Initial Assessment and Resuscitation
Michael Rhodes
Michael Kalina
I. Introduction
Resuscitation of the adult patient is an intense period of medical care in which initial and continuous patient assessment guides concurrent diagnostic and therapeutic procedures. As a dynamic period, resuscitation requires the trauma team to rapidly develop a differential diagnosis based on effectiveness of treatment and results of available diagnostic studies. When possible, the surgeon and emergency physician should direct this crucial activity. The supervising physician must ensure that the optimal resuscitation space, personnel, and equipment are present.
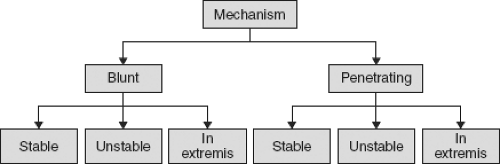
Resuscitation of the trauma patient requires an organized, systematic approach utilizing a well-rehearsed protocol. Advanced Trauma Life Support (ATLS) is a single-physician resuscitation course of the American College of Surgeons that prescribes an initial approach to an unstable patient with life-threatening injury (Table 4-1). The principles of ATLS resuscitation are also applicable to the Trauma Center environment and should be supplemented by a team approach to the trauma patient. The approach of a trauma team should be multispecialty and protocol driven based on patient “stability” and mechanism of injury (blunt vs. penetrating) (Fig. 4-1). This chapter presents a team-oriented approach for initial assessment and resuscitation.
II. Patient Stability
The term “unstable” has classically referred to physiologic parameters such as vital signs (pulse, blood pressure, and respiratory rate). Patients with abnormalities of these vital signs are usually sending out a clear distress signal. However, in the context of trauma resuscitation, the definition of unstable can be expanded to include patients who are considered metastable (the capacity to change at any time). These patients exhibit subjective, objective, or anatomical findings that may predict need for specialized trauma care in the Trauma Center. These expanded criteria for instability (and metastability) are liberal and refer to the potential need for operative intervention or the intensive care unit (ICU) (Table 4-2). Patients who meet these expanded criteria usually have injuries that are life- or limb-threatening. A subcategory of unstable patients, those who present in extremis (sometimes referred to as “agonal”), requires a tailored approach.
Blood pressure response to initial fluid challenge is also a measure of stability. Hypotensive patients who sustain a normotensive response to the first 1 to 2 L of fluid are responders and considered stable. Transient responders and non-responders are unstable (generally from ongoing bleeding) and should be treated accordingly.
Significant injury may also be suspected from interpretation of key phrases verbalized by patients.
“I’m choking”—airway dysfunction
“I can’t swallow”—airway dysfunction
“I can’t breathe”—ventilatory dysfunction
“Let me sit up”—ventilatory dysfunction, hypoxia, cardiac tamponade
“Please help me”—blood loss, hypoxemia
Table 4-1 Phases of Initial Assessment
Primary survey (15 s)
- Airway with C-spine controlM
→Voice, air exchange, patency, cervical immobilization
- Breathing
→Breath sounds, chest wall, neck veins
- Circulation
→Mentation, skin color, pulse, blood pressure, neck veins, external bleeding
- Disability (neurologic)
→Pupils, extremity movement (site and type), voice
- Expose the patient
Resuscitation
- Generic—ECG leads, pulse oximetry, IV, draw labs
- Concurrent with life-threatening injuries identified on primary survey
- Include gastric and urethral catheters, or perform with secondary survey
Secondary survey
- Head-to-toe examination (including spine)
- AMPLE history (A, allergies; M, medications currently taken; P, past illness;·L, last meal; E, events related to injury)
- Imaging
- Second survey may be delayed until after operating room in unstable patient or patient in extremis
Definitive care
- Surgery (may be in resuscitation phase)
- Splinting
- Medications (3 As): Analgesics, antibiotics, anti-tetanus
- Consultants
- Transfer
Tertiary survey
- Repeat primary and secondary surveys within 24 h for occult or missed injuries
- Creation of injury “problem” list with specific identification of physician handling each one
Modified from American College of Surgeons Committee on Trauma: Advanced Trauma Life Support Manual. Chicago: American College of Surgeons, 2008.
- Airway with C-spine controlM
“I’m going to die”—blood loss, hypoxemia
“I’m thirsty”—blood loss
“My belly hurts”—peritoneal irritation
“I need to have a bowel movement”—hemoperitoneum
“I can’t move my legs”—spinal cord injury
Table 4-2 Criteria for Adult Unstable (or Metastable) Trauma Patienta (Blunt or Penetrating Trauma)
Altered physiology
- Glasgow Coma Scale (GCS) score ≤14
- Pulse <60 or >120 beats/min
- Blood pressure <90 mm Hg after 2 L fluid challenge
- Blood pressure >190 mm Hg systolic
- Respiratory rate <12 or >24 breaths/min
- Poor gas exchange (e.g., SaO2 <90%)
- Temperature <92°F (33°C)
Altered physical findings
- Paralysis
- Hoarseness/inability to talk
- Labored respirations
- Severe pain
- External hemorrhage site(s)
- Combative
Altered anatomic findings
- Severe deformity(ies): Spine, neck, chest, extremities
- Penetrating wound from head to popliteal fossa
aIncreased index of suspicion:
- Age >55 y
- Coronary artery disease
- Obstructive lung disease
- Liver disease
- Insulin-dependent diabetes mellitus
- Anticoagulation or history of coagulopathy
- History of mental illness
- Pregnancy
- Glasgow Coma Scale (GCS) score ≤14
“Please do something for my pain”—significant injury
“Where am I?”—head injury, hypoxia, hypercarbia
III. Stable Adult with Blunt Trauma
Assess for airway, breathing, circulation, and neurologic disability.
Immobilize cervical spine.
Administer O2 nasally or by mask.
Insert at least one peripheral intravenous (IV) (18 gauge or larger).
Perform “stable patient” laboratory studies.
Splint deformed extremities.
Assess for occult injury.
Head, neck, chest, abdomen, pelvis, spine, and extremities.
Selective rectal and pelvic examinations.
Consider Insertion of a nasogastric tube (unnecessary in most stable patients).
Insert urinary catheter (if patient unable to void or pelvic fracture).
Limit IV fluid (e.g., 1 L in first 30 minutes).
Perform Select radiologic studies as indicated by mechanism of injury and physical examination.
Chest x-ray (usually routine).
C-spine—no x-ray if no symptoms or signs and not intoxicated (see Chapter 25).
Pelvis—no x-ray if no symptoms or signs.
CT of head with any alteration in consciousness, amnesia, headache, or history of anticoagulation.
CT of abdomen—if tenderness, macroscopic hematuria or microscopic hematuria with signs and symptoms (see Chapter 30).
Ultrasound of abdomen (selective)—if abdominal tenderness.
CT chest (with CTA) if history of acceleration/deceleration injury (e.g., MVC >25 mph, fall >10 ft
CTA neck if seatbelt sign to neck.
Spine and extremity films (selective)—if tenderness.
IV. Unstable Adult with Blunt Trauma
Assess airway (with C-spine immobilization).
Patency, voice, stridor, foreign body, tongue, lacerations, O2 saturation
Treatment options (see Chapter 3 for specific indications)
Administration of 100%O2 (by mask)
Suction
Chin lift
Oral airway (if obtunded)
Nasopharyngeal airway
Laryngeal mask airway (LMA)—very selective
Endotracheal intubation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree