as the closed-mouth mandibular block , anesthetizes the inferior alveolar, lingual, buccal, and mylohyoid nerves (Fig. 21.13) [8, 9]. This injection is useful for patients with trismus because it is performed while the jaw is in its physiologic rest position. A 25-gauge long needle is inserted parallel to the maxillary occlusal plane at the height of the maxillary buccal vestibule. The bevel should be oriented away from the bone of the mandibular ramus so that deflection occurs toward the ramus. The depth of penetration is approximately half the mesiodistal length of the ramus, which is about 25 mm in adults (measured from the maxillary tuberosity). The depth of insertion will vary with the antero-posterior size of the patient’s ramus. The Vazirani–Akinosi injection is performed “blindly” because no bony endpoint exists. However, in adult patients, a rule of thumb is that the hub of the needle should be opposite the mesial aspect of the maxillary second molar. After aspiration, the contents of the cartridge (1.8 mL) can be deposited slowly.
Fig. 21.13
Vazirani–Akinosi (closed mouth) nerve block ((a) area anesthetized; (b) technique)
Incisive (Mental) Nerve Block
The mental and incisive nerves are terminal branches of the IA nerve. The mental nerve exits the mental foramen at or near the apices of the mandibular premolars. The incisive nerve continues anteriorly in the incisive canal. Both nerves will be anesthetized after a successful inferior alveolar nerve block, but this injection technique can be useful when bilateral anesthesia is desired for procedures on premolars and anterior teeth [28] (Fig. 21.14). The lingual tissues are not anesthetized with this block. The initial technique for the mental and incisive nerve blocks is the same. A 25- or 27-gauge short needle is inserted at the mucobuccal fold at or just anterior to the mental foramen, which is typically located between the apices of the two premolars. The bevel of the needle should be oriented toward the bone and the tissue penetrated to a depth of 5–6 mm. After aspiration, approximately one-third to one half of the cartridge (0.6–0.9 mL) should be deposited. The difference between the mental nerve block and the incisive nerve block is that the incisive nerve block requires pressure to direct local anesthetic solution into the mental foramen. This can be accomplished by maintaining gentle pressure at the injection site for approximately 2 min following deposition of the solution [28].