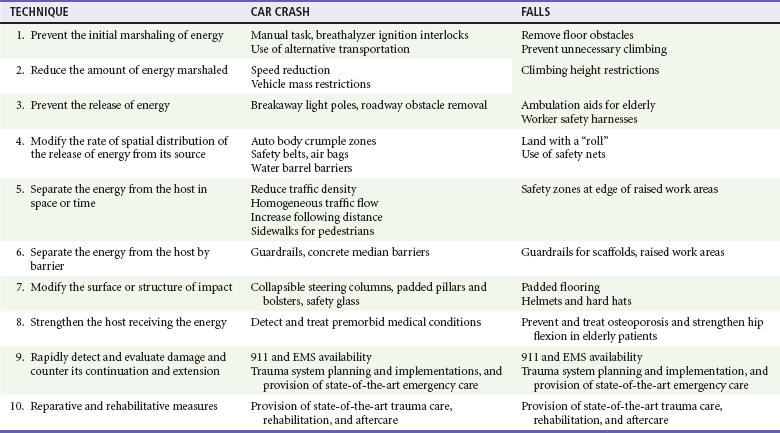
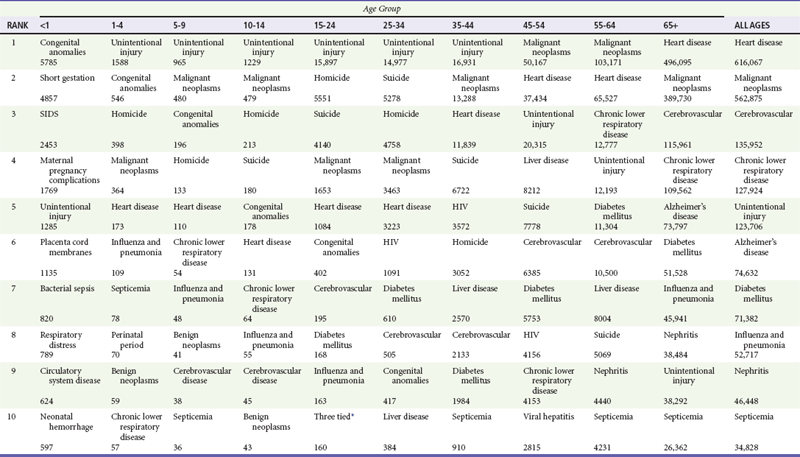
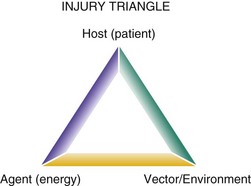
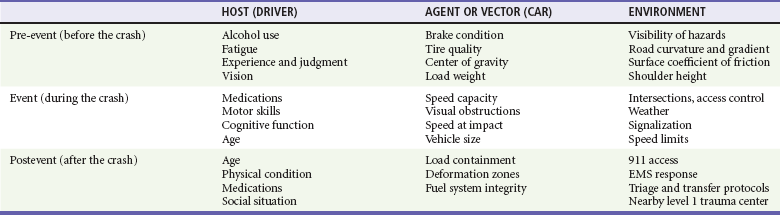
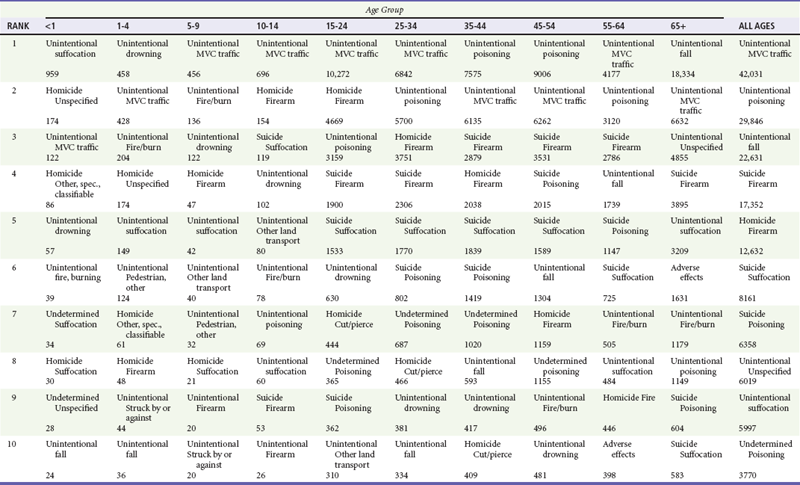
Chapter 40 The science of injury control is based on the concept that trauma is like a disease rather than just the consequence of fate or random occurrences. The principles of disease control are applied to injury as they are successfully applied to infectious diseases. Control of a disease as widespread and multifactorial as injury can occur only through broad interdisciplinary effort, including that of medicine, public health, policy makers, law enforcement, educated citizens, and others (Box 40-1). Emergency medicine plays a pivotal role in the care of injured patients and in injury control. In the United States, approximately one third of all emergency department visits are for the care of injuries, representing 13.3 visits per 100 people per year.1 Injury is the leading cause of death for many age groups (Table 40-1). In 2004, 29.6 million people were treated in U.S. emergency departments for injuries, of whom 93% were not admitted to the hospital.2 The medical cost of injury-related medical care in the United States is estimated to be $117 billion annually.2 Because the emergency care system may be the patient’s only contact with the health care system, emergency physicians should provide preventive services in addition to acute medical care for injured patients.3–5 Emergency physicians work with trauma surgeons, pediatricians, and others to decrease injuries through clinical and policy-relevant research and education.6 Table 40-1 Ten Leading Causes of Death, United States, 2007, All Races, Both Sexes HIV, human immunodeficiency virus; SIDS, sudden infant death syndrome. *Complicated pregnancy, HIV, and septicemia had 160 deaths each in 2007. Data from the National Center for Health Statistics, National Vital Statistics System. The major causes of injury include falls, motor vehicle collisions, gunshots, suffocation, and poisonings. Similar to other disease models, injury occurs from the interaction of agent and host through a vector and an environment that is conducive to exposure (Fig. 40-1). Injury is a harmful event caused by the acute transfer of energy to a patient that results in tissue and/or organ damage.7 The energy may be in any form, such as kinetic (e.g., falls and motor vehicle crashes), thermal (e.g., burns and hypothermia), chemical (e.g., poisoning), or electrical (e.g., lightning strike) energy or the absence of energy (e.g., hanging or drowning).8 Energy is the agent that is delivered to the host (patient) by a vector in an environment with variable risk. Cars and guns are examples of vectors of energy transmission that cause the injury. A car on an icy road is an example of the interaction of the environment and the vector to increase the likelihood of kinetic energy reaching the host and causing injury. Figure 40-1 The epidemiologic triad can be used as a framework for injury prevention. An injury occurs by the interaction of the host and agent through a vector and an environment that is conducive to injury. Alteration of any of these interactions prevents the injury.115 The goal of injury control is to prevent or decrease the transfer of energy to the host by (1) separating the host from the agent through modification of the environment, (2) equipping the host with protection against the agent, or (3) eliminating or modifying the vector that transmits the energy.8–13 The first step in the control of injuries is recognizing that injury is preventable. Public perception is that injuries result from accidents or random, unexpected events, similar to the way in which infections were regarded before the discovery of bacteria. As in other diseases, characteristics of the host affect prevention strategies, acute care, and rehabilitation outcomes. These include physical characteristics, such as age, gender, size, and motor skills, and mental or behavioral characteristics, such as intelligence, fatigue, alcohol use, emotional stability, social norms, and lifestyle. Risks for injury and death vary by age (see Table 40-1). For the likelihood of an injury to be decreased, changes in some of these predisposing factors can be made in the host (e.g., through improvement in driving skills or a commitment to wear a seat belt or not to drink and drive) and should be age specific for maximum effect. Energy is transmitted to the host through a vector, such as motorized and nonmotorized vehicles (e.g., car, bicycle, and skateboard), firearms, piercing instruments (e.g., knife and arrow), explosives, and lit cigarettes. Modifying the vector (by elimination or modification of design) and separating the vector from the host are important methods to reduce injury. For example, the understanding of biomechanical forces released during an injury event is crucial to understanding vehicle modification.14–16 Physicians should educate patients and families to modify or eliminate vectors they encounter during their daily lives—for example, recommending that families properly store household firearms and use gun locks.17 Another example is storing drugs that look similar in different locations on an ambulance or changing the packaging to reduce the risk of injuries caused by administering the wrong medication. When an injury occurs, host-agent interaction and energy transfer take place in an environment. This environment can be modified to decrease injury. If the environment does not permit energy transmission, the risk of injury, including intentional injuries to the host (patient), is eliminated.18 Most environmental modifications require no cooperation or action by the host and are more effective than altering host risk factors. Examples are implementing safer road design and lighting to prevent motor vehicle collisions, removing throw rugs to prevent falls, placing fences around pools, and separating bicycle paths from roadways.12,19 William Haddon, the first physician administrator for the National Highway Traffic Safety Administration (NHTSA), first described this type of approach in a landmark article on injury control in 1970.20 He laid out 10 methods for preventing injury (Table 40-2). Haddon later expanded these ideas to incorporate time and developed the Haddon matrix. The matrix recognizes that preventative interventions should be considered for the host, agent, vector, and environment before the event, during the event, and after the event. Any type or cluster of injuries can be prevented or reduced in severity through use of this matrix when the environment, vector, and population most at risk are identified and modified. An example of this process to reduce motor vehicle collision injuries is given in Table 40-3. The key to energy transfer reduction or prevention is understanding that (1) injuries are predictable, (2) they follow predictable patterns (e.g., by age or gender), and (3) reliance solely on human factors for prevention has significant limits. A fragile item sent through the mail arrives at its destination intact only if it has been properly packaged to reduce the energy to which it is subjected during transport. Likewise, injuries to people can be prevented by use of the cells of the Haddon matrix to mitigate the energy transfer of predictable events. Table 40-3 Typical Haddon Matrix (Constructed for Motor Vehicle Injury) EMS, emergency medical services. Adapted from Baker SP, O’Neill B, Ginsburg MJ, Li G: The Injury Fact Book, 2nd ed. New York, Oxford University Press, 1992. Decreasing personal injury is a goal of modern public health, but until the 1940s and 1950s, unintentional injuries were attributed primarily to human error, and prevention was based on educating people to act safely.10 Unsafe roads were built, and motorized vehicles and other consumer products were manufactured without regard to safety design flaws.21 This is analogous to supplying untreated tap water to homes and relying on educating people to purify their drinking water to prevent cholera.11 In the 1920s, attributing vehicle crashes to poor driver performance led to mandatory licensing of drivers. In the 1930s, when it was realized that vehicle crashes were caused not simply by human error but by mechanical factors as well, President Roosevelt called for automobiles to be made more crashworthy.8 In 1942, Hugh DeHaven, a former World War I pilot turned physiologist, pondering his own survival in an airplane crash when another occupant had been killed, suggested structural provisions be made to vehicles that would distribute the forces of energy over the human body to attenuate the energy transfer and reduce injuries in crashes. He focused on defining the physical factors that influence survival rather than the human error that caused the crash.8 As the United States embarked on its space program, Air Force researchers showed that humans could withstand splashdown with a sled that decelerates from 30 to 0 mph over a stopping distance of 2 feet.22 This demonstration was a significant advance in understanding the biomechanics of sudden deceleration. The recognition that injuries could be addressed similarly to diseases occurred in the 1940s, when John Gordon, an epidemiologist, suggested that injuries have epidemic patterns, seasonal variation, long-term trends, and demographic distribution and can be examined with methodologies applied to infectious diseases. Gordon also believed that, similar to infectious diseases, injury results from the interaction of the agent, host, and environment.8 In the 1960s, Haddon developed a two-dimensional approach to injury analysis by dividing the factors of agent, host, and environment into three phases: preinjury, injury, and postinjury. This phase-factor matrix has become a mainstay of injury control development. Any injury event can be broken down into the component factors, allowing specific interventions to target specific factors (Table 40-4).12,23 Table 40-4 Ten Leading Causes of Injury Deaths, United States, 2007, All Races, Both Sexes MVC, motor vehicle crash; spec., specific. Data from the National Center for Health Statistics, National Vital Statistics System. In 1985, the publication Injury in America: A Continuing Public Health Problem by the National Research Council and the Institute of Medicine called on the public health and health care community to address the injury epidemic.13 With the establishment of the National Center for Injury Prevention and Control (NCIP) in the Centers for Disease Control and Prevention (CDC), it was acknowledged that the control of injuries belongs in the disease control community and includes health care providers such as emergency physicians. Soon after its inception, the NCIP began sponsoring injury control research centers at academic institutions throughout the country. These centers, frequently led by physicians, including emergency physicians, conduct research in all three core phases of injury control (i.e., prevention, acute care, and rehabilitation) and serve as training centers for injury control specialists and as information centers for the public.24 To expand this work, the Society for the Advancement of Violence and Injury Research is open to any group or individual with an interest in advancing research in violence and injury (www.savirweb.org). In 2003 the NCIP began updating the CDC Injury Research Agenda to include acute care research, focusing on research that will improve acute injury care systems.25 After this, the NCIP Division of Injury and Disability Outcomes and Programs changed its name to the Division of Injury Response, with a mission “to increase the capacity to prevent injuries and their adverse health effects by working with partners to develop, evaluate, and promote evidence-based surveillance, prevention, and care practices.”26 This center became a home for acute injury care and acknowledges its importance for prevention. This division has also become a focal point for response to terrorist-related injuries, an important area of injury control. In 2009 the NCIP published a revised research agenda continuing the Center’s commitment to acute care research.27 The history of injury control began with the first injury. Pain from injury is a powerful stimulus for avoidance behaviors. Early prevention technology is seen in the instruments and garb of the earliest armies, shielding people from the harmful kinetic energy of weapons. Such technology included helmets, shields, and suits of armor. As the delivery of kinetic energy became more sophisticated, prevention technology did not keep pace.15,16 Firearms and automobiles represent new plateaus in harnessing kinetic energy as well as creating new sources of morbidity and mortality.21,28 The cultural belief was that individuals could avoid vehicular injury by safe driving, and if they did not drive safely, an “accident” would occur. It took more than 50 years to acknowledge that behavior modification alone was insufficient to mitigate high-energy transmission to humans in a hazardous environment. Cars were not uniformly equipped with seat belts until the 1960s.21 It took another two decades before air bags became standard.15,16,29 Implementation of effective injury control strategies depends on collaborative efforts by a number of individuals, including physicians, nurses, out-of-hospital care providers, epidemiologists, biomechanical engineers, public policy makers, law enforcement officers, lawyers, and other stakeholders.19,29,30 A major challenge is the wide diversity of disciplines and interests involved in safety and injury control, many of which are isolated from one another.10 In the 1990s, important strides were made in community-based injury control programs that rely on coalitions of existing resources with the support of the NHTSA, the CDC, and the State and Territorial Injury Prevention Directors Association. These community coalitions were created to garner existing resources and implement injury countermeasures through use of “the 3 Es” of public education, enforcement of laws, and engineering modification of hazardous devices and environmental conditions.19 Traditionally, physicians have focused on treating the patient after the disease has occurred. As the causes of many diseases have become better understood, education about risk assessment and clinically based prevention has been integrated into medical practice, particularly in infections (immunizations) and cardiovascular disease (smoking cessation). Emergency physicians are incorporating risk assessment, counseling, and referral of patients in high-risk groups for injury, such as those experiencing domestic violence.3,5 The Joint Commission has emergency department requirements for addressing abused patients.31 Emergency care providers are pivotal in the recording and accumulation of data about the injury event, which is useful for surveillance and epidemiologic analysis. Injury control techniques can be incorporated easily into emergency medicine practice as well.5,32–35 A rational approach to improve injury care in a community (Box 40-2) requires that physicians from a variety of specialties (e.g., emergency physicians, surgeons, pediatricians, and physiatrists) assume specific roles and activities in promoting injury control. This role for emergency physicians in injury control has been advocated by the American College of Emergency Physicians.36 Documentation of injury information in the medical record, assessment of risk factors in individual patients, counseling and referral, provision of systematized acute trauma care, and public health advocacy are all important.37–39 Gathering accurate data is essential to understanding the characteristics of a disease—its endemic populations, cyclic variations, geographic characteristics, and effectiveness of interventions. Consistent and comprehensive data should be gathered across the population of injured patients and used for hypothesis testing,40,41 hypothesis generation, ongoing monitoring of disease patterns and characteristics,35,42 and understanding of outcomes of prevention and policy interventions. The goal of injury data collection is to discover who is being injured (host), what is injuring them (vector), and the circumstances surrounding the injury (environment).43,44 Until recently, reliable data on the disease of injury were limited to mortality data collected by coroners and medical examiners.45 The Fatal Analysis Reporting System, a comprehensive data set on all car crash deaths in the United States, was established by the NHTSA in 197546 for examination of the epidemiology of motor vehicle crashes.40 Because death is uncommon compared with the large number of injured people who receive medical care, conclusions based solely on mortality data are limited.13,47,48 The advent of trauma registries in the 1980s increased the sample from patients who die to patients admitted to trauma centers. Because these data are skewed toward the most severe injuries, the conclusions based on these data are still limited when generalized to all injured people.49 Approximately 93% of injured patients seeking medical care for injury are treated and discharged from the emergency department, and many of them experience significant morbidity resulting in long-term disability and significant cost to society.13,35,42,47 To capture reliable emergency department data, the CDC developed Data Elements for Emergency Department Systems to define the minimum data set essential for physicians and information systems developers.50,51 The most crucial data element for the understanding of injury is the E code, a system for identifying the cause of injury in a patient’s medical record according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM).19 The E stands for external cause of injury, such as car crash, fall, or bicycle crash. The cause of injury cannot be extracted from diagnosis codes in medical records. These are N codes—the nature of the injury, such as skull fracture, laceration, or contusion. Because injury control depends on identifying the vector that is causing injuries and not just the resultant injuries, the only way to accomplish this systematically is by documenting the appropriate E code for each patient visit. Several states have mandated documentation of E codes for all emergency department discharges35,42–44; however, the completeness of this documentation is variable. The CDC found that 37% of hospital discharges after injuries were missing valid external cause of injury codes.48 The greatest barrier to the collection of E codes in the emergency department is inadequate physician documentation to assign accurate E codes retrospectively from the medical record.47,52,53 The first step in data gathering is complete and legible documentation of the cause of injury in patient medical records. Because injury problems in a community differ greatly from region to region, community-specific injury control efforts can be generated, implemented, and evaluated.19,41 E-coded hospital records can provide the who, what, and when of injury. The question of where can be either place of occurrence or place of residence, both of which are important and have implications for planned countermeasures. Hospital records are helpful in determining place of residence of injured patients, which is useful for community education in high-risk neighborhoods. Location-of-injury data are available only from other sources, such as emergency medical services (EMS), police, or other records. These data are more likely to be useful for environmental modification through engineering enhancements, police enforcement, or hazard removal. Linkage of these records to patient visits, either manually for specific research studies or electronically for surveillance, is the next step in gaining a comprehensive understanding of the epidemiology of injury.54,55 New desktop computer–based geographic information system programs can be used to study injury locations with minimal training and resources. The maps generated by these programs can identify areas with injury clusters to focus prevention efforts on areas with the greatest need.56,57 Statewide injury data linkages exist in some states and are available for surveillance information58 and research for unintentional and intentional injuries.32,41,59 For example, the Crash Outcome Data Evaluation System uses probabilistic linkage to create a database of crash, hospital, EMS, and emergency department information for motor vehicle crashes.60 Interest and opportunity to apply injury control principles for medical injuries, also known as medical errors, are growing. Medical injuries account for an estimated 50,000 to 98,000 deaths each year in the United States, with hundreds of thousands of nonfatal events occurring in emergency departments, intensive care units, and operating rooms.45 Emergency physicians can play an important role in use of injury control principles and science to reduce medical injuries.61–64 Application of injury control principles for the identification of injury patterns and for the development and evaluation of injury prevention strategies has great potential.63,64
Injury Prevention and Control
Perspective
Principles of the Disease of Injury
History of Injury Control
Methods of Prevention
Injury Control in Medical Practice
Injury Epidemiology and Documentation
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree