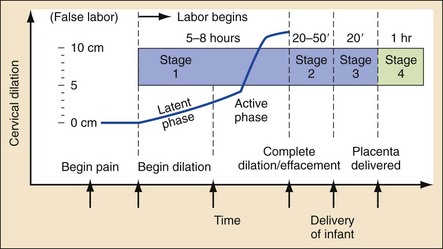
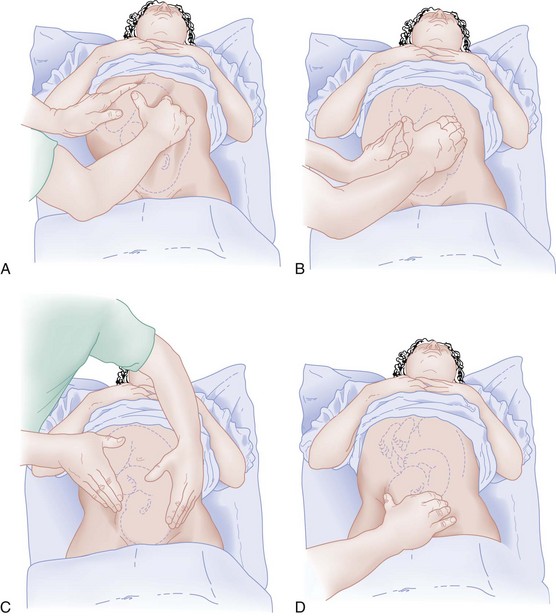
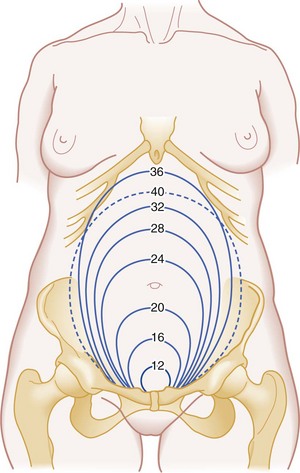
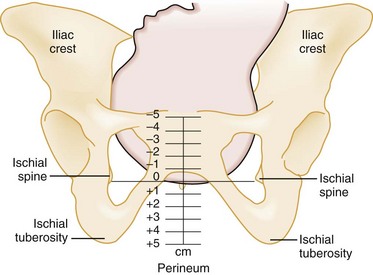
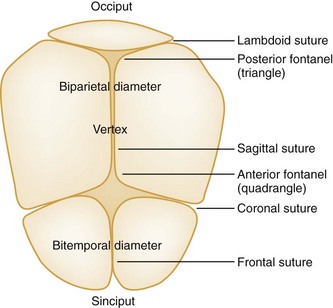
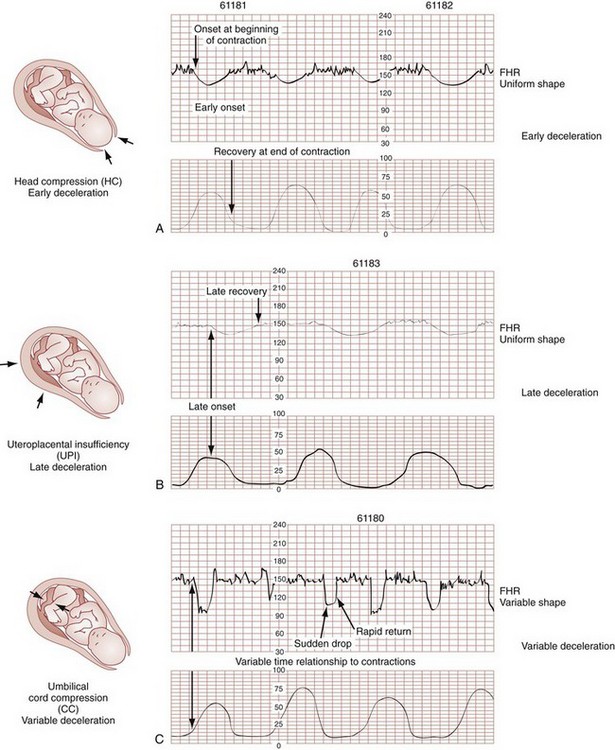
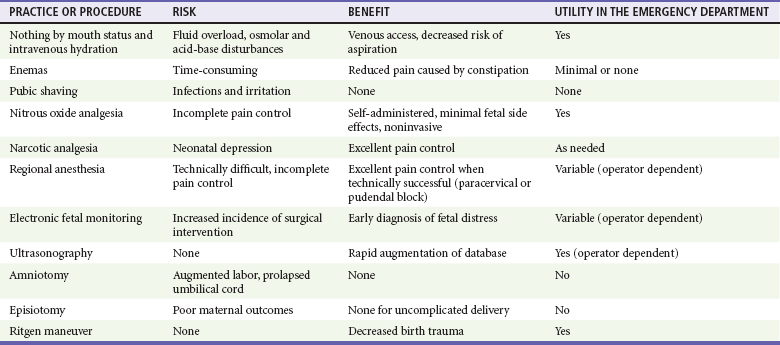
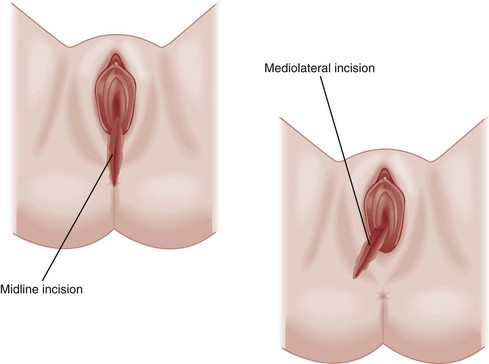
Chapter 181 Emergency department (ED) births are rare. In most cases, patients in labor are triaged directly to the obstetric suite for urgent management, maintaining a continuum of care with their primary providers. Because some births are precipitous and obstetric resources may not be immediately available, the emergency physician must possess the basic skills for intrapartum management of both normal and abnormal deliveries. In addition, a general knowledge of postpartum care is required in case of the occasional out-of-hospital delivery.1,2 In 2004 the perinatal mortality rate in the United States was 6.2 per 1000 live births and fetal deaths (<20 weeks of gestation).3 Delivery complications and mortalities do occur with greater frequency in the ED, where the perinatal mortality rate is approximately 8 to 10%.4 There are multiple causes of the “high-risk” ED delivery profile. The ED is often selected by an obstetric population with unexpected complications. Antepartum hemorrhage, premature rupture of membranes (PROM), eclampsia, premature labor, abruptio placentae, precipitous delivery, malpresentation, and umbilical cord emergencies are overrepresented in the ED population.4 Psychosocial factors further skew the epidemiology of ED deliveries. Women who present with precipitous deliveries often have had little or no prenatal care.5 Pregnant women who have drug or alcohol problems or are victims of domestic violence represent a disproportionate number of patients who deliver in the ED. Women who are unaware or in denial of their pregnancies or immigrants without access to other medical care also present to the ED when labor begins.6–8 Because of the high risk associated with ED delivery, patients should be transported to a facility that has obstetric and neonatal resources whenever possible. The management of a premature infant may require highly specialized intensive care that is unavailable at many community hospitals. The desire to transfer a woman with an impending high-risk delivery to such a facility should be tempered, however, by clinical and medicolegal judgment.9,10 Transfer, with resultant en route delivery, can be disastrous for the mother and fetus. Such a transfer also violates federal law. The Consolidated Omnibus Reconciliation Budget Act (COBRA) of 1989 was based on an “inappropriate” obstetric transfer.11 Federal law has identified labor as a condition unsuitable for transfer because of its unstable nature. Although the intent of this legislation is to protect women from medical abandonment because of financial reasons, COBRA runs the risk of forcing emergency physicians to occasionally perform difficult high-risk deliveries that might have better outcomes with transfer.12 For many ED deliveries, labor will have progressed to a point at which tocolysis is contraindicated and delivery is imminent. In general, this is when the mother feels the urge to push or the head is crowning. Whenever possible, a neonatologist or pediatrician should attend high-risk preterm (<36 weeks of gestation) deliveries, and preparations for neonatal resuscitation and high-level nursery care should be initiated (Box 181-1). The first stage of labor is the cervical stage, ending with a completely dilated, fully effaced cervix. It is divided into a latent phase, with slow cervical dilation, and an active phase, with more rapid dilation. The active phase begins once the cervix is dilated 3 cm.13 In multiparous women, the active phase can progress rapidly into stage 2 of labor (delivery of the fetus). Most women who deliver in the ED arrive while in the active phase of stage 1 or early stage 2 labor (Fig. 181-1).4 The duration of the first stage of labor averages 8 hours in nulliparous women and 5 hours in multiparous women. During this time, frequent assessment of fetal well-being is important. For low-risk pregnancies, fetal heart tones should be auscultated approximately every 15 minutes. For higher risk pregnancies, continuous external electrical monitoring may help identify fetal distress, allowing appropriate intervention.14 Abdominal examination with Leopold’s maneuvers may confirm the lie of the fetus (Fig. 181-2). After labor has begun, particularly during the active phase of stage 1, Leopold’s maneuvers are difficult to use. The firm contractions of the uterus prevent the identification of fetal “small parts.” Other modalities of assessing the lie, such as ultrasonography, may be necessary if presentation remains in question.15 Maternal examination also provides a rough guide to gestational age. At 20 weeks’ gestation, the uterine fundus reaches the umbilicus. Approximately 1 cm of fundal height is added per week of gestation until 36 weeks. At that time, the fundal height decreases as the fetus “drops” into the pelvis (Fig. 181-3). These estimates help establish gestational age rapidly. Effacement refers to the thickness of the cervix. A paper-thin cervix is 100% effaced. Dilation indicates the diameter of the cervical opening in centimeters. Complete, or maximum, dilation is 10 cm. Position describes the relationship of the fetal presenting part to the birth canal. The most common position of the head is occiput anterior. Station indicates the relationship of the presenting fetal part to the maternal ischial spines (Fig. 181-4). Presentation specifies the anatomic part of the fetus leading through the birth canal. In 95% of all labors, the presenting part is the occiput, or vertex. On digital examination, a smooth surface with 360 degrees of firm bony contours and palpable suture lines is noted. Palpation of the suture lines and the fontanels where they join allows the examiner to determine the direction the fetus is facing. Three sutures radiate from the posterior fontanel, and four radiate from the anterior fontanel (Fig. 181-5). The lateral margins are examined carefully for fingers or facial parts that indicate compound or brow presentations. When the clinician suspects rupture of membranes, a sterile speculum examination is performed. This may reveal pooling of amniotic fluid. Two tests to confirm the presence of amniotic fluid include a fernlike pattern when the fluid is allowed to dry on a microscope slide and the use of Nitrazine paper, which should turn blue, indicating an alkaline amniotic fluid (pH > 6). Although vaginal blood, cervical mucus, semen, and infection can interfere with results, sensitivities of both Nitrazine paper and ferning in detection of amniotic fluid are nearly 90%.16 The second stage of labor is characterized by a fully dilated cervix and accompanied by the urge to bear down and push with each uterine contraction. The fetal station is advanced to +3, with crowning of the presenting part as expulsion begins. Stage 2 uterine contractions may last 1 or 2 minutes and recur after a resting phase of less than 1 minute. The median duration of this stage is 50 minutes in nulliparous women and 20 minutes in multiparous women. More rapid progression through stage 2 should be anticipated for low-birth-weight premature infants. A prolonged second stage of labor is defined as more than 3 hours in nulliparous women if regional anesthesia is administered, more than 2 hours in nulliparous women without anesthesia or in multiparous women with regional anesthesia, and more than 1 hour in multiparous women without regional anesthesia.17 Prolonged second stage of labor is associated with an increase in maternal complications, including postpartum hemorrhage, infection, and severe vaginal lacerations.18 Antenatal Fetal Assessment: The assessment of a woman in the third trimester includes an assessment of fetal well-being. After 24 weeks’ gestation, the fetal condition affects clinical decision-making. During labor and delivery, the identification of fetal distress and appropriate intervention can reduce fetal morbidity and mortality. Electronic Fetal Monitoring.: Intrapartum fetal assessment by electronic fetal monitoring is most useful during stage 1 of labor. Electronic fetal monitoring confirms true labor and may help diagnose fetal distress. Tracings of fetal heart rate and uterine activity provide information that in combination with clinical data can presage fetal distress due to hypoxia and provide a window for intervention. Fetal heart rate tracings have several components that can be assessed: baseline heart rate, variability, accelerations, decelerations, and diagnostic patterns. Baseline heart rate, by definition, is the average fetal heart rate during a 10-minute period (in the absence of a uterine contraction) and is the most important aspect of fetal heart rate monitoring. Fetal bradycardia is defined as a baseline rate of less than 110 beats per minute; fetal tachycardia is defined as a baseline rate of more than 160 beats per minute.19 Decelerations in fetal heart rate are more complicated, and their interpretation should be integrated with the clinical situation. There are three types of deceleration: variable, early, and late (Fig. 181-6). These terms refer to the timing of the deceleration relative to the uterine contraction. Late decelerations are more serious and most often indicate uteroplacental insufficiency. The tracing contours are generally smooth, with the heart rate nadir occurring well after maximal uterine contraction (typically 30 seconds or more afterward).19 The lag, slope, and magnitude of late decelerations correlate with increasing fetal hypoxia. Late decelerations are particularly ominous in association with poor variability, nonreactivity, and baseline bradycardia. When these findings are present, immediate obstetric consultation for delivery to prevent further hypoxia is indicated. The need for newborn resuscitation should be anticipated and preparation for critical care established for these deliveries. Overall, 30% of infants with late decelerations have good outcomes. The remaining 70% have suboptimal outcomes related to either the underlying pathologic condition or hypoxia. Ultrasonography.: Ultrasonographic techniques have wide application in obstetric care. In the third trimester or during labor, ultrasonography can provide crucial information pertaining to impending delivery. When a technician and radiologist are available, the gestational age, biophysical profile, and amniotic fluid index as well as a survey of fetal and placental anatomy may be discerned (Table 181-1). The parameters of immediate interest in the ED are fetal viability (specifically in utero gestation and fetal heart rate), lie, and presentation. Ultrasonography may also reveal multiple gestations, allowing preparation and early communication with other specialists (from obstetrics, neonatology, and anesthesia). In 1991 the American College of Obstetricians and Gynecologists (ACOG) published recommendations regarding the indications for ultrasonography in the third trimester (Box 181-2). A 2- to 5-MHz transducer is appropriate for all bedside transabdominal sonographic assessments. Transvaginal ultrasonography is relatively contraindicated in the peripartum period, particularly in the cases of PROM and placenta previa.20 Table 181-1 Biophysical Profile: 30 Minutes of Ultrasonographic Observation Delivery: As stage 2 of labor progresses, preparation for delivery should be under way. A radiant warmer should be available and heated. Neonatal resuscitation adjuncts, such as a towel, scissors, umbilical clamps, bulb suction, airway management equipment (oxygen, bag-mask device with appropriate-sized masks, and endotracheal intubation and suctioning equipment for meconium), and equipment to achieve vascular access, should be available. Most deliveries require only basic equipment to cut and clamp the umbilical cord, to suction the mouth and nose, and to dry and stimulate the infant. A nurse should be at the bedside to coach and to provide reassurance to the mother. Controlled, coordinated expulsion with coaching to sustain each push aids with crowning and delivery of the head. When the fetus is crowning, care is exercised to have the delivery occur in a slow, controlled manner. Precipitous delivery is more likely to cause maternal injuries, such as perineal, rectal, urethral, labial, vaginal, and uterine lacerations, and fetal injuries.21 One described technique to potentially decrease the rate of maternal injury is the modified Ritgen maneuver.22 In the modified Ritgen maneuver, a towel-draped, gloved hand is used to stretch the perineum and gently exert pressure on the chin of the fetus. The second hand puts pressure on the occiput superiorly, guiding the head into slight extension. When the head is at the perineum, this slight extension of the head promotes delivery by positioning the head so that its smallest diameter passes through the pelvic outlet and perineum. Episiotomy.: Previously, the need for episiotomy in normal deliveries was an area of controversy. The original potential benefit of episiotomy included the substitution of a straight surgical incision for a ragged, uncontrolled traumatic laceration. Theoretically, the surgical approach decreased the incidence of severe rectovaginal tears. This rationale led to widespread routine episiotomy, with a medial incision used in the United States and a mediolateral incision used in the Commonwealth countries. Recent literature has shown that both types of incisions increase maternal morbidity, and they are no longer recommended for uncomplicated deliveries. Women receiving episiotomies have been shown to have a higher incidence of perineal trauma and maternal blood loss during delivery and more pelvic pain, sexual dysfunction, and urinary incontinence in the postpartum period.23 Episiotomy should be performed only for specific indications, such as shoulder dystocia or breech delivery. When the decision is made to use an episiotomy, the procedure should be done before excessive stretching of the perineal muscles occurs but near the time of delivery to avoid excessive bleeding. Common practice is to cut the episiotomy when the head is visible during a contraction and the introitus opens to a diameter of 3 or 4 cm. Most authors currently recommend a mediolateral incision to avoid perineal tears and rectal involvement; this is particularly true for a complicated delivery in which lacerations extending the surgical incision are likely (Fig. 181-7). Figure 181-7 A mediolateral episiotomy incision is preferred to a strictly midline incision. (Redrawn from www.aurorahealthcare.org/healthgate/images/exh44028a_ma.jpg.) Table 181-2 summarizes some of the adjuncts used in normal labor and delivery, with recommendations for their use in the high-risk setting of an ED delivery. These signs usually occur within 5 to 10 minutes of the delivery of the infant but may extend to 30 minutes. The risk of postpartum hemorrhage increases beyond 18 minutes and is in fact up to six times more likely after 30 minutes.25 Although the placenta may be delivered expectantly, active management reduces the length of the third stage of labor and thereby decreases the risk of postpartum hemorrhage. Active management includes the administration of uterotonics, gentle traction of the clamped umbilical cord with mild pressure applied above the symphysis pubis, and uterine massage after delivery.26 Be aware that any attempt to deliver the placenta before it separates is contraindicated. Normally a three-vessel structure, the umbilical cord is filled with a connective tissue known as Wharton’s jelly and is approximately 50 to 60 cm long and 12 mm in diameter. Normal architecture places the two umbilical arteries on either side of the single umbilical vein. A two-vessel cord (one umbilical artery) occurs in 1 of 500 deliveries, is more common in African Americans, and is a result of aplasia or atrophy. Approximately 30% of two-vessel cord infants have congenital defects. An association also exists between fetal structural anomalies and placental vascular occlusion or thrombosis.27 The placenta should also be examined for abnormalities. Clots adherent to the uterine aspect may indicate placental abruption. Accessory lobes (succenturiate placenta if completely separate) and abnormal cord insertion are common abnormalities. The umbilical cord and placenta routinely should be held for pathologic review.28 The discovery of an incomplete placenta or membranes should alert the emergency physician to the possibility of postpartum complications and should be documented. Third-Trimester Complications Associated with Delivery Perspective.: Premature or preterm labor and fetal immaturity are the leading causes of neonatal mortality. Preterm labor is defined as uterine contractions with cervical changes before 37 weeks of gestation. Women with premature labor are a heterogeneous group. Many underlying conditions result in preterm labor, which accounts for 9.6% of all pregnancies but 70% of all perinatal mortality.29 Factors linked to this problem include substance abuse, history of preterm delivery, multiple gestations, placental anomalies, infections, and lifestyle or psychosocial stressors30 (Box 181-3). The unexpected nature of premature labor often results in an ED visit. When delivery is not imminent, the patient can be moved to the obstetrics unit for further care. Clinical Features.: The diagnosis of preterm labor requires the identification of uterine activity and cervical changes before 37 weeks of gestation. Early maternal signs and symptoms include an increase or change in vaginal discharge, pain resulting from uterine contractions (sometimes perceived as low back pain), pelvic pressure, vaginal bleeding (usually bloody show), and fluid leak. Diagnostic Strategies.: If uterine contractions and cervical changes are present and the estimated fetal weight on ultrasonography is less than 2500 g, the diagnosis of premature labor is likely. The differentiation of false labor (Braxton Hicks contractions) from true labor is best done by electrical monitoring. Ultrasonography may aid in the diagnosis because fetal breathing movements make the diagnosis of false labor unlikely. The initial evaluation of a woman with possible preterm labor includes urinalysis, complete blood count, and pelvic ultrasonography. If delivery is not imminent, these studies can be performed in the ED or obstetrics area, whichever would provide the best monitoring. When possible, these patients should be transferred to a perinatal center with an associated intensive care unit. Management.: A viable fetus and healthy mother are indications for medical management directed toward the prolongation of gestation. Preterm labor should not be postponed with medical management in the cases of fetal compromise, major congenital anomalies, intrauterine infection, placental abruption, eclampsia, significant cervical dilation, or, most important, PROM.31 The treatment of preterm labor involves multiple modalities. Tocolytics and fetal maturation therapy combined with bed rest and hydration are used in the hope of prolonging pregnancy (Box 181-4). These patients optimally should be transferred to an appropriate center before delivery whenever possible because medical management fails in more than 25% of preterm patients in whom it is attempted.32 Tocolysis: The two classically used tocolytics are magnesium sulfate and beta-mimetic drugs. Other medications that have been shown to be effective include prostaglandin synthetase inhibitors (nonsteroidal anti-inflammatory drugs [NSAIDs]) and calcium channel blockers.33 When they are indicated and in coordination with an obstetric consultant, tocolytics initiated in the ED may arrest premature labor, preventing imminent delivery in 75 to 80% of patients for 48 to 72 hours.29 Magnesium Sulfate: Magnesium sulfate competitively inhibits calcium uptake into smooth muscle and allows relaxation. The efficacy of magnesium sulfate as a tocolytic agent has not been clearly established.34 Women treated with magnesium require monitoring. Magnesium produces respiratory and neurologic depression at elevated levels, exacerbated by renal insufficiency. Pulmonary edema and cardiac dysrhythmias have also been reported.29 These effects can be reversed rapidly by the administration of calcium-containing solutions (i.e., 1 g of 10% calcium gluconate solution) (Table 181-3). Table 181-3 Beta-Mimetics: Beta-mimetics (ritodrine and terbutaline) cause smooth muscle relaxation by activating enzymes that bind calcium to the sarcoplasmic reticulum. This effect is mediated by beta2 receptors that increase cyclic adenosine monophosphate concentrations in the myometrium. The beta-mimetic is titrated to effect because the dosage needed to eliminate uterine activity varies. In one meta-analysis, beta-mimetics and magnesium sulfate had similar efficacy in elimination of contractions.33 Despite evidence that beta-mimetics are effective tocolytics, their side effect profile is somewhat prohibitive for their selection over other options. Maternal pulmonary edema, myocardial ischemia, and cardiac dysrhythmia are the main adverse effects of high-dose beta-mimetics. Pulmonary edema is more likely to occur in mothers with preexisting cardiac disease, multiple gestation, and maternal infection. Pulmonary edema is caused by high-output failure and tends to occur when there is sustained maternal tachycardia of more than 120 beats/minute. Beta-mimetics should be gradually titrated according to uterine activity and maternal heart rate.30 Other beta-mimetic side effects include gluconeogenesis and glycogenolysis, which can be a problem for diabetic mothers. Surveillance of the urine for glucose and ketones is recommended. Fetal heart stimulation can result in both fetal dysrhythmia and cardiac hypertrophy. Also, some studies have shown an association between beta-mimetics and an increased incidence of fetal intraventricular hemorrhage.35 NSAIDs: The prostaglandin synthetase inhibitors, specifically indomethacin and sulindac, have been shown to be as effective as magnesium and the beta-mimetics in multiple trials. However, in the fetus, pulmonary hypertension, ductus arteriosus constriction, renal insufficiency, necrotizing enterocolitis, and intraventricular hemorrhage have been reported with NSAID use. Potential maternal side effects include a prolonged bleeding time and renal insufficiency.33,36 Calcium Channel Blockers: Calcium channel blockers have also been used as tocolytics with success, reducing muscle contractility by their effect on transmembrane calcium influx. Nifedipine or nicardipine may be given.37 Equal in efficacy to ritodrine and magnesium sulfate, calcium channel blockers have been shown to have relatively good maternal and fetal side effect profiles.30 Aggressive titratable tocolytics are best for the initial 24 to 48 hours of preterm labor. After uterine contractions have been stopped, the patient can usually be maintained with oral agents, although the benefits of maintenance tocolysis, studied to date primarily with beta-mimetics and magnesium, have yet to be shown.33 It is important to review the contraindications to tocolytics before initiation of these therapies (Box 181-5). Any patient receiving tocolytics should be externally monitored (electrically) for signs of fetal distress.
Labor and Delivery and Their Complications
Perspective
Epidemiology of Emergency Delivery
Patient Transfer Considerations
Medicolegal Considerations
Nursery Requirements
Normal Delivery
Stages of Labor
Second Stage of Labor
ELEMENT ASSESSED
NORMAL SCORE = 2
ABNORMAL SCORE = 0
Fetal heart rate reactivity
2 accelerations >15 beats/minute for >15 seconds
<2 accelerations
Amniotic fluid index
1 pocket >1 cm in orthogonal planes
No large pockets
Fetal muscle tone
1 episode of active flexion-extension with full return to flexed posture
<1 episode or slow, incomplete actions
Body movements
3 discrete moves
≤2
Breathing motions
1 episode of fetal breathing of at least 60 seconds in duration during 30 minutes of observation
No breathing activity
or
The absence of 1 episode of fetal breathing of at least 60 seconds in duration during 30 minutes of observation
Third Stage of Labor
Specific Disorders
Premature Labor
DRUG
EFFECT ON LABOR
Barbiturates
Can stop labor in anesthetic doses
Alcohol
Decreases oxytocin release, smooth muscle relaxant
Cocaine
Increased prematurity, placental infarction
Caffeine or aminophylline
Increased duration of labor
Narcotics
Increased latent phase, slow dilation (minimal effect once in active labor)
Atropine, scopolamine
Lower uterine segment relaxation, decreased frequency of contractions
Halothane
Strong inhibition of labor
IV nitroglycerin
Profound uterine relaxation