2. Severe features of preeclampsia include BP ≥160/100 mm Hg on two occasions at least 4 hours apart; thrombocytopenia (platelet count <100,000 per μL); impaired liver function; severe persistent right upper quadrant or epigastric pain; progressive renal insufficiency (serum creatinine >1.1 mg per dL or a doubling of serum creatinine in the absence of other renal disease); pulmonary edema; new onset cerebral or visual disturbances. Another change is the removal of intrauterine growth restriction as a feature of severe preeclampsia because it is a very common finding.
3. HELLP syndrome is often considered a subtype of severe preeclampsia, although it may be a related but unique condition. Alanine aminotransferase (ALT) and aspartate aminotransferase (AST) may be significantly elevated in this disorder. The platelet count is generally <100,000 per mm3. BP may be normal (15% of cases) in the HELLP syndrome, which will occasionally delay the diagnosis. Management and treatment are the same as for preeclampsia with severe features.
4. Eclampsia is the onset of seizure activity not attributable to another cause in a pregnant woman. Any seizure in a pregnant patient with hypertension after the 20th week of gestation should be assumed to be eclampsia until proved otherwise. Seizures may occur as late as 2 weeks’ postpartum.4 Headaches and visual disturbances are common prodromal symptoms before the onset of seizures.
D. Chronic hypertension with superimposed preeclampsia. This is the manifestation of preeclampsia in patients with chronic hypertension regardless of the cause.
1. Patients with chronic hypertension are at increased risk for the development of preeclampsia. It is vital that the pregnant patient with chronic hypertension seek early prenatal care, and even preconception counselling, when possible. Early assessment of renal function is key to diagnosis and monitoring of patients with superimposed preeclampsia.
2. Comorbidities that may exist with hypertension include connective tissue disorders, such as systemic lupus erythematosus and scleroderma, and severe renal disease, such as acute or chronic glomerulonephritis.
3. Preexisting renal disease in the setting of chronic hypertension may make the diagnosis of superimposed preeclampsia difficult, if not impossible. Following trends in proteinuria of a 24-hour timed specimen may be the only means to make this diagnosis.
CLINICAL PEARLThe differential diagnosis of hypertension during pregnancy includes gestational hypertension, chronic hypertension, preeclampsia, and chronic hypertension with superimposed preeclampsia.
II.Epidemiology
Preeclampsia and gestational hypertension are primarily disorders of older nulliparous women. Because assisted reproductive technology allows the older patient to achieve a successful pregnancy who may also have other comorbidities such as hypertension and diabetes, the incidence of these disorders will continue to rise.
A. Incidence. Preeclampsia affects 6% to 8% of all pregnancies, of which 25% have preeclampsia with severe features.5
1. HELLP syndrome occurs in 10% of women with preeclampsia with severe features.
2. The rate of preeclampsia in the United States is on the rise. For preeclampsia overall, the rate has increased from 3.4% in 1980 to 3.8% in 2010. The increase in preeclampsia with severe features accounts for the overall increase. In 1980, severe preeclampsia accounted for 0.3% of the cases compared to 1.4% in 2010.5
B. Maternal mortality. Preeclampsia and its sequelae, one of the three leading causes of maternal mortality, account for more than 25% of all cases of maternal mortality in the United States. Most of the deaths related to preeclampsia are due to pulmonary complications (e.g., pulmonary edema) and intracranial hemorrhage.
C. Neonatal mortality. Preeclampsia with severe features is a major contributor to neonatal morbidity and mortality, due to impaired uteroplacental perfusion, placental abruption, and iatrogenic prematurity due to onset of preeclampsia remote from term.
III. Risk factors (see Table 22.2)

A. Positive predictors. There are multiple risk factors for the development of preeclampsia. Preeclampsia frequently occurs during the first pregnancy and in those with a family history of preeclampsia. Advanced maternal age (older than 35 years) is now also recognized as an independent risk factor. Young age and low socioeconomic status may not play as great a role as previously thought.6
B. Protective factors. Cigarette smoking has been reported to be a protective factor against the development of preeclampsia, perhaps due to reduced secretion of soluble fms-like tyrosine kinase-1 (sFlt-1), a major mediator of preeclampsia.7
IV.Etiology
The true etiology of preeclampsia remains unknown. However, vascular endothelial injury is a consistent finding and leads to the clinical manifestations of preeclampsia.
A. Decreased placental perfusion. Owing to trophoblastic invasion, uterine spiral arteries vasodilate in a normal pregnancy to accept the increases in blood flow during late pregnancy. In preeclampsia, these changes do not occur. This abnormal angiogenesis results in superficial placentation that later in pregnancy causes release of soluble fms-like tyrosine kinase-1 (sFlt-1) and soluble endoglin (sEng), both placentally derived antiangiogenic factors. Increased levels of sFlt-1 and sEng reduce the placental release of vascular endothelial growth factor (VEGF) and placental growth factor (PlGF) both required for normal angiogenesis. Without VEGF and PlGF, placental ischemia and endothelial dysfunction occur and leads to the signs and symptoms of preeclampsia.8
B. Outcome of placental ischemia. Placental ischemia triggers the maternal systemic endothelial alterations that result in proteinuria, hypertension, and occasionally liver dysfunction.
C. Inflammatory mediators. Inflammatory mediators such as prostaglandins, interleukins, and endothelins, all of which have vasoactive properties, may trigger endothelial cell activation and dysfunction. An abnormal response to nitric oxide has been proposed as a factor in the development of preeclampsia.
D. Oxidative stress. Oxidative stress that results in membrane damage and lipid peroxidation due to free radical formation has been described as a potential mediator of endothelial cell dysfunction and activation in preeclampsia.
E. Vasoactive substances. Abnormal responses to vasoactive substances such as norepinephrine and angiotensin II may also play a role in the pathogenesis of preeclampsia. For example, a normotensive pregnant patient is usually refractory to the effects of an infusion of norepinephrine or angiotensin II. However, the preeclamptic patient with preeclampsia lacks this refractoriness.9
F. Antioxidants. Dietary deficiencies of antioxidants such as β-carotene and vitamin E have been reported in preeclampsia. There was initial enthusiasm for dietary supplementation of these antioxidants for prevention of preeclampsia. However, large randomized, placebo-controlled trials conducted during pregnancy found that supplementation with vitamins C and E did not reduce the risk of preeclampsia or improve maternal or fetal outcome.
G. Lifestyle modifications. Obesity due to dietary excess is still one of the most important risk factors in the development of preeclampsia. Protein and calorie restriction for obese pregnant women does not reduce the risk of preeclampsia or gestational hypertension and may increase the risk of intrauterine growth restriction and should be avoided.3 Exercise for prevention of preeclampsia has been investigated. Moderate exercise has been hypothesized to stimulate placental angiogenesis and improve maternal endothelial dysfunction. Small clinical trials have been unable to make any conclusions about the efficacy of moderate exercise in improving endothelial dysfunction. Large randomized trials are necessary.3
H. Genetic influences. Genetic influences have been reported in preeclampsia. Polymorphisms in the genes controlling the expression of inflammatory mediators such as interleukins have been described.10
I. Prostaglandin imbalance. A consistent finding in preeclampsia is a predominance of thromboxane, relative to prostacyclin, perhaps related to the endothelial injury.
1. Thromboxane is associated with vasoconstriction, platelet aggregation, decreased uterine blood flow, and increased uterine activity. Prostacyclin is associated with the opposite effects.
2. Aspirin, which inhibits the production of thromboxane, has been proposed as a means of preventing the development or decreasing the severity of preeclampsia. Although the routine use of this agent in all pregnant women does not appear to be indicated, there is a possibility that aspirin (81 mg daily) may be useful in women at high risk of developing early onset severe disease.11,12
V.Pathophysiology. The pathophysiology of preeclampsia can involve every maternal organ system, as well as the fetus (see Table 22.3).
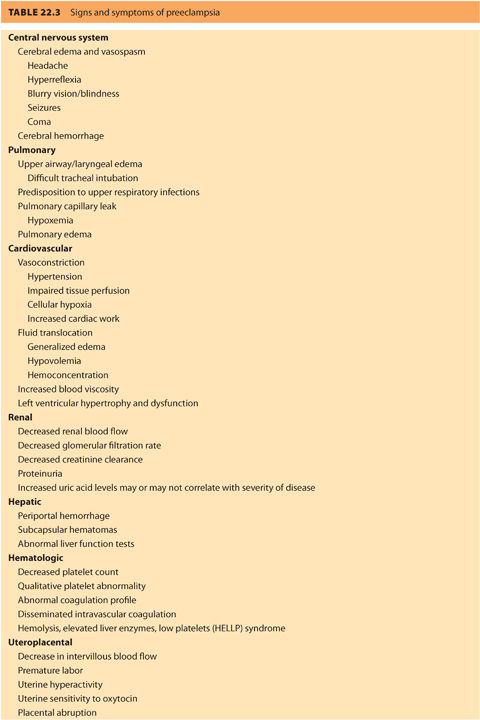
A. Central nervous system
In normal patients, cerebral perfusion is autoregulated within a mean arterial pressure of 50 to 160 mm Hg. One study has described abnormal autoregulation of cerebral blood flow in patients with preeclampsia.13 Clinical manifestations include hyperreflexia, headaches, visual changes including cortical blindness, and seizures. Headache is a marker for end-organ involvement and is a criterion for the diagnosis of preeclampsia with severe features. Severe retro-orbital headache is considered a premonitory symptom for eclampsia.13
1. A hyperdynamic and hyperperfused state has been described in the cerebral circulation of patients with preeclampsia, similar to patients with hypertensive encephalopathy. This is particularly true in patients with headaches as a manifestation of their preeclampsia. These findings have been documented by magnetic resonance imaging (MRI) studies.14
2. Generalized cerebral edema, which frequently presents in imaging studies of the brain, is a poor prognostic sign and may precede herniation of the brainstem through the foramen magnum.
3. Postmortem brain findings in patients with preeclampsia include edema, hyperemia, thrombosis, and bleeding ranging from petechiae to large cerebral hemorrhages. Intracranial hemorrhage, particularly subarachnoid hemorrhage, is a common cause of maternal mortality.
4. Electroencephalogram (EEG) findings are usually nonspecific in patients with preeclampsia.
5. Imaging studies of the brain may demonstrate areas of infarction that will often resolve spontaneously on serial examination but may persist in some women even after delivery.
B. Cardiovascular system
Preeclampsia is a dynamic disease process with hemodynamic changes characterized by increased vascular tone and increased sensitivity to vasoconstrictors occurring during the course of the disease and its treatment. Many of these changes are associated with endothelial cell dysfunction as described previously.
1. Studies reporting the use of invasive hemodynamic monitoring have had conflicting results, in large part because of the range of responses and the difficulty of interpreting data from patients who were treated with vasodilators or anticonvulsants.15
2. Preload is generally decreased due to a relative depletion of intravascular volume (third spacing effects). Preload may be augmented with intravenous (IV) administration of crystalloid or colloid solutions.
3. A hyperdynamic response to volume expansion may occur in the patient with preeclampsia.16 This is probably related to the increased release of atrial natriuretic peptide (ANP) compared to normal controls.17 Cardiac output may rise to three to four times that of baseline when blood volume is expanded.
4. Afterload is almost universally increased two- to threefold above baseline values. The increase in afterload is primarily responsible for the increase in BP seen in preeclampsia. With increases in afterload, the left ventricle may fail.
5. Volume contraction increases the sensitivity of the patient with preeclampsia to blood loss. Hemoconcentration leads to an elevated hematocrit.
C. Respiratory system
1. Increased airway edema as a result of third spacing can lead to difficult tracheal intubation. This also predisposes the patient with preeclampsia to mucosal injury and profuse hemorrhage during airway instrumentation.
2. Pulmonary edema (affects 3% of all preeclamptic women) may occur on a noncardiogenic basis due to endothelial capillary leakage.
D.Coagulation system
1. Platelets are affected by preeclampsia. The abnormality can be both quantitative and qualitative. Thrombocytopenia is the most common hematologic disorder in women with preeclampsia. A decrease in the platelet count is generally the first index of coagulation to become abnormal but it is below 100,000 in fewer than 10% of patients with severe features. Because platelets adhere to the damaged arterial walls, platelets release thromboxane and other factors resulting in platelet activation.18
2. Signs and symptoms of disseminated intravascular coagulation (DIC), such as a low fibrinogen and prolonged prothrombin time (PT) and partial thromboplastin time (PTT), rarely occur until the platelet count falls below 100,000 per mm3.19 Unless the platelet count is <100,000, or there is a precipitous decrease in platelet count within a short time period (i.e., 1 to 2 hours) and/or there are signs of clinical bleeding (e.g., ecchymosis at BP sites), a full coagulation profile is unnecessary before neuraxial anesthesia placement.
3. In HELLP syndrome, prolonged PT/PTT should be anticipated and a full coagulation profile obtained for all patients.
E. Genitourinary/renal system
1. Proteinuria is a hallmark of preeclampsia and is an indicator of renal dysfunction. It is a product of endothelial cell damage and a “leaky” capillary state.
2. Normally, glomerular filtration rate (GFR) dramatically increases during pregnancy. Women with preeclampsia have diminished GFR, and renal function will worsen as the process becomes severe. This can lead to renal insufficiency and oliguria.
3. Elevated blood uric acid levels were once considered a predictor of decreased renal function; however, the uric acid level is not a good monitor of onset or offset of preeclampsia. Elevated uric acid levels correspond to decreased GFR or may indicate increased tubular reabsorption.20 The blood urea nitrogen (BUN) level also rises in patients with preeclampsia.
4. Acute tubular necrosis is rare, but may occur in the severely volume constricted patient and in the face of severe blood loss and inadequate volume replacement.
F. Hepatobiliary system
1. Hepatic changes associated with preeclampsia may range from a mild elevation in liver function tests to a syndrome similar to acute fatty liver of pregnancy. Hepatic rupture has been reported but is fortunately rare.
2. Large subcapsular hematomas have been reported in patients with severe preeclampsia and are often manifested by right upper quadrant pain. These can usually be managed without surgical intervention, but severe subcapsular hemorrhage/hematoma can cause intraperitoneal hemorrhage. This requires emergency laparotomy and if unrecognized can result in maternal death. Early treatment by interventional radiologists using stents is very successful in limiting the morbidity associated with subcapsular hematomas and, indeed, may be lifesaving.
G. Fetus and placenta
1. Preeclamptic women have decreased uteroplacental perfusion, leading to fetal growth restriction and oligohydramnios. Because uteroplacental blood flow is proportionate to BP, hypotension during neuraxial analgesia/anesthesia must be avoided.
CLINICAL PEARLEvery organ system is affected by preeclampsia and the anesthesiologist must pay particular attention to the cardiac, respiratory, and coagulation systems. Additionally, airway edema can make tracheal intubation difficult.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







