Disease phenotype
Clinical features
Objective laboratory and prognostic markers
Asymptomatic hepatic steatosis
Incidence: 2–5 % of US population
Symptoms: occasional hepatomegaly/RUQ pain, good muscle tone, appear medically well
Risk factors: daily alcohol consumption > 2 to 3 drinks/day, female gender
Prognosis: generally favorable and reversible with abstinence
Treatment: alcohol detox to sobriety, multivitamin, counseling, psychiatric meds to prevent relapse
Labs:
Serum AST and ALT may be mildly elevated or > 2:1 ratio
Normal or minimally elevated MCV without anemia
Urine ethylglucuronide to verify alcohol use in past 5 days
Normal albumin, bilirubin and INR
Imaging: increased hepatic steatosis on CT/MRI.
Biopsy: variable steatosis with mild inflammation and pericellular fibrosis
Prognosis: may improve/resolve with abstinence or lead to progressive liver damage/fibrosis with continued alcohol use
Alcoholic hepatitis
Incidence: 5–10 per 100,000
Symptoms: acute jaundice, nausea, abdominal pain, fever, encephalopathy.
Risk Factors: binge intake > 4 weeks in chronic user, younger age, genetic polymorphisms
Prognosis: 10–30 % 1 month mortality; 50 % 1-year mortality with abstinence; 90 % mortality without abstinence
Treatment:
Manage acute alcohol withdrawal
Thiamine, folate, enteral nutrition
Steroids x 6 weeks in highly selected patients
Alcohol abstinence
Management of encephalopathy, bleeding, ascites
Not candidates for liver transplant in most centers
Labs:
Serum AST: ALT > 2:1 frequently seen but both < 1000 IU/mL
Urinary ethylglucuronide detectable if alcohol use in past 5–7 days
CBC: moderate to severe macrocytosis with anemia, frequent thrombocytopenia, leukocytosis with left shift if severe
Moderate to severely ↑ bilirubin and INR, low albumin.
Imaging: hepatic steatosis in CT/MRI +/− hepatosplenomegaly, +/− ascites and venous collaterals
Biopsy: steatosis with neutrophilic inflammation, cirrhosis in 40–60 %
Prognosis: discriminant function ≥ 32 has 30–50 % mortality at 1 month
Decompensated alcoholic cirrhosis
Incidence: unknown but 10–15 % of patients with heavy alcohol will go on to develop cirrhosis
Symptoms: anorexia, weight loss, ascites, muscle wasting/weakness, palmar erythema, telangiectasias
Risk Factors: lifetime alcohol consumption exceeding 3–4 drinks/day over 10 years or more
Prognosis: determined by severity of portal HTN complications (variceal bleeding, ascites, encephalopathy). If MELD > 20, then ~70 % 1 year survival even with abstinence
Treatment:
Thiamine, folate, and multivitamins
Medical management of ascites with diuretics
Lactulose/rifaxamin for encephalopathy
Endoscopy for varices
Transplant in selected patients with favorable prognosis for long-term abstinence and compliance
Labs:
Serum AST and ALT frequently normal or minimally elevated
CBC: Moderate to severe macrocytosis with anemia, low WBC and platelets due to portal HTN.
Bilirubin and INR variably elevated, low albumin
Imaging: small shrunken, nodular liver with ascites, collaterals and splenomegaly
Biopsy: cirrhosis with minimal steatosis/inflammation
Prognosis:
MELD score predicts mortality at 3 months:
<9 = ~2 % mortality
10–19 = 6 % mortality
20–29 = 20 % mortality
30–39 = 53 % mortality
>40 = 71 % mortality
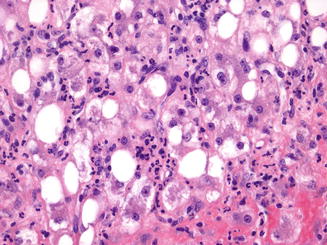
Fig. 69.1
Alcoholic hepatitis. An example of acute alcoholic hepatitis with Mallory-Denk bodies, steatosis, and neutrophilic inflammation (400× magnification)
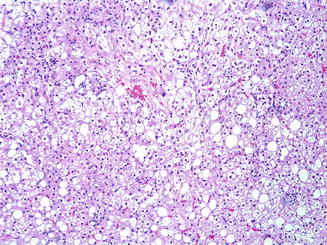
Fig. 69.2
Hepatic steatosis. Low-grade steatohepatitis showing predominantly steatosis (100× magnification)
Patients with ALD often, if not always, have, concomitant alcohol use disorders (AUD) which are classified by clinical symptoms (Table 69.2). Alcohol use disorders (AUD) are a major source of morbidity and mortality in the general population with an estimated prevalence of 6–8 % in North America [2]. Approximately 10–33 % of all medical ICU patients have an AUD which places them at risk of developing alcohol withdrawal syndrome [3]. A thorough history for heavy and chronic alcohol use should be taken, as alcoholic hepatitis can occur even weeks after the patient has stopped drinking. Though the pattern of alcohol use resulting in alcoholic liver disease (chronic vs binge drinking [i.e., consuming five or more drinks in less than 2 h]) is still unclear, chronic daily use of >30 g (approximately two standard drinks) alcohol increases the risk for cirrhosis. Alcoholic hepatitis patients report a mean use of 100 g or greater daily (~7 standard drinks or more per day), frequently in the days or weeks prior to presentation [1]. A standard drink is defined as 12 oz of beer, 5 oz of wine, or 1.5 oz hard liquor.
Table 69.2
Diagnostic criteria for alcohol use disorder and alcohol withdrawal syndrome
Alcohol use disorders | |
Diagnostic Criteria Mild: 2–3 symptoms Moderate: 4–5 symptoms Severe: 6+ symptoms | At least two of the following: 1. Alcohol taken in larger amounts or over longer period than intended 2. Persistent desire or failed efforts to cut down/control use 3. Great deal of time spent obtaining, using, or recovering from effects of alcohol 4. Craving, or strong desire/urge to use alcohol 5. Recurrent alcohol use resulting in failure to fulfill major role obligations at work, home, school 6. Continues alcohol use despite persistent/recurrent social or interpersonal problems related to alcohol use 7. Important social, occupational, or recreational activities given up/reduced due to alcohol use 8. Recurrent alcohol use when physically hazardous 9. Continued alcohol use despite knowledge of persistent/recurrent physical or psychological problem related to alcohol use 10. Tolerance: (a) Either a need for markedly increased amounts of alcohol to achieve the desired effect/intoxication (b) OR markedly diminished effect of continues use of same amount of alcohol 11. Withdrawal: (a) Symptoms consistent with alcohol withdrawal syndrome (see below) (b) Alcohol (or closely related substance such as benzodiazepine) taken to relieve/avoid withdrawal symptoms |
Remission definitions | In early remission: After full criteria for AUD diagnosis met, NO criteria for AUD have been for 3 months, but less than 12 months (Craving criteria can still be met but considered to be in early remission) In sustained remission: After full criteria for AUD diagnosis met, NO criteria for AUD met for 12 or more months (Craving criteria can still be met but considered to be in sustained remission) |
Alcohol withdrawal Syndrome | |
Diagnostic criteria | 1. Cessation/reduction of heavy/prolonged alcohol use 2. Two or more of the following, developing within several hours to a few days following cessation/reduction in alcohol use: (a) Autonomic hyperactivity (sweating, pulse >100 beats per minute) (b) Increased hand tremor (c) Insomnia (d) Nausea or vomiting (e) Transient visual, tactile, or auditory hallucinations (f) Psychomotor agitation (g) Anxiety (h) Generalized tonic-clonic seizures 3. Signs/symptoms of above criteria cause clinically significant distress/impairment in social, occupational, or other important areas of functioning 4. Above signs/symptoms not attributable to another medical condition and not better explained by another mental disorder, including withdrawal or intoxication with another substance |
Lab testing for alcohol use can be helpful in the proper setting as patients may be reluctant to disclose the true nature of their alcohol and/or co-occurring illicit drug use. Ethanol testing in the blood or urine can be used, though the short half-life results in a narrow time window for positive results (blood ~10-12 h, urine ~18-24 h) [4]. Ethyl glucuronide, a metabolite of ethanol formed in the liver by the conjugation of ethanol with glucuronic acid via UDP-glucuronosyltransferase, can be detected in the urine approximately 72–90 h after the last ingestion of alcohol and can be helpful in verifying reports of abstinence [4]. Since there can be substantial inter-individual variation in the production of urinary ethyl glucuronide, results should always be interpreted in the appropriate clinical context.
Prognosis in Alcoholic Hepatitis
Once a clinical diagnosis of AH is established, prognosis can be determined based on the Maddrey’s discriminant function or Model for endstage liver disease (MELD) scores which both predict 1 month mortality of approximately 20–35 % [5].1Other prognostic scoring models have been used, such as the Chronic Liver Failure- Sequential Organ Failure Scoring System (CLIF-SOFA) and have been validated in cohorts which included ALD and AH, showing as good or better prognostic performance when compared to the MELD score [6].
The standard medical management of AUD includes vitamin and mineral supplementation as well as management of AWS (Table 69.3). Patients with AUD have a higher risk of requiring mechanical ventilation and are more prone to develop sepsis and pulmonary infections which contributes substantially to morbidity and mortality [8]. In addition, complications of alcoholic cirrhosis, such as GI bleeding or spontaneous bacterial peritonitis, may also prompt ICU admission.
Table 69.3
Clinical institute withdrawal assessment of alcohol scale, revised (CIWA-Ar)
Record heart rate and blood pressure for 1 min | |
|---|---|
NAUSEA AND VOMITING—Ask “Do you feel sick to your stomach? Have you vomited?” Observation 0 No nausea or vomiting 1 Mild nausea with no vomiting 2 3 4 Intermittent nausea with dry heaves 5 6 7 Constant nausea, frequent dry heaves and vomiting | TACTILE DISTURBANCES—Ask “Do you have any itching, pins and needles sensations, any burning, any numbness, or do you feel bugs crawling on or under your skin?” 0 None 1 Very mild itching, pins/needles, burning or numbness 2 Mild itching, pins/needles, burning or numbness 3 Moderate itching, pins/needles, burning or numbness 4 Moderately severe hallucinations 5 Severe hallucinations 6 Extremely severe hallucinations 7 Continuous hallucinations |
TREMOR- Arms extended and fingers spread apart. Observation. 0 No tremor 1 Not visible, but can be felt fingertip to fingertip 2 3 4 Moderate, with patient’s arms extended 5 6 7 Severe, even with arms not extended | AUDITORY DISTURBANCES- Ask “Are you more aware of sounds around you? Are they harsh? Do they frighten you? Are you hearing anything that is disturbing to you? Are you hearing things you know are not there?” 0 Not present 1 Very mild harshness or ability to frighten 2 Mild harshness or ability to frighten 3 Moderate harshness or ability to frighten 4 Moderately severe hallucinations 5 Severe hallucinations 6 Extremely severe hallucinations 7 Continuous hallucinations |
PAROXYSMAL SWEATS- Observation. 0 No sweat visible 1 Barely perceptible sweating, palms moist 2 3 4 Beads of sweat obvious on forehead 5 6 7 Drenching sweats | VISUAL DISTURBANCES- Ask “Does the light appear to be too bright? Is its color different? Does it hurt your eyes? Are you seeing anything that is disturbing to you? Are you seeing things that you know are not there?” Observation. 0 Not present 1 Very mild sensitivity 2 Mild sensivity 3 Moderate sensivitiy 4 Moderately severe hallucinations 5 Severe hallucinations 6 Extremely severe hallucinations 7 Continuous hallucinations |
ANXIETY- Ask “Do you feel nervous?” 0 No anxiety 1 Mildly anxious 2 3 4 Moderately anxious 5 6 7 Equivalent to acute panic states as seen in severe delirium or acute schizophrenic reactions | HEADACHE, FULLNESS IN HEAD—Ask “Does your head feel different? Does it feel like there is a band around your head?” Do not rate for dizziness or lightheadedness. Otherwise, rate severity. 0 Not present 1 Very mild 2 Mild 3 Moderate 4 Moderately severe 5 Severe 6 Very severe 7 Extremely severe |
AGITATION- Observation 0 Normal activity 1 Somewhat more than normal activity 2 3 4 Moderately fidgety and restless 5 6 7 Paces back and forth during most of the interview, or constantly thrashes about | ORIENTATION AND CLOUDING OF SENSORIUM- Ask “What day is this? Where are you? Who am I?” 0 Oriented and can do serial additions 1 Cannot do serial additions or is uncertain about date 2 Disoriented for date by no more than 2 calendar days 3 Disoriented for date by more than 2 calendar days 4 Disoriented for place/or person |
Total score:_____ (maximum: 67) | |
ICU Management of Alcohol Use Disorders, Including Alcohol Withdrawal Syndrome (AWS) and Delirium Tremens (DTs)
The ICU management of alcohol withdrawal must occur in parallel with the medical management of their liver disease. Alcohol withdrawal syndrome (AWS) is defined as a complex of symptoms developing within hours to days of reduction or cessation of alcohol use that has been heavy and prolonged, in the absence of another medical cause for the symptoms (DSM-V) [9]. Symptoms are protean and may fluctuate including autonomic hyperactivity, hand tremor, insomnia, nausea and vomiting, visual, tactile, or auditory hallucinations, psychomotor agitation, anxiety, and generalized seizures. Delirium tremens (DT) or withdrawal delirium (as it is termed in the DSM-V), is a more severe form of AWS, characterized by alcohol withdrawal symptoms coupled with delirium, including decreased attention and awareness with disturbance in, memory, orientation, perception or visuospatial abilities (DSM-V) (Table 69.4). Patients with DT have as high as a 10–20 % inpatient mortality rate particularly within the first 48 h of presentation. Delirium symptoms should also prompt a thorough evaluation for other medical problems that could produce delirium such as infection, GI bleeding, hypoglycemia, electrolyte disturbances, occult head injury, or ingestion of other toxins/psychoactive drugs. Alcohol withdrawal symptoms can appear several hours after cessation of all alcohol use and reach full severity approximately 50–60 h after stopping alcohol [10].
Table 69.4
Michigan alcohol withdrawal severity (MAWS) scoring system
Symptom classes | Scoring | |
|---|---|---|
Type A (CNS excitation) Anxiety or nervousness Restless Bothered by bright light Bothered by sounds | Assign one point for each Maximum 4 points | |
Type B (Adrenergic hyperactivity) Nausea or vomiting Visible tremor Sweat visible (palms/forehead) SBP more than 30 mmH over baseline or >170 mmHg OR DBP more than 20 mmHg over baseline or >100 mmHg
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| ||




