131 Hypothermia and Frostbite
• Accidental (primary) hypothermia occurs when the ambient temperature outstrips a person’s ability to thermoregulate.
• Secondary hypothermia is due to an underlying medical problem that alters thermoregulation.
• Mild hypothermia is treated by passive external rewarming, moderate hypothermia by a combination of passive and active external and active internal rewarming, and severe hypothermia by active external and active internal rewarming techniques.
• For patients without a pulse or blood pressure, aggressive, invasive measures should be pursued.
• One should hesitate to declare death in a hypothermic patient. Consider rewarming to a temperature of 32° C to 35° C.
• Frostbite remains a clinical diagnosis and needs to be distinguished from nonfreezing injuries (frostnip, pernio, and trench foot).
• The cornerstone of therapy is rapid rewarming in a circulating bath of heated water.
• In all aspects of care a subsequent “freeze-thaw-freeze” cycle must be avoided.
• Additional therapies involve the use of antiprostaglandins, both topical and systemic, and possibly thrombolytics.
• The full extent of frostbite injury can take weeks to become evident.
Perspective
Accidental hypothermia is responsible for approximately 700 deaths per year in the United States.1 It primarily affects those least able to ward off the effects of cold weather: the very young, the very old, and the poor, disabled, pharmacologically inquisitive, environmentally adventurous, and mentally ill. Urban people are common victims. Hypothermia can occur in many latitudes, with episodes reported even in Florida.2 It occurs when a person’s ability to generate heat and remain warm is outstripped by the ambient temperature.
Epidemiology
Accidental hypothermia is generally manifested as progression from an initial state of catecholamine release and stimulation (mild hypothermia) to one marked by a predictable slowing of metabolism and all critical body functions to the extent that patients may appear dead. The profound physiologic changes and metabolic slowing all reverse with rapid rewarming, and reports of remarkable neurologically intact survival despite hours of pulselessness and resuscitation are not infrequent. This has given rise to the adage “No one is dead until they are warm and dead.” Not surprisingly, there is little strong scientific evidence for treatment recommendations because trials cannot be conducted. The medical literature is composed mostly of animal experiments, case reports and series, and retrospective reviews. Still, rational approaches can be inferred from the extant literature for this uncommon but serious problem (Table 131.1).
Table 131.1 Definitions of Hypothermia
| LEVEL OF HYPOTHERMIA | CORE TEMPERATURE (° C) |
|---|---|
| General | >35 |
| Mild | 32-35 |
| Moderate | 28-32 |
| Severe | <28 |
Hypothermia
Pathophysiology
Mechanisms of Heat Loss
The mechanisms of heat loss are as follows:
• Radiation of heat occurs when the ambient temperature is less than body temperature and heat is lost directly to the environment via electromagnetic radiation.
• Conduction is heat transfer from one (warmer) solid to another (cooler) when they are in contact.
• Convection is loss of heat from a surface to a (usually moving) gas or fluid, typically air or water. It can be considered an adjunct to conduction.
• Evaporation causes heat loss through the energy required to vaporize water (i.e., sweat).
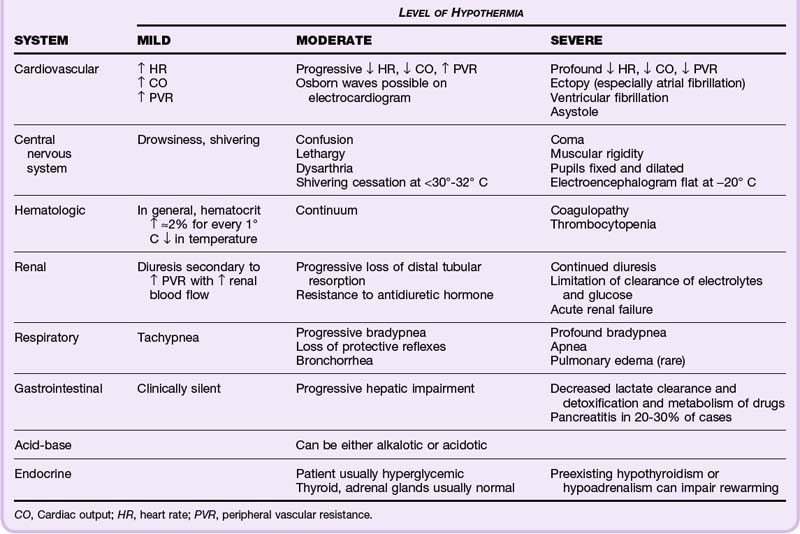
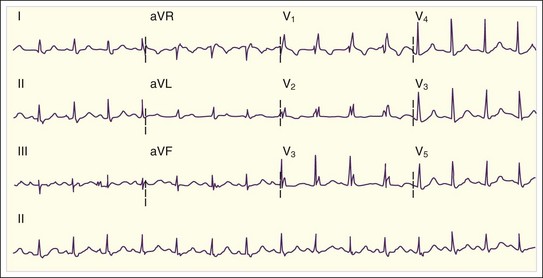
As a person cools, a fairly predictable procession of pathophysiologic changes occurs, as seen in Table 131.2 and Figure 131 .1.
Presenting Signs and Symptoms
The critical element of the diagnosis of hypothermia is accurate measurement of core temperature. Several methods exist, all of which have potential drawbacks (Table 131.3). Laboratory and physiologic changes are correlated with the temperature. For example, a normal hematocrit value in a severely hypothermic patient should prompt concern for hemorrhage because the hematocrit should rise in a predictable fashion with ever-lowering temperature. Alternatively, arterial blood gas values should be interpreted as though the patient is normothermic (the alpha-stat method) and not corrected for the actual core temperature (the pH-stat method). Evaluation for infection, metabolic derangement, and cardiac, neurologic, renal, and other organ system abnormalities is important because comorbid conditions are common as a cause, a consequence, or coincidence of hypothermia.
Table 131.3 Methods of Measuring Core Temperature
| METHOD | COMMENTS |
|---|---|
| Esophageal probe | Easy to insert |
| Falsely high temperature readings possible with warmed oxygen via an endotracheal tube | |
| Rectal probe | Insert to 15-20 cm |
| If the probe is in or surrounded by cold stool, temperature recordings will lag behind true changes | |
| Temperature-recording Foley catheter | Inflowing cold urine may falsely lower temperature recordings |
| Pulmonary artery catheter | Most accurate and most invasive method |
| Higher potential for iatrogenic injury, especially ventricular fibrillation in cold, irritable myocardium |