87 Injuries to the Shoulder Girdle and Humerus
• Scapular fractures require high force and are therefore associated with a high percentage of injuries to the ipsilateral chest wall and lung.
• Posterior dislocation of the sternoclavicular joint may damage vital structures within the superior mediastinum and thorax.
• Proximal and middle third clavicle fractures and type I and type III distal third clavicle fractures should be treated by placement of an arm sling.
• Open clavicle fractures require urgent open reduction and internal fixation.
• The degree of acromioclavicular separation can be diagnosed from an acromioclavicular view radiograph taken with the patient in the sitting or standing position.
• Axillary nerve function, both sensory and motor, should be tested in all patients with glenohumeral dislocation.
• Most proximal humerus fractures, especially in older individuals, can be treated conservatively.
• Injuries to the radial nerve should always be considered in patients with midshaft humerus fractures.
• Supracondylar fractures in children, especially those with significant displacement, may be associated with injuries to the brachial artery and the median and radial nerves.
Pathophysiology
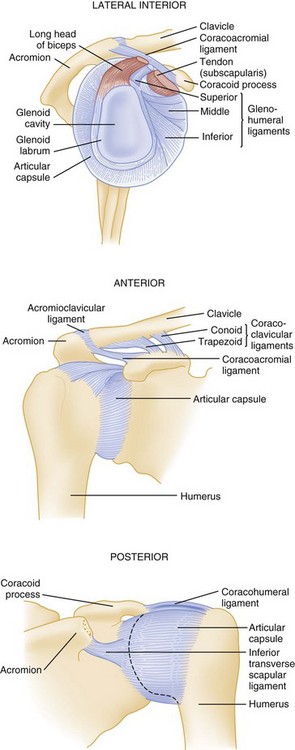
The scapula and clavicle are attached to the axial skeleton by ligaments at the sternoclavicular joint and by muscles from the blade or body of the scapula to the thorax. The clavicle is attached to scapula by the coracoclavicular and acromioclavicular ligaments. The coracoacromial ligament serves as the roof of the coracoacromial arch, beneath which the neurovascular bundle traverses (Figs. 87.1 and 87.2).
Presenting Signs and Symptoms
Sternoclavicular Joint Sprains and Dislocations
These injuries are graded as type I, a simple sprain of the joint; type II, subluxation of the joint, either anterior or posterior; and type III, complete dislocation of the joint. Dislocation usually results from a lateral force applied to the shoulder and an indirect force applied to either a rolled-back shoulder (anterior dislocation) or a rolled-in shoulder (posterior dislocation). Posterior dislocations are potentially life-threatening because the dislocated medial head of the clavicle may cause pneumothorax or injuries to the great vessels, esophagus, or trachea (all structures in the superior mediastinum).1
The patient complains of severe pain in the affected sternoclavicular joint. In anterior dislocations, the protruding medial end of the clavicle is visible, easily palpable, and tender. In posterior dislocations, there is often a cavity where the medial end of the clavicle would normally lie, which is especially noticeable when compared with the uninjured side. Patients with posterior dislocations may also have signs and symptoms of pneumothorax, vascular occlusion, and esophageal or tracheal injury.2 Routine radiographs may not be diagnostic, and computed tomography (CT) is usually required to make the diagnosis. This should always be performed with intravenous (IV) contrast media when a posterior sternoclavicular dislocation is suspected to rule out injuries to the superior mediastinal vascular structures3 (Fig. 87.3).
Acromioclavicular Joint Dislocation or Separation
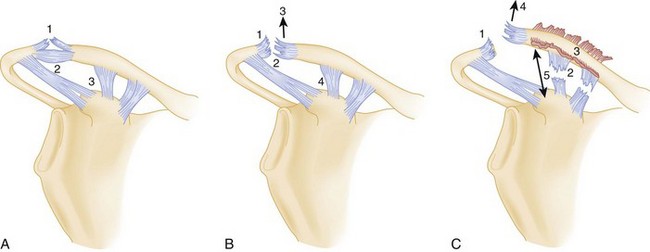
Acromioclavicular separations are generally caused by a fall onto the point of the shoulder or acromioclavicular joint with the arm adducted (thus the lay term shoulder pointer to describe this injury). It is caused less frequently by a fall onto the outstretched arm in extreme abduction, which drives the acromion below the clavicle. Acromioclavicular separations are classified as six types, although only the first three (I to III) are commonly seen. Types IV to VI are very uncommon and usually require surgical repair.1 In type I acromioclavicular separations, the acromioclavicular ligaments are partially torn and the coracoclavicular ligaments are intact, which results in less than 50% superior dislocation or separation of the clavicle from the acromion (Fig. 87.4, A to C). In type II injuries, the acromioclavicular ligaments are completely torn and the coracoclavicular ligaments are stretched or partially torn, which results in at least 50% superior dislocation or separation of the clavicle from the acromion. In type III injuries, both the acromioclavicular and coracoclavicular ligaments are completely torn, with complete superior dislocation or separation of the clavicle from the acromion.
The patient complains of severe pain in the acromioclavicular joint. Type I dislocations are characterized by tenderness and some swelling over the acromioclavicular joint, with little or no tenderness over the distal end of the clavicle and coracoid process. With type II dislocations, patients have tenderness and more swelling over the acromioclavicular joint and some tenderness over the coracoid process. In type III dislocations, the clavicle is obviously dislocated superiorly when the patient is sitting or standing, with less deformity noted when the patient is supine. Shoulder radiographs may miss an acromioclavicular separation if the radiograph is taken with the patient supine. Acromioclavicular views (a single radiograph that includes both acromioclavicular joints) should be taken with patients in the sitting or standing position and the arms unsupported. In type I injuries there is less than 50% cephalad dislocation of the clavicle on the acromion of the affected shoulder. Type II injuries are marked by greater than 50% cephalad displacement of the clavicle on the acromion on the affected side. In type III dislocations, complete dislocation is seen on sitting or standing films. Use of weight-bearing films (the patient holds weights with the affected arm) is of no benefit.4
Clavicle Fractures
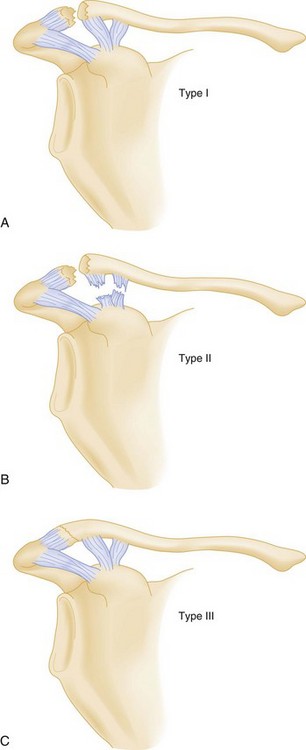
The most common mechanism of injury is a medially directed blow to the shoulder, usually from a ground-level fall. Children frequently have a bowing deforming or a greenstick fracture, whereas in adults the fracture fragments are often significantly displaced. Clavicle fractures are divided into proximal third, middle third, and lateral third. Lateral third fractures are divided into types I, II, and III (Fig. 87.5). Type II lateral third fractures are relatively unstable because the coracoclavicular ligament has been disrupted.
Scapula Fractures
Scapular fractures are typically associated with high-energy force and are thus often associated with significant life-threatening injuries, especially injuries to the ipsilateral ribs, pleura, and lungs. Most scapular fractures are caused by a direct blow, although fractures of the glenoid and scapular neck may occur as a result of a fall on an outstretched arm.5
Glenohumeral Dislocations
Patients generally have severe pain in the glenohumeral joint and hold the affected arm in adduction and internal rotation. There is lack of the normal contour, with a depression where the humeral head would normally reside. Patients report extreme pain in the joint with any attempted movement of the arm. Anteroposterior (AP) and axillary or transthoracic lateral radiographic views should be obtained in all patients with suspected dislocations, even if the patient has a history of multiple dislocations, because occasionally an associated fracture of the proximal end of the humerus or a posterior dislocation will be present.6,7 If displaced fractures of the glenoid or proximal end of the humerus are suggested on plain radiographs, CT scans of the shoulder should be obtained. Although the AP film usually shows the “light bulb” appearance of the humeral head, it is not always present (Fig. 87.6). Though rare, with luxatio the patient has the classic picture of holding the arm in marked adduction and over the head (Fig. 87.7). The radiograph reveals the humeral head to lie inferior to the glenoid and the humeral shaft adducted superiorly (Fig. 87.8).

Fig. 87.6 Anteroposterior shoulder radiograph of a patient with a posterior glenohumeral dislocation.

Fig. 87.7 Photograph of a patient with luxatio erecta.
(From Thomsen T, Setnick G, editors. Procedures consult—emergency medicine module.
Proximal Humerus Fractures
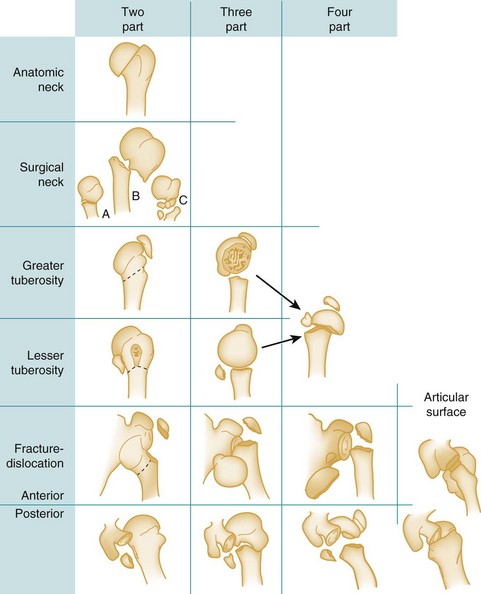
The Neer fracture classification is most commonly used and is based on the position of the articular segment, the greater and lesser tuberosities, and the humeral shaft. According to the Neer classification, a fracture is considered displaced if any major fracture fragment is displaced 1 cm or more or is angulated greater than 45 degrees.8 Fractures are classified as one-, two-, three-, or four-part fractures and are usually differentiated along the classic epiphyseal lines (anatomic neck, surgical neck, greater tuberosity, and lesser tuberosity) (Fig. 87.9).
The patient has severe pain in the proximal end of the humerus. An obvious deformity may be present, as well as swelling and extreme tenderness over the proximal end of the humerus. The trauma radiographic series recommended by Neer,8 as well as an AP internal rotation view and an axillary lateral view, provides the most complete diagnostic information. A CT scan of the shoulder may be necessary to better define the extent of injury.
Distal Humerus (Supracondylar) Fractures
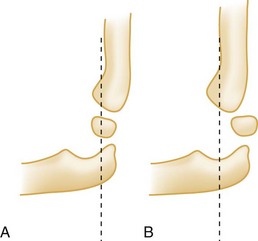
The patient is generally seen holding the injured arm in extension with the unaffected hand. Swelling, as well as tenderness to palpation over the distal end of the humerus, is typical. An S-shaped deformity may be present if significant displacement of the fracture fragments has occurred. The patient resists any attempt to flex or extend the elbow. Elbow radiographs (AP and lateral views) should be obtained. The fracture will often be visible only on the lateral view unless fracture fragments are significantly displaced. Normally, the anterior humeral line should pass through the capitellum (Fig. 87.10, A and B). If the capitellum is anterior to the anterior humeral line, it is diagnostic of a flexion-type supracondylar fracture in a child. If the capitellum is posterior to the anterior humeral line, it is diagnostic of an extension-type supracondylar fracture. Based on radiographic findings, extension fractures are often classified into three types: type I has minimal or no displacement; type II is a displaced fracture with the posterior cortex intact; and type III is a completely displaced fracture, with both the anterior and posterior cortices disrupted.