CHAPTER 51 LIVER INJURY
The liver is the most commonly injured intra-abdominal organ with an incidence of 30%–40%. The overwhelming majority of liver injuries, however, are minor, with spontaneous cessation of hemorrhage almost always the rule, and operative intervention is rarely required. On the other hand, complex hepatic injuries continue to challenge even the most experienced trauma surgeons.
INCIDENCE
Hepatic injury occurs in approximately 5% of all trauma admissions. Nationwide, there has been a steady decline in the incidence of penetrating liver injuries. However, blunt injuries seem to be on the rise predominantly because their presence has been more readily detected by the almost routine use of CT scanning in patients sustaining blunt trauma. The incidence of complex hepatic injuries, however, has remained relatively stable over the past 25 years, ranging from 12% to 15%.1
Motor vehicle crashes (MVCs) continue to account for most (approximately 80%) blunt hepatic injuries, followed by pedestrian and car collisions, falls, assaults, and motorcycle crashes. Most patients with blunt hepatic trauma have associated injuries, both intra-abdominal and extra-abdominal. Concomitant chest trauma is the most common associated injury encountered with blunt hepatic trauma, occurring in over 50% of patients. Patients with right-sided lower rib fractures, particularly ribs 9–11, have at least a 20% chance of sustaining an underlying hepatic injury. In spite of the high aforementioned incidence of associated chest trauma, injury to the brain remains the single most significant determinant in overall survival outcome.2 In the era of nonoperative management of blunt trauma, the risk of a missed injury, especially to the diaphragm or small bowel, is of major concern. Adherence to meticulous interpretation on imaging studies by experienced personnel should limit this pitfall to 1%–2%.
MECHANISM OF INJURY
Blunt Hepatic Injury
In MVCs, those most susceptible to hepatic injury are unrestrained front-seat passengers. These passengers are particularly vulnerable to a compression injury from the steering wheel especially during periods of rapid deceleration.3 Although the anterior abdominal wall stops, the posterior abdominal wall continues to move forward, and the intra-abdominal organs are “trapped” and compressed resulting in stretching/tearing of the liver at its vascular and structural attachments. As the liver is only partially protected by the rib cage, liver injury from steering wheel contact is one of the most important contributing factors to driver injury.
Penetrating Hepatic Injury
Damage caused by a penetrating injury is based on the kinetic energy of the projectile and the density and elasticity of the tissue. Lowenergy weapons such as knives only cut and do not create a temporary cavity. Medium-energy and high-energy firearms damage not only the tissue directly in the path of the missile but also the tissue on each side of the missile’s path. As a missile passes through the relatively inelastic liver parenchyma, a temporary cavity (three to six times the size of the missile’s front surface area, lasting for a fraction of a second) and a permanent cavity (visible to the examiner) are created. The higher-energy firearms create larger temporary and permanent cavities, resulting in far more extensive tissue damage; the vacuum created by this larger cavity pulls clothing, bacteria, and other debris from the surrounding area into the wound as well.
DIAGNOSIS
Hemodynamically Stable Patients
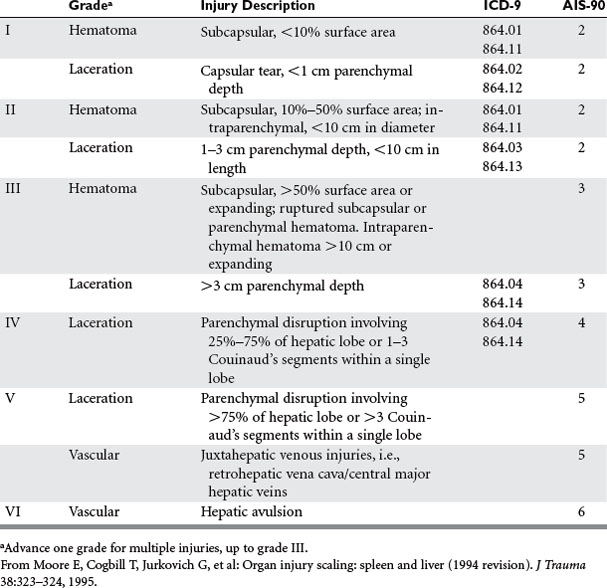
Scans should immediately be interpreted and classified according to the American Association for the Surgery of Trauma liver injury scale4 (Table 1) by the CT fellow or attending radiologist, always in the presence of the chief trauma resident and trauma attending. The senior trauma attending in presence makes the final decision as to the appropriateness of nonoperative therapy. It should be noted that the grade of injury or degree of hemoperitoneum on CT does not determine the need for operative intervention, as this decision is based primarily on the patient’s hemodynamic stability and the absence of peritoneal signs. Instead, the CT scan merely provides the surgeon with a general anatomic overview of the injury, identifies associated abdominal injuries requiring operative intervention, and can be used as a base for comparing future healing of the hepatic injury and resorption of intraperitoneal blood. CT can also identify injuries involving the bare area of the liver, which commonly present with minimal intra-abdominal bleeding, a paucity of abdominal signs, and often a negative DPL.
The role of FAST as a screening exam in hemodynamically stable patients is evolving and in the near future may eliminate the need for CT scan. Currently, many trauma centers forgo CT scanning in stable patients with negative initial FAST exams and merely repeat the FAST in 6 hours. However, scanning for only free fluid has its diagnostic limitations because not all blunt hepatic injuries result in hemoperitoneum. In a recent study looking specifically at sonographic detection of blunt hepatic trauma, Richards et al.5 determined the overall sensitivity of FAST for blunt hepatic injuries (all grades) to be 67%, based on the detection of free fluid alone. On the other hand, it is clear that most solid organ injuries without intraperitoneal fluid on FAST are, in general, of minimal clinical significance.6 At present, most trauma surgeons agree that those patients who are hemodynamically stable and who have either intraperitoneal blood on their initial FAST exam or positive findings on physical exam over the lower chest and upper abdomen should have a CT to specifically identify a hepatic or splenic injury that can be managed nonoperatively. Once identified, the hepatic injury may be followed with ultrasound if necessary.
ANATOMIC LOCATION OF INJURY AND INJURY GRADING—AAST-OIS
Comprehensive knowledge of hepatic anatomy is essential to the proper management of traumatic liver injuries. Couinaud has described the functional anatomy of the liver, based on the hepatic venous drainage (Figure 1). The ligamentous attachments of the liver are depicted in Figure 2.
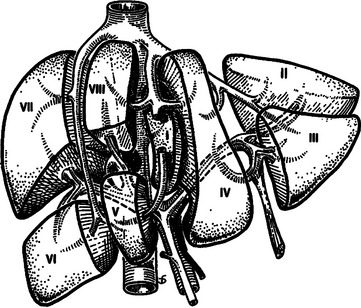
Figure 1 Functional division of the liver, according to Couinaud’s nomenclature.
(From Mattox KL, Feliciano DV, Moore EE, editors: Trauma, 4th ed. New York, McGraw-Hill, 1999, Figure 30-1. Originally appeared in Blumgart LH, editor: Surgery of the Liver and Biliary Tract. New York, Churchill Livingstone, 1988.)
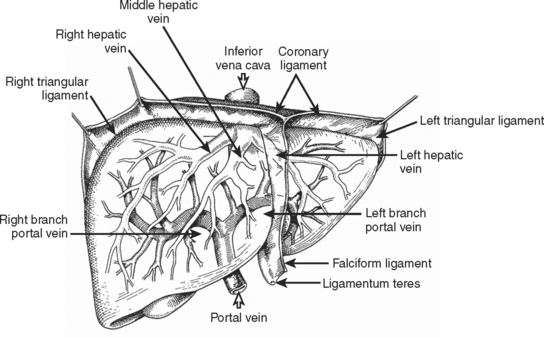
Figure 2 Surgical anatomy of the liver.
(From Mattox KL, Feliciano DV, Moore EE, editors: Trauma, 5th ed. New York, McGraw-Hill, 2004, Figure 30-2.)
The American Association for the Surgery of Trauma (AAST) created the Organ Injury Scaling (OIS) Committee to standardize injury severity scores for individual organs to facilitate clinical investigation and outcomes research. The liver injury scale devised by the AAST is shown in Table 1.
MANAGEMENT
Nonoperative Management/Blunt Hepatic Trauma
 Absence of associated intra-abdominal or retroperitoneal injuries on CT scan that require operative intervention
Absence of associated intra-abdominal or retroperitoneal injuries on CT scan that require operative interventionPreviously cited inclusion criteria such as neurological integrity are no longer valid, as neurologically impaired patients can be safely managed nonoperatively in a monitored setting.7 Furthermore, mandatory repeat CT scans to document improvement or stabilization of injury are unnecessary and contribute little to patient outcome. Rather, the patient’s clinical course should dictate the need for additional evaluation.
Most (80%–90%) blunt hepatic trauma patients can be successfully managed nonoperatively. Although nonoperative management was initially limited to AAST grades I–III injuries, it is now clear that the hemodynamic status of the patient, rather than AAST grade of injury, is the most significant factor in determining the need for operative intervention. Up to 20% of select patients with grades IV and V injuries can be managed nonoperatively. However, many grade IV and most grade V injuries will usually present with hemodynamic instability or concomitant injuries mandating surgery, thus precluding nonoperative intervention. In a multi-institutional study, grades IV and V injuries were responsible for 67% of all patients who failed nonoperative management and subsequently required operative intervention.8 Therefore, although hemodynamic stability determines which patients can be managed nonoperatively, the subgroup of patients with complex hepatic injuries (grades IV and V) are at substantially higher risk for treatment failure and should therefore be closely monitored in a critical care unit.
Conversely, the same basic standards apply to patients with lower AAST-grade injuries (i.e., I–III). In these instances, the initial injury may be deemed as “not significant,” and thus it becomes tempting to avoid surgical intervention despite hemodynamic instability or a decreasing hematocrit, relying instead on further fluid and blood transfusions. This course of action is fraught with pitfalls and should be avoided to minimize the morbidity and mortality of nonoperative management. To summarize, of all the variables monitored, hemodynamic stability appears to be the most crucial and is considered the watershed for nonoperative or operative intervention.
Nonoperative Management/Penetrating Hepatic Trauma
Renz et al.9 nonoperatively managed 13 patients with penetrating right thoracoabdominal gunshot wounds. The authors stressed the importance of serial abdominal exams and contrast-enhanced CT scanning in their successful nonoperative management. Demetriades et al.10 substantiated this concept with their successful management of select patients with isolated gunshot injuries to the liver. These authors concluded that hemodynamically stable patients with grades I and II liver injuries and no evidence of peritonitis can be safely managed nonoperatively. However, it should be noted that this approach failed in nearly one-third (5/16) of the patients in the “observed group” who eventually required delayed laparotomy. More recently, Omoshoro-Jones et al.11 described successful nonoperative management in 31 of 33 patients with gunshot wounds to the liver, including grades III–V injuries. Although the higher-grade injuries were associated with more complications (most of which were managed nonoperatively), the overall success of nonoperative management did not depend on the AAST grade of liver injury.
Operative Management/General Principles
Before the incision is made, the patient should receive a dose of antibiotics to cover aerobic and anaerobic microbes and is placed on a warming blanket. The surgeon must keep in mind that hypothermia is a frequent complication of resuscitation and operation in patients with major hepatic injuries. Appropriate maneuvers to decrease hypothermia are shown in Table 2.12 Adherence to these maneuvers will usually prevent the development of intraoperative coagulopathies and fatal arrhythmias.
Table 2 Maneuvers to Prevent/Decrease Hypothermia in Patients with Major Hepatic Injuries
< div class='tao-gold-member'> Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|