CLINICAL PEARLNeuraxial analgesia provides superior pain relief to the mother during labor and delivery and conveys other significant benefits.
II.Effects of neuraxial analgesia on the progress of labor
A. Observational data demonstrate that neuraxial analgesia is associated with increased cesarean and instrumental vaginal delivery rates, and prolonged duration of labor. However, controversy exists as to whether this association is causal.
B. Ideally, one would conduct a randomized, double-blind, placebo-controlled trial to determine the true effect of neuraxial analgesia on the progress and outcome of labor. However, designing and conducting such a study is fraught with several difficulties:
1. Ideally, the control group would receive no analgesia; this is unethical.
2. Most controlled trials have utilized systemic opioids or inhaled analgesia (e.g., nitrous oxide) as the control group, but these modes of analgesia also have limitations:
a. Neuraxial analgesia is significantly superior to other forms of analgesia, making blinding of patient and provider virtually impossible.
b. Patients may be unwilling to enroll in a study knowing they might be randomized to an inferior form of labor analgesia, resulting in difficulties with achieving an adequate sample size.
c. The marked superiority of neuraxial labor analgesia contributes to a high crossover rate between study groups, preventing meaningful interpretation of the data.
d. The effect of systemic opioids on labor outcomes has not been well studied and opioids may differ on their effects on uterine muscle contractility.13
3. The external validity of these studies may be questioned because many women have already made a decision regarding labor analgesia before the onset of labor and may be unwilling to let random chance determine the type of analgesia they will receive.
4. There is difficulty in controlling for other factors that are known to affect the progress and outcome of labor, including:
a. Induction of labor
b. Artificial rupture of membranes
c. Parity
d. Payer status
e. Obstetric provider management (e.g., labor augmentation)
5. Selection bias
a. Women who are at higher risk for prolonged labor and operative delivery are more likely to request and receive neuraxial analgesia than women who undergo rapid, uncomplicated labor.8
b. Greater pain during labor appears to be associated with an increased risk for operative delivery.
(1) Women who received continuous infusion, low-concentration bupivacaine/fentanyl epidural analgesia, and who required three or more manual epidural boluses to treat breakthrough pain during labor (top-up doses), were more than twice as likely to undergo cesarean delivery (CD) than women who required fewer boluses.14
(2) The rate of CD was 14% in women who gave themselves 50 mg per hour or more of meperidine via patient-controlled intravenous analgesia (PCIA) compared to 1.4% in those who gave themselves less than 50 mg per hour.15
CLINICAL PEARLAlthough observational studies show that neuraxial analgesia is associated with increased rate of CD and a prolongation of labor, these findings have not been confirmed in properly constructed, randomized controlled trials.
III.Duration of the first stage of labor
A.No randomized controlled trials to date have investigated the effect of neuraxial analgesia on the duration of the first stage of labor as a primary outcome.
B.Studies that have investigated the impact of neuraxial labor analgesia on the duration of the first stage of labor as a secondary outcome have conflicting results.
1. Randomized controlled trials investigating the impact of initiation of labor analgesia during the latent phase of labor have demonstrated no difference or a shorter duration in the first stage of labor for women randomized to early neuraxial analgesia compared to those assigned to receive systemic opioid analgesia in latent labor.12,16,17
2. Systematic reviews have demonstrated no difference or a longer duration (~30 minutes) in the first stage of labor between women randomly assigned to receive epidural analgesia and systemic opioid analgesia.18,19
3. Effect of neuraxial technique
a. Combined spinal-epidural (CSE) versus epidural analgesia: Randomized controlled trials have demonstrated no difference or a shorter first stage duration in women randomized to receive CSE analgesia.20,21
b. Choice of local anesthetic: No differences in the rate of cervical dilation or duration of the first stage of labor were observed between women randomized to receive 0.08% bupivacaine/fentanyl 2 μg per mL and 0.08% ropivacaine/fentanyl 2 μg per mL via patient-controlled epidural analgesia (PCEA).22
c. Maintenance of analgesia
(1) Continuous infusion versus PCEA: a 2002 meta-analysis of nine studies reported no difference in the duration of the first stage of labor between patients randomized to continuous epidural infusion and PCEA.23
(2) Continuous infusion versus programmed intermittent bolus (infusion pump is programmed to administer regular bolus doses): a 2013 meta-analysis of eight studies demonstrated that women who received programmed intermittent scheduled boluses of epidural medication reported no difference in the duration of first stage of labor compared to women who received a continuous infusion with or without PCEA.24
d. Local anesthetic concentration: a 2013 meta-analysis of 11 studies demonstrated no difference in the duration of first stage of labor between women who received low concentrations of epidural local anesthetic (defined as ≤0.1% bupivacaine or ≤0.17% ropivacaine) and those who received higher concentrations.25
4. Difficulty with assessment—differences in outcomes among these studies are likely due to variations in study design, differences in neuraxial analgesic techniques and medications, and the impact of confounding factors influencing uterine activity.
a. Assessment of duration: documentation of start and end times
(1) The definition of start time differs among studies but is usually consistent within a study.
(2) End time is clearly defined at 10 cm cervical dilation, which can only be assessed via manual cervical examinations. Studies differ in frequency and/or requirement of regular cervical examinations, increasing intra-study variation in determining full cervical dilation.
(3) Women with effective neuraxial analgesia will likely have an artificially prolonged duration of the first stage of labor because these patients will complain of rectal pressure (and subsequently be examined and verified to be at complete cervical dilation) at a later time compared to those who have received systemic opioid analgesia.
b. Direct effects of local anesthetics on uterine tone and contractility
(1) In vitro studies in human myometrium demonstrate increased tone but decreased rate and strength of contractions when exposed to high concentrations of local anesthetics.26
(2) In vitro studies in human myometrium exposed to clinically relevant local anesthetic concentrations showed no effect on uterine activity or tone.27
c. Effect on plasma catecholamine levels
(1) Initiation of neuraxial analgesia is associated with a rapid decrease in maternal plasma concentrations of epinephrine. In turn, this is hypothesized to cause an increase in uterine activity secondary to decreased β-adrenergic receptor activation.10
(2) Studies have demonstrated an increased incidence of uterine tachysystole in women who received CSE technique for labor analgesia compared to traditional epidural analgesia.28,29 Two important limitations of these studies are (1) plasma epinephrine levels were not measured or correlated with the occurrence of uterine tachysystole, and (2) the duration of the first stage of labor was not assessed as an outcome to determine if this increased uterine activity affected the progress of labor. This increase in uterine tachysystole may not be associated with higher rates of abnormal fetal heart rate tracings or adverse neonatal outcomes.30
(3) Additional studies have suggested that the epidural administration of dilute concentrations of epinephrine (1.25 to 5 μg per mL) with local anesthetic does not affect the progress of labor.31,32
d. Effect on oxytocin concentration
(1) Fluid boluses: Bolus administration of 1-L of crystalloid solution (but not 0.5-L or maintenance fluid alone) has been shown to decrease uterine activity, possibly by decreased production and release of antidiuretic hormone and oxytocin, both of which originate from the posterior pituitary gland.33
(2) Rahm et al.34 demonstrated lower plasma oxytocin concentrations 60 minutes after initiation of epidural analgesia (bupivacaine with sufentanil) compared to women without epidural analgesia.
e. Genetic polymorphisms
(1) New evidence suggests polymorphisms in the β2-adrenergic receptor (ADRB2) and catechol-O-methyltransferase (COMT), and oxytocin receptor (OXTR) genes may affect the progress of labor.35,36
(2) Further studies are needed to elucidate the interaction of these and other genotypes with neuraxial analgesia and their impact on labor progress.
5. Summary of evidence for the effect of neuraxial labor analgesia on the duration of the first stage of labor
a. The available evidence suggests that neuraxial analgesia has a variable effect on the duration of the first stage of labor: It may prolong it in some patients, whereas shortening it in others.
b. These inconsistent results are likely a result of the influence of several factors known to affect uterine activity and duration of the first stage of labor, including management of labor, as well as differences in neuraxial analgesic techniques and medications.
CLINICAL PEARLStudies investigating the effect of neuraxial analgesia on the length of the first stage of labor report varying results. Differences in analgesic technique, study design, and obstetric management are the most likely reasons.
IV.Duration of the second stage of labor
A. Effective neuraxial analgesia prolongs the second stage of labor.
1. Meta-analyses of randomized controlled trials demonstrates that the median duration of the second stage of labor is 15 to 20 minutes longer in women who receive neuraxial analgesia compared to those who received systemic opioids.18,19
2. Recent data suggest that labor curves developed in the 1950s by Friedman may not reflect the pattern of modern labor.37
a. There are several factors which may explain these changes in labor patterns in modern obstetrics:
(1) Parturients are heavier and older, two factors that are known to affect the progress of labor.38
(2) Operative vaginal deliveries are being performed at a lower rate, which may increase the CD rate.38
(3) The use of neuraxial labor analgesia is more prevalent.2,3,38
b. Zhang et al.37 performed a secondary analysis of data from the Consortium on Safe Labor, a multicenter study involving more than 62,000 patients demonstrating:
(1) The time to progress from 4 to 6 cm cervical dilation was much longer than previously described by the Friedman labor curves.
(2) Nulliparous and multiparous patients progressed at a similar rate of cervical dilation before 6 cm dilation, after which multiparous women progressed much faster. This suggests the transition to active phase of labor might occur at approximately 6 cm instead of 4 cm as previously thought.
(3) The 95th percentiles for the duration of the second stage of labor in nulliparous women with and without neuraxial analgesia were 3.6 hours and 2.8 hours, respectively.
c. Cheng et al.39 demonstrated in a retrospective cohort study that the 95th percentile duration of the second stage was prolonged by more than 2 hours in women who received epidural analgesia.
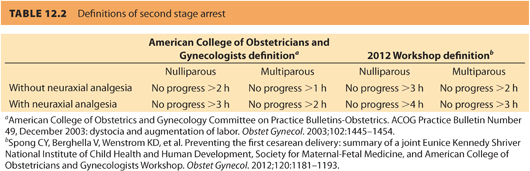
3. The American College of Obstetricians and Gynecologists (ACOG) has specific definitions for a prolonged second stage of labor, depending on parity and presence or absence of neuraxial analgesia. However, new criteria for defining second stage arrest have been proposed, which are concordant with more recent data (see Table 12.2).
4. Effect of prolonged second stage duration on maternal and neonatal outcomes.
a. Rouse et al.40, in a secondary analysis of data from a multicenter study involving nulliparous women, demonstrated that long (≥3 hours) compared to short second stage labor duration was associated with:
(1) Decreased rates of spontaneous vaginal delivery and increased rates of instrumental vaginal delivery
(2) Increased risk of chorioamnionitis, uterine atony, and third- or fourth-degree perineal laceration
(3) No increased risk of adverse neonatal outcomes (after adjusting for mode of delivery)
b. Laughon et al.41 conducted a multicenter retrospective cohort study involving more than 100,000 parturients of mixed parity. The authors demonstrated that prolonged second stage, as defined by ACOG guidelines, was associated with:
(1) Decreased rates of spontaneous vaginal delivery and increased rates of operative vaginal delivery
(2) Increased risk of chorioamnionitis and third- or fourth-degree perineal lacerations
(3) Increased risk of neonatal asphyxia in nulliparous women with epidural analgesia (the absolute rate for this outcome was low at 0.3%)
(4) Sixfold increased risk of perinatal mortality in parturients without epidural analgesia regardless of parity
(5) No increased risk of hypoxic-ischemic encephalopathy in parturients with epidural analgesia regardless of parity
c. Summary of evidence for maternal and neonatal outcomes with prolonged second stage of labor
(1) It is unclear whether the longer second stage of labor caused by neuraxial analgesia also causes other adverse outcomes (e.g., chorioamnionitis, lacerations) or whether these outcomes are independently associated with prolonged second stage.
(2) The need for intervention (instrumental or surgical) should not be mandated solely based on second stage duration, especially if progress is being made and maternal/fetal status remains reassuring.42 By extending the duration of the second stage, more women will be able to deliver vaginally, thereby reducing the rate of CD.
B. Immediate versus delayed pushing
1. The impact of immediate versus delayed pushing on second stage labor duration, mode of delivery, and maternal/neonatal outcomes is controversial.
a. The Pushing Early or Pushing Late with Epidural (PEOPLE) study was a randomized, multicenter controlled trial, which demonstrated that compared to immediate pushing, women who were randomized to delayed pushing had43:
(1) Higher rate of spontaneous vaginal delivery
(2) Shorter duration of pushing
(3) Lower rate of mid-rotational forceps
(4) Longer duration of second stage of labor
b. Tuuli et al.44 performed a meta-analysis that included more than 3,000 parturients from nine high-quality and three low-quality randomized controlled trials. When only the high-quality studies were analyzed, the authors found that delayed pushing:
(1) Did not increase spontaneous vaginal delivery rates
(2) Did not decrease operative delivery rates
(3) Was associated with longer duration of second stage of labor but shorter duration of pushing
(4) Differences in the definition of maternal and neonatal outcomes precluded meta-analysis.
2. Despite no clear advantages to delayed pushing, the potential for maternal exhaustion from prolonged pushing makes it unreasonable to require parturients to begin pushing from a high fetal station.
CLINICAL PEARLNeuraxial analgesia prolongs the second stage of labor. The clinical impact of this prolongation on maternal and fetal outcomes is unclear.
V. Instrumental vaginal delivery
A. Observational data suggest an association between neuraxial labor analgesia and increased rate of instrumental vaginal delivery, that is, vacuum or forceps delivery.
B. No randomized controlled trial has assessed the effect of neuraxial analgesia on the rate of instrumental vaginal delivery as its primary outcome, although multiple trials have assessed it as a secondary outcome variable.45–47
C. Most randomized controlled trials and systematic reviews of randomized controlled trials comparing neuraxial to systemic opioid analgesia, in which the rate of CD was the primary outcome, have concluded that effective neuraxial analgesia is associated with an increased risk of instrumental vaginal delivery.18,19,46,47
1. Sharma et al.19, in an individual patient meta-analysis of studies performed at a single institution involving more than 2,700 patients, reported an adjusted odds ratio of 1.86 (95% confidence interval [CI], 1.43 to 2.40).
2. A meta-analysis involving 23 studies calculated a risk ratio for instrumental vaginal delivery for women randomized to epidural analgesia or systemic opioid analgesia of 1.42 (95% CI, 1.28 to 1.57).18
3. A systematic review of five randomized controlled trials comparing early (defined as cervical dilation of 3 cm or less) compared with later (>3 cm cervical dilation) labor initiation of neuraxial analgesia showed no increase in instrumental vaginal delivery rates in women receiving early analgesia (risk ratio 0.94; 95% CI, 0.87 to 1.02).48
D. Impact studies, also known as before–after studies, are designed to assess the incidence of a patient outcome before and after the implementation of a specific treatment (e.g., implementation of a neuraxial analgesia service).
1. In contrast to randomized controlled trials comparing neuraxial to systemic opioid analgesia, most impact studies have demonstrated no difference in instrumental vaginal delivery between the control and study time periods.
a. Impey et al.49 found no increase in the instrumental vaginal delivery rate at the National Maternity Hospital in Dublin despite a fivefold increase in the epidural analgesia rate over a 7-year period.
b. At Tripler Army Medical Center, Yancey et al.50 reported no change in the instrumental vaginal delivery rate (11.1% vs. 11.9%) despite an increase in the epidural analgesia rate from 1% to 80% in a 1-year period.
c. A systematic review of seven impact studies involving more than 28,000 patients showed no difference in instrumental vaginal delivery rates (mean change, 0.76%; 95% CI, −1.2 to 2.8).51
E.These conflicting results emphasize the potential impact of multiple confounding factors on data interpretation regarding the influence of neuraxial analgesia on instrumental vaginal delivery rates. The contribution of these factors to the outcome of second stage of labor is not only poorly understood, but also poorly controlled in many studies. Some of these factors include:
1. Neuraxial analgesia–induced motor blockade
2. Maternal pain and the urge to bear down
3. Fetal station and position
4. Definition of prolonged second stage and indications for instrumental vaginal delivery
CLINICAL PEARLRandomized controlled trials and observational and impact studies conflict over whether neuraxial analgesia increases the risk of instrumental delivery. How neuraxial analgesia impacts factors that may affect the second stage of labor is not well understood.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








