146 Insecticides, Herbicides, and Rodenticides
• Organophosphorus and carbamate poisonings cause excessive stimulation of muscarinic and nicotinic receptors by acetylcholine, which can potentially lead to life-threatening bronchorrhea and bronchospasm.
• Aggressive airway management and liberal use of atropine are important in the management of both organophosphorus and carbamate poisoning.
• Only a nondepolarizing neuromuscular blocker, such as vecuronium or rocuronium, should be used for intubation. Succinylcholine is metabolized by plasma cholinesterase, and prolonged paralysis may result if it is used in the setting of organophosphate poisoning.
• Timely administration of pralidoxime is key to the treatment of organophosphorus poisoning, but pralidoxime is not indicated for carbamate poisoning.
• Unintentional pediatric ingestion of 4-hydroxycoumarins (superwarfarins) accounts for the vast majority of rodenticide exposures and rarely results in toxicity.
• Ingestion of an anticoagulant rodenticide should be considered when a child younger than 6 years has an elevated prothrombin time or bleeding without another explanation.
• The prothrombin time should be measured at 24 and 48 hours after large ingestions of 4-hydroxycoumarins.
• Because no specific antidote or pharmacologic intervention has proved beneficial in treating paraquat or diquat poisoning, early decontamination is the most important step.
insecticides
Organophosphorus Compounds and Carbamates
Epidemiology
Organophosphate (OP) compounds and carbamates are used extensively worldwide for agricultural, industrial, and domestic pest control and, as a result, represent a significant public health issue in the developing world. An estimated 3 million poisonings and more than 200,000 deaths occur from OP compounds each year worldwide.1 In the United States in 2008, 4642 exposures to OP compounds and 2644 exposures to carbamates were reported to the National Poison Data System of the American Association of Poison Control Centers.2
Pathophysiology
Under normal circumstances, ACh is hydrolyzed by AChE to yield acetic acid and choline. In the presence of OP insecticides, AChE is phosphorylated, whereas in the presence of carbamate insecticides, the enzyme is carbamylated. As a result, the rate of regeneration of active AChE is slowed, and its function is inhibited. Within 24 to 72 hours of OP poisoning, an alkyl group may dissociate from the AChE-OP complex and thereby result in “aging” of the AChE. Once aging occurs, reactivation of AChE is no longer possible, and only synthesis of new enzyme can restore activity. In the case of carbamate poisoning, breakdown of the carbamate-AChE complex occurs much more rapidly and aging does not occur (Box 146.1).3
Box 146.1 Effects of Organophosphate and Carbamate on Acetylcholinesterase (AChE)
These complexes inactivate AChE and allow acetylcholine to sit on the nicotinic and muscarinic receptors and produce the symptoms of toxicity.
Three things can happen to the phosphorylated or carbamylated AChE:
ACh accumulates in the autonomic nervous system at postganglionic muscarinic (parasympathetic and sympathetic) receptors and preganglionic nicotinic (sympathetic) receptors. It also accumulates at the neuromuscular junction and in the central nervous system (CNS). Overstimulation of these receptors is responsible for the cholinergic toxidrome seen with OP and carbamate insecticide poisoning (Table 146.1).
See Table 146.1, Effects of Organophosphorus and Carbamate Insecticides, at www.expertconsult.com
Table 146.1 Effects of Organophosphorus and Carbamate Insecticides
| RECEPTOR | TARGET TISSUE | CLINICAL EFFECT |
|---|---|---|
| Gastrointestinal tract | Vomiting, diarrhea, cramping | |
| Genitourinary tract | Urination | |
| Heart | Bradycardia | |
| Lungs | Bronchorrhea, bronchospasm | |
| Eye | Miosis, lacrimation | |
| Salivary glands | Salivation | |
| Sweat glands | Diaphoresis | |
| Adrenal glands | ↑ Catecholamines—tachycardia | |
| Central nervous system (nicotinic/muscarinic) | Brain | Agitation, seizures, coma (organophosphates > carbamates) |
| Neuromuscular junction (nicotinic) | Skeletal muscle | Weakness, fasciculations, paralysis |
Presenting Signs and Symptoms
The clinical effects are summarized in Table 146.1; only caveats in the clinical findings are emphasized here. Bronchorrhea occurs commonly with moderate to severe poisonings4 and can progress to pulmonary edema and respiratory failure. Miosis in the setting of cholinergic symptoms is fairly specific for OP and carbamate insecticide poisoning and may help make the diagnosis. Unfortunately, it is not consistently present.
Although the parasympathetic muscarinic effects are most often emphasized, certain sympathetic effects may predominate. Sinus tachycardia is more common than bradycardia,4,5 and mydriasis may even be seen.5 Nicotinic effects often predominate in mild cases and occur early in severe cases. Excessive nicotinic stimulation at the neuromuscular junction has effects that resemble the actions of a depolarizing neuromuscular blocking agent. Therefore, patients with OP or carbamate insecticide poisoning may exhibit muscle fasciculations and weakness. Paralysis occurs as the toxicity worsens, and the primary cause of death in acute poisonings is probably respiratory arrest secondary to paralysis and bronchorrhea.
One to 3 days after apparent resolution of the symptoms, patients may experience profound weakness and paralysis of the proximal muscles, neck flexor muscles, and cranial nerves. This development, termed the intermediate syndrome,6 is probably explained by ongoing AChE inhibition (Box 146.2).
Box 146.2 Paralysis Seen After Organophosphate Poisoning
Type II (Intermediate Syndrome)
• Develops 1 to 3 days after resolution of the acute organophosphate poisoning symptoms
• Manifested as paralysis and respiratory distress secondary to weakness of the proximal muscles, neck flexor muscles (with relative sparing of the distal muscle groups), and cranial nerve palsies
• Lasts for 4 to 18 days and may require mechanical ventilation
• Results from ongoing acetylcholinesterase inhibition or suboptimal treatment
Differential Diagnosis and Medical Decision Making
A detailed history in a patient with signs and symptoms of cholinergic excess often elucidates exposure to OP or carbamate insecticides. The diagnosis of OP or carbamate insecticide poisoning is therefore usually straightforward; however, certain clinical aspects may be mimicked by other entities. Table 146.2 is a partial list of other agents or diagnoses to consider.
Table 146.2 Differential Diagnosis of Organophosphorus and Carbamate Poisoning
| Other acetylcholinesterase inhibitors | Physostigmine, neostigmine, pyridostigmine |
| Other organophosphorus cholinesterase inhibitors (chemical weapon nerve agents) | Sarin, tabun, soman, Vx |
| Cholinomimetics | Pilocarpine, carbachol, methacholine, bethanechol, muscarine-containing mushrooms |
| Nicotinic alkaloids | Nicotine, coniine, lobeline |
| Other (symptom based) |
All patients with potential OP poisoning should undergo erythrocyte (red blood cell [RBC], or true) cholinesterase and plasma (pseudo) cholinesterase measurement from specimens obtained after arrival at the emergency department (ED). Though not often useful or necessary for making a diagnosis in the ED, the results of this measurement may help guide continued therapy. RBC cholinesterase hydrolyzes ACh and correlates with toxicity, whereas plasma cholinesterase is the first to decline and may be a more sensitive marker of exposure.7 Both substances should be measured because one may exhibit greater inhibition than the other, depending on the specific OP to which the patient was exposed. Box 146.3 summarizes the tests that may be helpful in evaluating a patient with moderate to severe toxicity.
Treatment
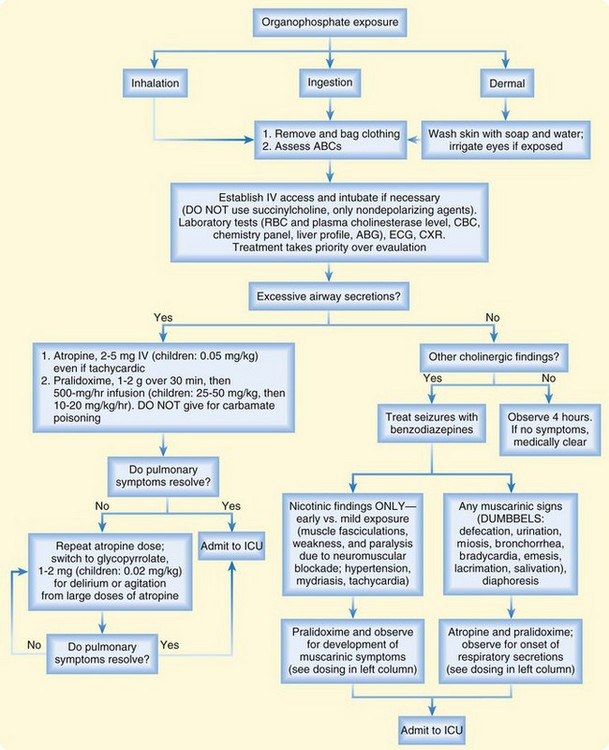
The treatment algorithm for OP and carbamate insecticide poisoning is summarized in Figure 146.1. The first step is adequate decontamination of the patient by removal of wet clothing and washing of contaminated skin with soap and water. ED personnel should wear gowns, gloves, and masks to prevent exposure to contaminated body fluids.8
As the patient is being decontaminated, the emergency physician (EP) should focus on the ABCs (airway, breathing circulation), with particular attention paid to early airway, management for copious secretions, seizures, coma, severe weakness, and paralysis. If intubation is necessary, only a nondepolarizing neuromuscular blocking agent, such as vecuronium or rocuronium, should be used. Succinylcholine is metabolized by plasma cholinesterase, so prolonged paralysis may result if this agent is used a patient with OP poisoning.9
![]() Priority Actions
Priority Actions
Organophosphates
Treatment should next be directed at controlling muscarinic activity. Atropine is the drug of choice and should be administered intravenously at a dose of 2 to 5 mg (pediatric dose, 0.05 mg/kg) every 3 to 5 minutes, with the end point being control of respiratory secretions. Tachycardia is not a contraindication to atropine administration. Mild poisonings may resolve with just 1 to 2 mg of atropine, and severe poisonings may require more than 1000 mg.10 Large doses of atropine may lead to antimuscarinic CNS toxicity. If such toxicity occurs, glycopyrrolate (1 to 2 mg; pediatric dose, 0.025 mg/kg) can be used in place of atropine.
Organochlorines
Epidemiology
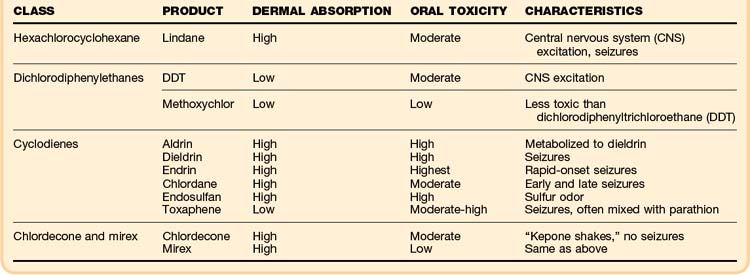
Organochlorines are heavily chlorinated aromatic compounds that are nonvolatile and poorly water soluble. They are divided into four classes on the basis of their structural characteristics, and they vary tremendously with respect to dermal absorption, lipid solubility, and toxic doses. The clinical toxicity, which is similar for each of the classes, is summarized in (Table 146.3).
See Table 146.3, Major Organophosphorus Insecticides, at www.expertconsult.com
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree