133 Infections of the Urogenital Tract
Infections in the intensive care unit (ICU) contribute significantly to patient morbidity. Depending on the type of ICU, nosocomial infections may account for 70% of infections.1 Nosocomial infections of the urogenital tract are frequent and sometimes underestimated in the ICU.2
 Definition
Definition
Urinary tract infection can be the primary cause for admission to the ICU or can be acquired after intensive care procedures. Because patients are frequently sedated in the ICU, clinical diagnosis of urinary tract infection (UTI) is often difficult. Nevertheless, UTI is an important cause of morbidity and antibiotic resistance in the ICU. Complicated UTI is a very heterogeneous entity, with a common pattern of the following factors3,4:
 Etiology
Etiology
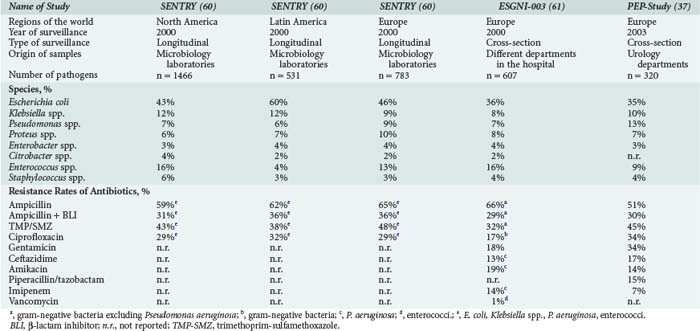
Causative pathogens of UTI are almost exclusively bacteria and yeast. Viral pathogens are only found in patients with severe immunosuppression, such as after bone marrow transplantation. High antibiotic pressure and special circumstances in the ICU modulate the microbial spectrum. Escherichia coli is the most frequent pathogen but occurs less frequently than in uncomplicated community-acquired UTI. Other Enterobacteriaceae may also be uropathogens (e.g., Klebsiella, Proteus, Enterobacter, Serratia, Citrobacter, or Morganella species). Non-fermenters such as Pseudomonas aeruginosa, gram-positive cocci such as staphylococci and enterococci, and Candida species may also play an important role (Table 133-1). The microbial spectrum is likely to differ over time and from one institution to the next. To follow the spectrum and development of antibiotic resistance, each ICU has to update its own analyses.
 Epidemiology
Epidemiology
The Extended Prevalence of Infection in Intensive Care (EPIC II) study1 revealed that 51% of patients were infected on the study day, and 71% of all patients were receiving antibiotics. The total occurrence of the most frequent types of ICU-acquired infection were respiratory tract infections 63.5%, abdominal infections 19.6%, bloodstream infections 15.1%, and renal or urinary tract infections in 14.3%.1 The true incidence of UTI, however, may be even higher if meticulously looked for. In a prospective study specifically evaluating nosocomial UTI, nosocomial UTIs accounted for 28% of the nosocomial infections, lower respiratory tract infections for 21%, pneumonia for 12%, and bloodstream infections for 11%. The rates of urinary catheter–associated UTIs varied between 4.2% (symptomatic UTI) and 14.0% (asymptomatic UTI), which shows that asymptomatic bacteriuria is frequent in ICU patients, although symptoms of UTIs in intensive care patients are frequently difficult to assess.2 In the one-day point prevalence study in urological patients in Europe (PEP/PEAP study) asymptomatic bacteriuria accounted for 29% of nosocomial UTIs, followed by cystitis (26%), pyelonephritis (21%), and urosepsis (12%),5 showing that nosocomial UTI is present with high frequency in certain patient groups.
Urinary tract infections in the ICU are divided into two groups:
Urinary Tract Infections with Nonurologic Complicating Causes
Individuals with diabetes are at higher risk for urinary tract infection.6 Increased susceptibility in patients with diabetes is positively associated with increased duration and severity of diabetes as a result of impaired granulocyte function, decreased excretion of Tamm-Horsfall protein, low interleukin (IL)-6 and IL-8 levels in the urine that lead to lower “cidality” of the urine, and altered microflora in the genital region. In addition, diabetic cystopathy and nephropathy may be complicating factors in the urinary tract. In addition to antibiotics, treatment must address the metabolic situation. In pyelonephritis, usually a switch to insulin or to insulin-analogous therapy is necessary.
Immunosuppression is generally associated with increased risk of UTI. Patients with leukopenia (<1000/µL) show a higher rate of febrile UTIs and bacteremia due to UTI.4 Symptoms and findings in these patients frequently are not diagnostic. Febrile episodes, however, are due to infections in approximately 60% of cases.
Pathogens may be translocated into the urinary tract from contiguous infectious foci (e.g., appendicitis, sigmoid diverticulitis, translocation by ileus). Symptoms and localization of pain can be misleading and may delay diagnosis. Operations or trauma may cause hypothermia, tissue hypoxia, and hemodynamic alterations that produce kidney dysfunction and impaired mucosal perfusion. The use of latex catheters in these critical situations (e.g., operations with heart-lung machine) can also lead to urethral strictures. Silicone catheters or suprapubic catheters are recommended in these patients.7 Suprapubic catheters cannot prevent UTI. They can, however, lower the rate of UTI from 40% to 18%.8
Urinary Tract Infections with Urologic Complicating Causes
Patients show a high risk to develop bacteriuria after renal transplantation, threatening clinical outcomes for both the patient and transplant. Early infections (up to 3 months after transplantation) are differentiated from late infections (more than 3 months after transplantation). Early infections may present with no symptoms. In this phase, occult bacteremia (60% of bacteremias after renal transplantation originate from the urinary tract), allograft dysfunction, and recurrent UTI after antibiotic therapy are frequently seen.4 The newer immunosuppressive agents are associated with a lower incidence of rejection but a higher risk of late infection. In particular, mycophenolate mofetil is associated with an increasing incidence of UTI and with infections caused by cytomegalovirus.4 Infection can induce graft failure by the direct effect of cytokines and free radicals or reactivation of cytomegalovirus infection. It can be very difficult to distinguish rejection from infection.4 Patients must also be investigated for a surgical complication.
UTIs caused by Candida species are frequently asymptomatic. There is, however, a risk of obstructive fungal balls leading to candidemia or invasion of the anastomosis in renal transplant recipients. Asymptomatic candiduria should therefore be treated in these patients.4 Urine transport disturbances (e.g., from obstructive ureteral stone) require specific urologic therapy such as percutaneous nephrostomy or stenting. In the case of bladder obstruction, an indwelling urinary catheter (suprapubic or transurethral) will be the primary therapy in the ICU. Long-term indwelling catheters (more than 30 days) are associated with a selected microbial spectrum of difficult-to-treat uropathogens (e.g., Providencia spp., Proteus spp., Pseudomonas spp.).9 After initiation of antimicrobial therapy, the catheter should be exchanged to remove biofilm material.
 Pathophysiology
Pathophysiology
In uncomplicated UTI, pathogens need to have very specific virulence factors enabling them to initiate an infection after invasion of the urinary tract. The medical conditions of an ICU patient may weaken physiologic barriers and defenses, thus facilitating entry of pathogens. In addition, the nosocomial environment in the ICU, including antibiotic pressure and decreased supply of oxygen or nutrients (e.g., iron) to tissues, can select pathogens with specific resistance patterns. A general adaptation strategy is the formation of hypermutator strains, which show 100- to 1000-fold increased mutation frequencies, enabling the pathogens to rapidly adapt to challenging environments and to thus develop effective mechanisms for antibiotic resistance.10,11
The basic structural unit of a biofilm is a microcolony—that is, a discrete matrix-enclosed community consisting of bacteria of one or more species. The biofilm is usually built up of three layers12,13:
 Diagnosis
Diagnosis
Urinary Examinations
Dipstick Test
The dipstick test is done with undiluted urine and investigates the following infection-related parameters15:
Microscopy
There are two possibilities of microscopic evaluation15:
TABLE 133-2 Standard Values for Urine in Counting Chamber and Field of Vision
| Erythrocytes | Leukocytes | |
|---|---|---|
| Uncentrifuged urine (chamber counting) | <10/mL | <10/mL |
Data from European Urinalysis Guidelines, 2000.
Clinical Diagnosis
To survey and compare infection rates in different institutions, UTIs should be classified according to widely accepted definitions, such as the definitions of the U.S. Centers for Disease Control and Prevention (CDC). The CDC/National Healthcare Safety Network (NHSN) definitions16 stratify health care associated UTIs into symptomatic, asymptomatic, and other infections of the urinary tract. To be of value in determining a nosocomial infection, the urine specimens must be obtained aseptically using an appropriate technique such as clean catch collection, bladder catheterization, or suprapubic aspiration.
 Therapy
Therapy
General Principles
Not all bacteriuric patients in the ICU need to be treated. Asymptomatic bacteriuria in general does not have to be treated.17 Therapy should only be started in patients with significant symptoms and morbidity and in whom asymptomatic bacteriuria may be deleterious (e.g., before traumatizing intervention of the urinary tract and in pregnant women). In the ICU, indications for treatment of asymptomatic UTI might include some other circumstances such as renal transplant, severe diabetes mellitus, or severe immunosuppression. In complicated UTI, antibiotic therapy can only be successful when the complicating factors can be eliminated or urodynamic functions restored. Treatment of complicated UTI therefore comprises adequate antibiotic treatment and successful urologic intervention.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree