(1)
Chennai Breast Centre, Chennai, India
Breast surgery and radiotherapy produce changes which make it difficult to distinguish posttreatment changes from breast cancer recurrence (Fig. 44.1). High-quality imaging and understanding of the changes that might occur following surgery or radiotherapy is important to ensure an accurate interpretation and recommendation.
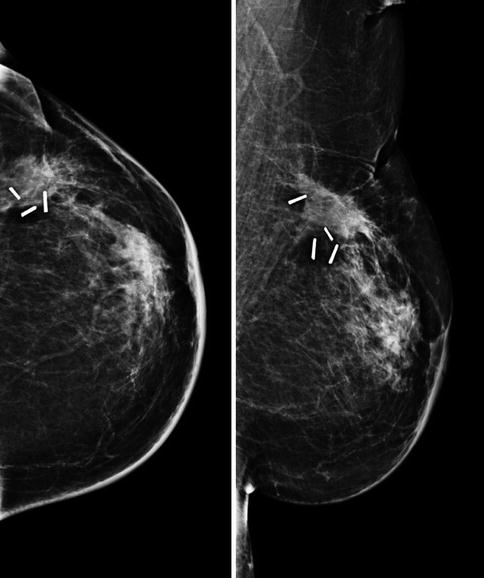
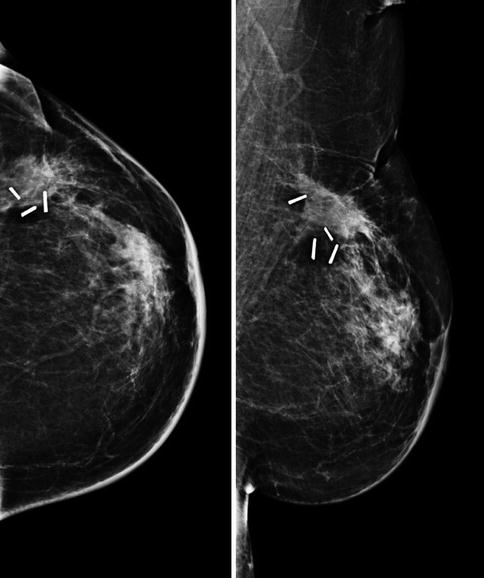
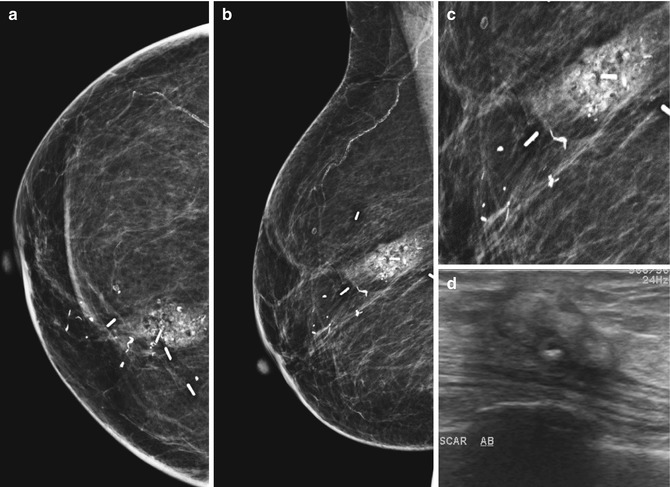
Fig. 44.1
CC and MLO, a year after breast conservation. Surgical clips are seen. Note the architectural distortion seen at the operated site along with retraction and skin thickening. Postoperative changes mimic a recurrence on mammogram
The most commonly done surgical procedures are excision biopsies, breast-conserving surgery for breast cancer, breast augmentation, and breast reduction. In the immediate postoperative period, the surgical site is edematous with fluid collection. The cavity was allowed to fill up with fluid which then gets absorbed gradually and heals by fibrosis. The long-term cosmetic outcome with this approach is not very good with this technique. The cosmetic outcome is better when the cavity is obliterated by mobilizing adjacent breast tissue. Surgical clips are left in the tumor bed, to mark the tumor bed for boost during radiotherapy.
Radiotherapy is an integral part of breast conservation therapy. Radiotherapy to the breast after breast conservation reduces the local recurrence rates significantly. Conventional radiotherapy to the whole breast with a boost to the tumor bed achieves effective local control. Whole breast radiotherapy is planned usually for 5 weeks up to a total dose of 50 Gy given as fractions of 2 Gy everyday with electron boost to the tumor bed.
Changes That Occur in the Treated Breast
Post treatment, the changes can be classified as early and late. Early changes include edema, hematoma, seroma, and infections. Late changes include fibrosis, scarring, architectural distortion, dystrophic calcifications, oil cyst formation due to fat necrosis, and recurrences (Fig. 44.2).
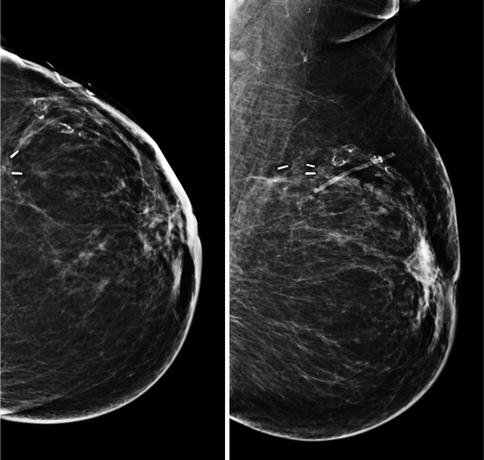
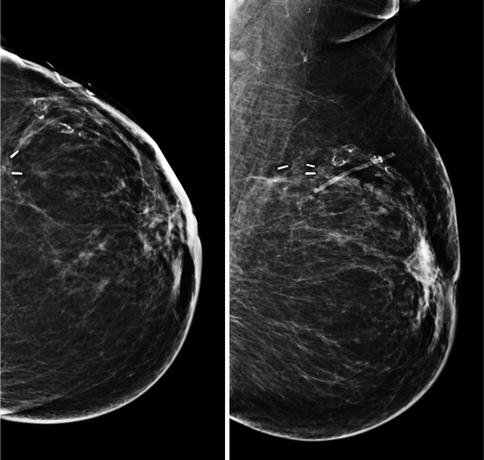
Fig. 44.2
CC and MLO of a treated breast. Scar marker is in place. Surgical clips are seen. There is skin thickening and architectural distortion
Edema
Skin thickening and edema can occur in the operated site. The postoperative induration usually settles down in 2–3 weeks time. During radiotherapy, the breast becomes red and edematous with a slight pitting (peu de orange appearance). This is as a result of the skin edema. Radiotherapy-related edema is likely to involve the entire breast unlike the focal edema that is seen with surgical changes. Two to three weeks after completion of treatment the edema slowly subsides and the redness decreases and becomes more normal over 6–18 months. Axillary clearance sometimes aggravates the edema of the breast as it interrupts the lymphatic drainage and may contribute to edema of the breast like lymphedema of the arm (Fig. 44.3a–c).
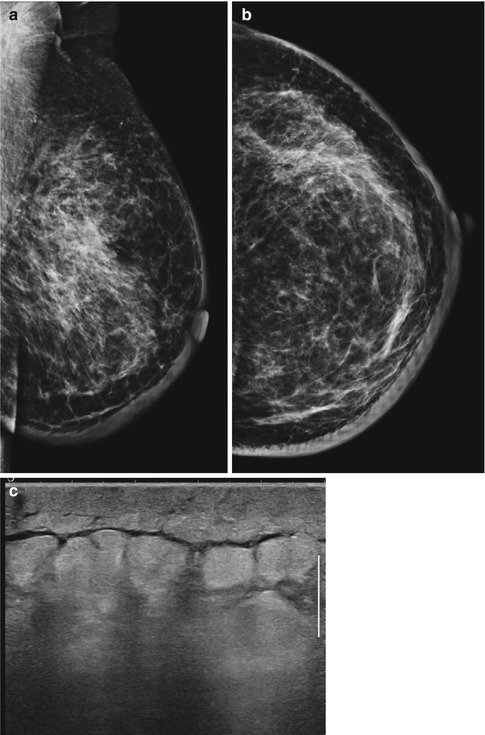
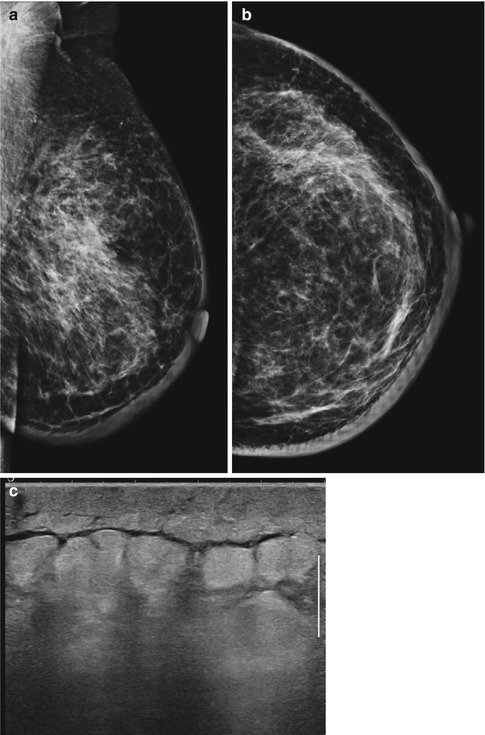
Fig. 44.3
(a, b) CC and MLO done a year after surgery: images showing skin and breast edema with trabecular thickening and Kerley B lines. (c) Ultrasound image shows skin edema
Hematoma
Meticulous hemostasis is essential when closing the lumpectomy cavity. Hematoma leads to complications like infections and the blood breakdown products incite a great degree of inflammation which leads to fibrosis with poor cosmetic results in the long term.
Seroma
If the lumpectomy cavity is not approximated and closed, seroma fills the cavity. Seroma gets absorbed over time, but sometimes it forms capsule and presents as a mass on a mammogram. As it gets absorbed, the scar retracts and results in poor cosmesis, particularly in large excisions (Figs. 44.4a–c and 44.5a, b).
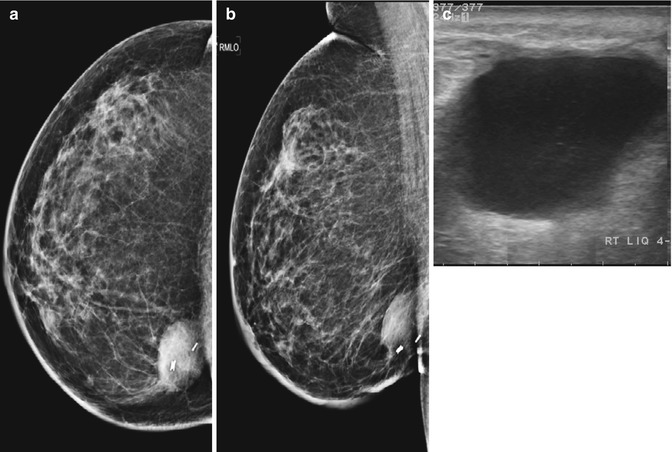
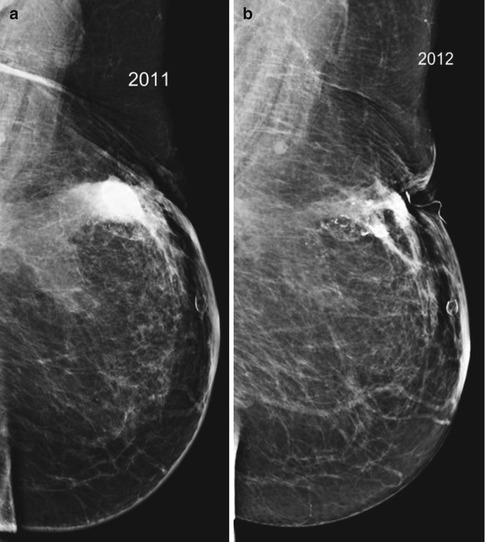
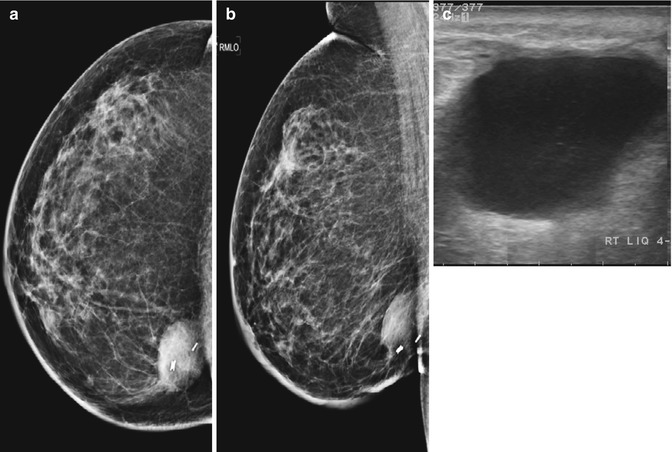
Fig. 44.4
(a, b) CC and MLO a year after breast conservation. There is a well-encapsulated collection at the operated site which is a seroma. (c) Ultrasound image showing a fluid collection
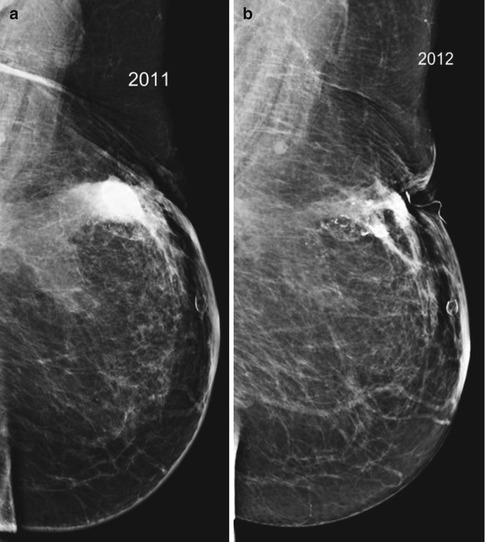
Fig. 44.5
(a, b) MLO images after breast conservation showing resolution of seroma in the subsequent year. Dystrophic calcifications are present
Fat Necrosis
Fatty breasts, extensive mobilization of the breast tissue during surgery, and ischemia due to strangulating sutures are all contributory factors for fat necrosis. The blood breakdown products that incite inflammation also contribute to the ischemic fat necrosis. When fat is ischemic, it liquefies and forms oil cysts. The fatty acids released due to fat necrosis further contributes to inflammation in the adjacent tissues. Calcium may get deposited in the wall of the cyst or in the adjacent tissues (Fig. 44.6a–d).