Bruises, clothing imprints and friction burns, together with any history available from the patient or witnesses, can help to determine the direction and severity of the injuring agent.
Repeated physical examination is essential.
CHEST INJURIES
Chest injuries are commonly caused by major trauma such as assaults, road traffic accidents and falls. They vary in severity from minor bruising or an isolated rib fracture to severe chest wall, pulmonary and cardiac injuries that may:
- disrupt the mechanism of respiration
- impair gas exchange
- produce hypovolaemia
- cause cardiogenic shock.
Immediate Assessment and Management
- Attend to ABCs as described in Chapter 1.
- Give a high-concentration of oxygen.
- Consider tension pneumothorax (→ p. 74).
- Cover open (sucking) wounds of the chest wall with firm, waterproof dressings. Note that this may allow a tension pneumothorax to develop.
- Obtain intravenous (IV) access. For a discussion of the rate and type of fluid infusion → pp. 7 and 331.
- Connect the patient to appropriate monitors (arterial O2 saturation [SaO2], ECG and blood pressure [BP]) and measure the respiratory rate.
- Request an urgent chest radiograph (CXR).
- Obtain an urgent 12-lead ECG.
- Consider early analgesia.
- Consider blood gas analysis.
Further Assessment and Management
Ask about
- Site and character of pain
- Dyspnoea
- Mechanism of injury
- Past medical history.
Look for
- Sweating, pallor, cyanosis
- Increased respiratory rate, work of breathing
- Uneven or abnormal chest movements
- Areas of tenderness, bruising, abrasions or crepitus
- Dullness or hyperresonance on percussion
- Reduced air entry, abnormal breath sounds
- Abnormal position of apex beat or trachea
- Increased pulse rate or paradoxical pulse
- Inaudible heart sounds (tamponade)
- Distended neck veins
- Abdominal tenderness
- SaO2, BP and ECG abnormalities.
Radiographs of the Chest
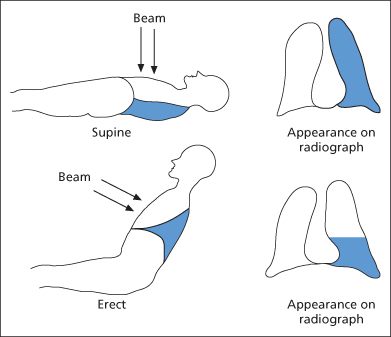
Ideally, the CXR should be performed with the patient erect to permit fluid level detection (→ Figure 6.1). With the patient supine, fluid present in the pleural cavity will lie behind the lung and produce a diffusely opaque lung field. A lateral decubitus film (‘sick side down’) may also reveal a fluid level, even in a supine patient.
Wounds to the Chest Wall
Sucking wounds, although unusual, attract immediate attention. In contrast, small stab wounds may be underestimated. They must be assumed to penetrate the parietal pleura until proved otherwise. This entails confirmation of the mechanism of wounding, observation of progress (if necessary, with repeated CXRs or CT scan) and occasionally careful examination of the anaesthetised wound by an experienced surgeon in an operating theatre (but not in the ED). A long, incised wound at right angles to the line of the ribs is usually superficial.
XR
All patients with stab wounds to the trunk should have a CXR. A CT scan of the thorax may be required.
TX
The presence of surgical emphysema, pneumothorax or haemothorax confirms pleural penetration. A chest drain will usually be required but should not be inserted through the wound (→ later). Most cases settle without surgical management; thoracotomy is indicated only if bleeding is severe or if a large air leak persists.
Antitetanus cover must be established and the wound covered with an antiseptic dressing. Be aware that an open wound may effectively prevent the development of a tension pneumothorax. Stab wounds are best left unsutured to allow drainage of any intramuscular bleeding.
Pneumothorax and Haemothorax
Traumatic pneumothorax may follow rib injury, stab wounds or barotrauma. The degree of pleuritic pain and dyspnoea is very variable. Clinical suspicion should be followed by radiographic confirmation except in the case of tension pneumothorax (→ later).
Haemothorax may also follow multiple rib fractures as a result of intercostal vessel damage. The bleeding is often brisk and continuous from the high systolic pressure of the intercostal arteries. In contrast, bleeding from the low-pressure pulmonary vessels usually stops with the collapse of the lung. A stab wound may cause profound bleeding from the internal thoracic artery or other intrathoracic structures. Symptoms and signs usually reflect the initial injury.
XR
Look carefully for small pneumothoraces – especially apically, laterally and medially (close to the heart border). Haemothorax may appear as blunting of the costophrenic angles. A large quantity of blood lying parallel to the diaphragm is often missed (a subpulmonary haemothorax). If this area looks slightly abnormal consider requesting a lateral decubitus film (→ p. 73) that may reveal the problem. A CT scan of the thorax may be required.
TX
- Give high-concentration oxygen by mask
- Monitor SaO2, BP and ECG
- Consider early analgesia
- Insert a chest drain (→ Box 6.1 and Figure 6.2).
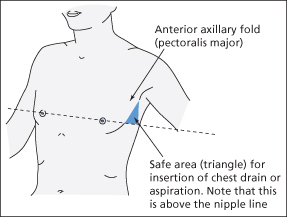
 Box 6.1 Insertion of a Chest Drain
Box 6.1 Insertion of a Chest Drain- Position the patient in a semi-recumbent position with the affected side uppermost
- Administer oxygen, attach a pulse oximeter and obtain venous access
- Consider IV morphine if there is adequate respiratory effort. Sedation with a small dose of midazolam is also an option in some patients
- Perform intercostal blocks posterior to the anticipated site of drain insertion. This is done by injecting 2 mL of 1% lidocaine around the neurovascular bundle (just below the inferior border of the rib). About three intercostal nerves should be blocked to include a space above and a space below
- Infiltrate local anaesthetic down to the parietal pleura at the site of insertion. Aspiration of air bubbles into a syringe containing residual local anaesthetic is a useful confirmatory sign
- Clean the skin and use surgical gloves and drapes
- Make a small incision down to parietal pleura. Aim for the upper border of the lower rib, to avoid the neurovascular bundle
- Open the incision with forceps. Some blunt dissection over the superior border of the rib may be required with the tips of scissors
- Consider inserting a gloved finger and sweeping the cavity to establish lung collapse
- Insert a chest drain (up to 28 G in an adult) using either a pair of curved artery forceps or a blunt trocar. Better still, use a modern drainage tube that includes a flexible introducer within its lumen
- Attach the drain to an underwater seal or a double Heimlich (‘flutter’) valve. In the case of the former, check for movements with respiration
- Advance the drain up to 15–20 cm in an upward, posterior direction
- Close the wound with large sutures on either side of the drain
- Cover the site with a waterproof dressing
- Cover the dressing completely with strips of tape
- Secure the drain with a ‘mesentery’ of adhesive tape
- Confirm the position of the chest drain on CXR
The ‘open’ technique is described but new equipment is now available on the market that makes ‘closed’ techniques much safer than was previously the case. In particular, catheters that are small diameter and wire guided (Seldinger type) are quick and easy to insert and relatively comfortable for the patient.
Some small haemopneumothoraces can be managed conservatively if the patient is stable and there are no plans to institute IPPV. Such patients should be discussed with senior staff and must be observed closely for signs of deterioration. A repeat radiograph will be needed after 4 h to check for radiological enlargement of the pneumothorax.
Tension Pneumothorax
This is a life-threatening emergency; the rapid increase in intrapleural pressure moves the mediastinum, compressing the opposite lung and impairing venous return. The patient has:
- dyspnoea
- unilaterally reduced breath sounds
- distended neck veins
- tracheal deviation
- impaired cardiac output
- cyanosis (a late sign).
The patient may look and feel as if they are ‘about to die’. (They are!) The clinical picture may be mistaken for that of a cardiac tamponade (→ p. 78). However, tension pneumothorax is more common and there is hyperresonance to percussion over the affected side.
XR
This delays treatment and so is inappropriate in the case of a clinically obvious tension. If taken, it would show a hyperexpanded lung field that is displacing the mediastinum, depressing the diaphragm and compressing the opposite lung.
TX
Immediate needle decompression (→ Box 6.2). This is part of the initial assessment or primary survey and resuscitation phase of management.
 Box 6.2 Treatment of Tension Pneumothorax (Needle Thoracocentesis)
Box 6.2 Treatment of Tension Pneumothorax (Needle Thoracocentesis)- On the affected side, identify the second intercostal space in the midclavicular line
- Insert a cannula with a syringe attached just above the rib, until air is aspirated (a cannula of at least 4.5 cm in length will be required)
- Remove the syringe and needle. There should be a hissing decompression followed by an immediate clinical improvement
- Tape the cannula in place
- Proceed to chest tube drainage (→ Box 6.1 and Figure 6.2)
- Once the chest drain is working, remove the cannula and dress the site
- Obtain a CXR
Surgical Emphysema
Gas under the skin can be caused in three main ways:
Subcutaneous gas in the chest or neck can usually be felt as crepitus. Other symptoms and signs result from the original insult.
Surgical emphysema after blunt trauma is usually a direct result of damage to the lung, but clinical and radiological examination may not initially confirm this. Stab and gunshot wounds may injure the pharynx or oesophagus. Infection spreading from such wounds into the mediastinum is a major, life-threatening complication.
XR
Subcutaneous or mediastinal gas may easily be seen on a plain CXR (or CT scan) as streaking in the soft tissues.
TX
Look for the injury that has caused the air leak. Observe in hospital.
In the case of suspected oesophageal or pharyngeal injury, prophylactic antibiotics should be started and surgical advice sought.
Rib Fractures
Fractured ribs are common and result from direct blows or falls. There is local tenderness, pain on inspiration and coughing, and difficulty with trunk movements. The patient must be asked about shortness of breath and previous cardiorespiratory problems. Careful observation should reveal any significant dyspnoea. The chest should be examined thoroughly to exclude underlying pneumohaemothorax and contusion.
XR
A CXR is mandatory in the presence of dyspnoea or past history of respiratory problems. There are usually more ribs fractured than can be seen on a plain film.
TX
Multiple Rib Fractures
- Give high-concentration oxygen by mask
- Monitor SaO2, BP and ECG and measure the respiratory rate
- Consider early analgesia
- Measure the blood gases.
Request an urgent anaesthetic opinion; the patient often requires intensive care. The inevitable underlying contusion will cause severe hypoxaemia. Pain may require a thoracic epidural infusion.
Fewer Than Three Fractured Ribs
- Exclude underlying problems and respiratory difficulty
- Assess mobility in the light of home circumstances
- Assess the level of pain.
The patient may go home if the above considerations do not contraindicate it. Adequate analgesia and GP follow-up will be required. For patients with a past history of cardiorespiratory problems, also consider the following:
- Prophylactic antibiotics
- Prophylactic steroids
- Community physiotherapy.
The patient must take analgesics and cough rather than refuse to do both. Winding a scarf around the chest and pulling on the crossed-over ends while coughing provides a surprising amount of pain relief. Strapping of the ribs, however, is contraindicated.
Patients with clinical signs of chest injury who do not have fractures on radiograph should be treated in exactly the same way as those with radiographic signs.