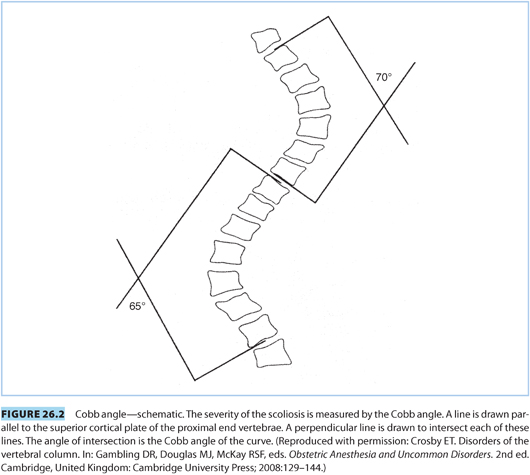
(1) The Cobb angle measures the degree of spinal curvature (see Fig. 26.2). Minor curves (10 to 20 degrees) occur in approximately 2% of adolescents in the United States. These are benign and require no therapy. Curves <40 degrees rarely require fusion, but thoracic curves >65 degrees will require fusion and, if untreated, can result in a restrictive respiratory pattern limiting ventilatory reserve.1
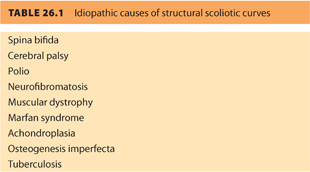
(2) Nonstructural curves are the result of leg length discrepancies or posture. The spine remains mobile and the curve is not progressive. Structural curves are more commonly idiopathic and can result from a variety of conditions (see Table 26.1).
b. Surgical correction involves decortication of the vertebrae with fusion and instrumentation. During fusion and instrumentation, the spinal muscles are dissected away from the curved vertebrae. Once exposed, the spinous processes and interspinous ligaments are removed to allow “straightening” of the curve. The vertebrae are then decorticated and subsequently fused.
2. Obstetric management
a. Mild curves are not affected by pregnancy. Parturients with corrected or mild scoliosis tolerate pregnancy and delivery well and require no special considerations. Patients with curves >25 degrees that have not been stabilized may experience clinical deterioration due to the mechanical and hormonal effects of pregnancy (see Table 26.2).
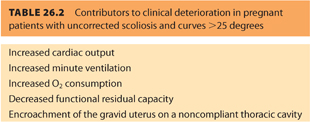
b. In patients with severe disease, all of these can contribute to deterioration of cardiopulmonary function. In addition, those patients with severe disease or preexisting cardiopulmonary compromise may not tolerate the physiologic changes of advanced labor.
c. Patients with kyphoscoliosis of the lumbar spine may also have funnel-shaped distortion of the pelvis. These deformities often result in abnormal fetal presentations. Indications for cesarean delivery (CD) are outlined below.2
(1) Maternal decompensation
(2) Pelvic abnormalities
(3) Malpresentation
(4) Inadequate labor
3. Anesthetic considerations
a. Antepartum care
(1) Pathophysiology. Preanesthetic evaluation should be obtained in patients who have undergone corrective surgery or have a Cobb angle >30 degrees. The anesthesiologist should determine if there are associated disorders (e.g., spina bifida, Marfan syndrome) as well as determine the extent of cardiopulmonary disease. Because scoliosis can interfere with formation, growth, and development of the lungs, especially in patients with disease occurring before age 8, the number of alveoli will be reduced. The pulmonary vasculature develops in parallel to alveolar formation. If these processes are interrupted, increased pulmonary vascular resistance can produce pulmonary hypertension and right-sided heart failure.
(2) Respiratory function. Mechanical function can also be impaired by vertebral and rib cage abnormalities. The most common pulmonary function abnormality is a restrictive pattern. This occurs in patients with curves >65 degrees. In these patients, the functional residual capacity (FRC) is also reduced, causing airway closure during normal tidal breathing. The most common blood gas abnormality is a reduced PaO2, normal PaCO2, and increased alveolar-to-arterial oxygen gradient. These findings result from venoarterial shunting and altered regional perfusion. Pulmonary function tests and blood gas analysis will be helpful in symptomatic patients to determine if the patient will tolerate the demands of labor and delivery.
(3) Other neuromuscular disorders and scoliosis. In addition to the skeletal deformity, patients with scoliosis resulting from neuromuscular disorders can also suffer from respiratory compromise produced by abnormalities of central control of respiration and supraspinal innervation of respiratory muscles. These patients may be at risk for aspiration pneumonitis resulting from compromised protective airway reflexes.
(4) Preanesthetic consultation. A preanesthetic consultation gives the anesthesiologist an opportunity to review prepregnancy radiographs as well as operative records. In cases where such radiographs are unavailable, it is desirable to obtain a radiograph at term to identify the extent and location of instrumentation. A preanesthetic consultation also allows for discussion of the advantages and disadvantages of neuraxial anesthesia before the patient experiences pain. The natural history of scoliosis is for back pain to increase over time. Although there is a lack of evidence suggesting that neuraxial anesthetic techniques worsen back pain in this population, it is important for this to be part of the discussion. In those who have undergone instrumentation, it is helpful to detail the caudal extent of instrumentation. In approximately 20% of patients, the instrumentation extends to a level of L4–L5. Patients with evidence of cardiopulmonary disease may require subspecialty referrals for optimization and delivery planning.
b. Intrapartum management
Patients with scoliosis, particularly those who have undergone instrumentation, are at increased risk for difficult epidural placement and complications (see Table 26.3).3
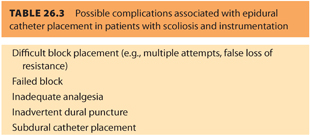
(1) Inadequate block. Inadequate or unsatisfactory block can be expected in up to 50% of patients with instrumentation. However, recent advances in instrumentation may lessen the incidence of poor-quality block.
(2) Anatomic considerations. Some practitioners consider corrective spinal surgery a relative contraindication to neuraxial anesthesia. However, in many patients, a neuraxial catheter may be inserted below the level of instrumentation and preferably in the least affected part of the spine. Ultrasound may be helpful in identifying the caudal extent of instrumentation.4 Patients with a Cobb angle >40 degrees will also have a vertebral deformity resulting in vertebral bodies that are shorter with thinner pedicles and laminae. This deformity causes a narrower vertebral column on the concave side.
(3) Technical considerations. The rotational component of scoliosis frequently requires placement of a laterally directed needle (i.e., from the palpable spinous process toward the convexity of the curve) (see Fig. 26.3).5 The actual angle varies with the degree of curvature and is best determined by identification of the ligaments during advancement of the needle. Also, the degree of lateral deviation is determined by the severity of the curvature. Consider a bevel direction of the epidural needle parallel to the long axis of the back (i.e., parallel to the dural fibers) to reduce the risk of headache in the event of dural puncture.6 Indeed, due to the increased incidence of “spotty” or “patchy” blocks, intentional dural puncture and use of a continuous spinal may be considered, particularly in patients at increased risk for CD.7,8 Other possible analgesic modalities include (i) intraspinal opioids, (ii) caudal analgesia, (iii) intravenous (IV), and (iv) patient-controlled analgesia (PCA). If dural puncture has occurred and the patient develops a postdural puncture headache (PDPH), Gerancher et al.9 report the successful placement of a caudal blood patch in a patient with Harrington rod instrumentation. However, most obstetric anesthesiologists are not experienced in the caudal approach so care should be exercised if considering this option.
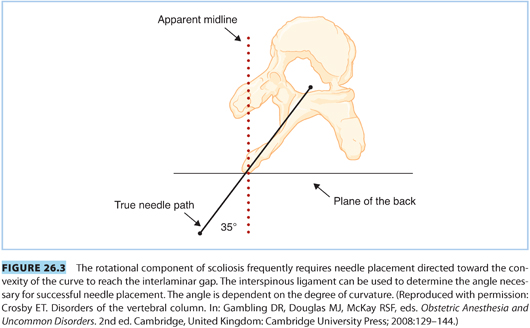
CLINICAL PEARLThe rotational component of scoliosis frequently requires placement of the needle lateral to the apparent midline and directed toward the convexity of the curve.
(4) Anesthesia for cesarean delivery. For CD, neuraxial techniques are preferred. However, in some patients positioning may be difficult and neuraxial placement is impossible or the technique fails. In addition, patients with severe disease may not tolerate supine positioning. In such cases, general anesthesia will be necessary to ensure airway control and adequate ventilation. Invasive monitoring is rarely indicated in patients with scoliosis, but in cases where there is severe respiratory compromise and evidence of impending respiratory failure, an arterial line will be helpful for assessing ventilatory management in the operating room as well as postoperatively.
B. Spinal surgery
1. Clinical issues
Corrective surgery for scoliosis, including instrumentation, represents the most common spinal surgery in patients presenting for obstetric care (see preceding text). Because of early detection and intervention, the number of patients with uncorrected curves is reduced from previous decades, limiting the number of patients with cardiopulmonary complications. Occasionally, patients will present having sustained trauma or after laminectomy or other procedures for herniated discs.
2. Obstetric management
Obstetric management is rarely affected, except that these patients will occasionally have continuing back pain that requires chronic opioid therapy. In these cases, the care team should be reminded of the risk of withdrawal symptoms and that such patients will benefit from early anesthetic consultation to assist in managing chronic opioid doses as well as adding agonist–antagonist opioid agents during the peripartum period.
3. Anesthetic management
Several published studies and case reports describe epidural or continuous spinal analgesia/anesthesia for labor and delivery in women with spinal instrumentation. There is no contraindication and no long-term sequelae from neuraxial techniques. The risks of neuraxial block are listed in Table 26.3. These risks are substantially lower for those patients who have undergone only discectomy or simple fusion.10 Neuraxial blocks should be placed above or below the level of the surgery, and conservative dosing should be used, recognizing that the smaller epidural space may require less local anesthetic. A continuous spinal catheter may improve success,8 although current equipment in the United States results in an unacceptable rate of PDPH.
CLINICAL PEARLThe risks and benefits of neuraxial block must be discussed, particularly the natural progression of chronic back pain that is likely unaltered by the neuraxial anesthetic.
C. Spinal cord injury
The annual incidence of SCI is 4.5 per 100,000 population in the United States.11 More than half of these occur in the cervical region.12 Improvements in acute care and rehabilitation have enabled more women with SCI to become pregnant. Both the level of injury and its duration impact the care of these patients.
1. Clinical issues
a. Duration of injury
(1) Acute phase
During the initial spinal shock phase, the patient suffers flaccid motor paralysis, areflexia, and sympathetic denervation below the level of the lesion. This results in vasodilation that can compromise both temperature regulation and hemodynamic stability to a degree commensurate with the level of the lesion. If the lesion is above T1, there may be relative bradycardia due to unopposed parasympathetic innervation. Lower systemic vascular resistance results in venous pooling, decreased venous return, and hypotension. In fact, anything that results in vagal stimulation (e.g., Valsalva, tracheal suctioning) may cause profound bradycardia, which may require external or chemical pacing with a direct-acting catecholamine agonist. During this phase, respiratory complications are common due to paralysis of the intercostal muscles, poor cough, and decreased respiratory reserve. These complications are further compounded during pregnancy by upward displacement of the diaphragm by the gravid uterus and “thoracic” breathing.
(2) Chronic phase
After a period of several weeks, a chronic state of paralysis, muscle spasticity, and disuse atrophy ensues. In addition, cardiovascular reflexes attempt to compensate for the loss of sympathetic tone with variable success. During this period, orthostatic hypotension is common. Meanwhile, some of the motor reflex activity returns, often pathologically. The mass motor reflex occurs when a stimulus that normally causes contraction of a small number of fibers, produces widespread spasm. Thermoregulation is also impaired in these patients. Other related problems include (i) anemia, (ii) chronic urinary tract infections, and (iii) decubitus ulcers.
b. Level of injury
(1) Women with cord injuries below S2 have involvement of bladder, bowel, and sexual function.
(2) Women with lesions above T10 will not experience labor pain and, although they are not at particular risk for preterm labor, they may not present until labor is advanced.
(3) Above T6, patients are at risk for autonomic hyperreflexia (see subsequent text) and respiratory compromise. Estimates suggest that more than two-thirds of parturients with a lesion above T6 will develop autonomic hyperreflexia in response to distension of the uterus, bladder, or rectum.
(4) When lesions are above T1, patients lose sympathetic innervation to the heart, compromising the reflexive response to hypotension.
c. Other complications
Additional medical complications can include respiratory compromise, from lesions above T5, due to a loss of FRC. With the addition of pregnancy, patients have an increased likelihood of respiratory failure. Impaired thermoregulation due to vasodilation, impaired sweating, and autonomic hyperreflexia are also possible. Urinary tract infections occur at a much higher rate as well.
d. Autonomic hyperreflexia
This potentially life-threatening complication results from lack of central inhibition of the sympathetic neurons present in the spinal cord below the level of injury. Painful visceral or cutaneous stimuli (e.g., uterine contractions or bladder distension) below the level of the spinal cord lesion stimulate sympathetic afferents in the sympathetic chain. Although inhibitory neurons in the intact individual limit the spread of this impulse, patients with SCI respond with an impulse that propagates up and down the sympathetic chain, resulting in massive sympathetic stimulation and vasoconstriction. With lesions below T6, compensatory vasodilation in the intact portion of the cardiovascular system prevents critical hypertension. If the lesion is above T6, there is insufficient innervated vasculature to adequately compensate. This results in profound hypertension.
CLINICAL PEARLSCI above a T6 level warrants neuraxial anesthesia to prevent autonomic hyperreflexia; close hemodynamic monitoring is required.
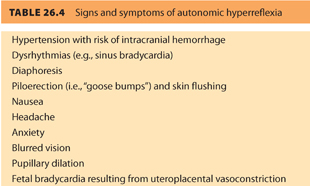
(1) Signs and symptoms of autonomic hyperreflexia (see Table 26.4)
(2) Prevention/treatment
(a) Prevention is paramount. Early administration of combined spinal-epidural (CSE), or epidural analgesia with local anesthetics and opioids can prevent autonomic hyperreflexia caused by uterine contractions. Neuraxial analgesia prevents the reflex by interrupting noxious sensory input from the viscera. A Foley catheter should be placed to prevent bladder distension.
(b) Treatment of a hypertensive emergency includes removal of the offending stimulus, if possible (e.g., consider bladder catheterization), and administration of IV nitroprusside, sublingual nitroglycerin, and/or phentolamine.
a. Traumatic SCI occurring during pregnancy may result in spontaneous abortion or preterm delivery. For the first several months after injury, the patient is at increased risk for deep vein thrombosis (DVT) and pulmonary embolism. Prophylaxis against these complications may impact plans for neuraxial anesthesia. Guidelines for administration of neuraxial anesthesia in patients receiving anticoagulants can be found at http://www.asra.com.
b. Patients with SCI who have lesions above T10 will have painless labor and are at risk for preterm labor and delivery. Before term, they are monitored closely to prevent home delivery. Because of inadequate expulsive efforts in the second stage, assisted delivery may be necessary.
c. Antepartum consultation in a high-risk obstetric anesthesia clinic, with delivery at a tertiary care center that includes appropriate anesthesia coverage, is recommended.
d. For those at risk for autonomic hyperreflexia, antihypertensive medications should be available at the bedside and labor analgesia should be instituted early. Autonomic hyperreflexia can also confound the diagnosis of preeclampsia.
e. Temperature should be measured at regular intervals because hyperthermia (in the absence of infection) can occur as a result of altered thermoregulation.
f. Patient position should be changed regularly to prevent decubitus ulcer formation.
g. The American College of Obstetricians and Gynecologists (ACOG) concluded in their 2002 Committee Opinion: Obstetric management of patients with spinal cord injuries, that obstetricians should be aware of the specific problems related to SCIs. Autonomic dysreflexia is the most significant medical complication seen in women with SCIs and precautions should be taken to avoid stimuli that can lead to this potentially fatal syndrome. Women with SCIs may give birth vaginally, but when CD is indicated, adequate anesthesia (spinal or epidural, if possible) is needed.15
3. Anesthetic management
a. Neuraxial analgesia is the most common approach for the prevention and treatment of autonomic hyperreflexia. Although either CSE or epidural analgesia is a good choice, CSE may be preferable for its rapid onset. Labor analgesia differs in these patients by (i) need for initiation very early in labor, (ii) a typical test dose that will not identify unintentional subarachnoid catheter placement, and (iii) difficult assessment of level of analgesia. If neuraxial block placement is impossible, other measures for treating autonomic hyperreflexia should be at the bedside (e.g., nitroglycerin, nitroprusside).
b. Sensory levels can only be reliably assessed if the level of block is more cephalad than the spinal cord lesion. However, a limited assessment can be made by stroking the abdomen above and below the umbilicus. If there is contraction of the abdominal muscles, the level of sensory block is below that level because sensory blockade will abolish this reflex.
c. Placement of an arterial catheter may be indicated to allow beat-to-beat monitoring of blood pressure (BP) because many of these patients have low baseline BP and are prone to hemodynamic instability. Pulse oximetry may also be prudent.
d. For CD, spinal anesthesia is preferable because it provides better protection from autonomic hyperreflexia compared to epidural anesthesia.13 If neuraxial anesthesia is technically impossible, or if the level of cord injury produces respiratory embarrassment when supine, general anesthesia will be necessary. During the period of denervation (i.e., 24 hours to 1 year after injury), succinylcholine should not be administered due to the risk of hyperkalemic cardiac arrest, due to the potential for massive potassium release from postsynaptic and extrajunctional receptors. However, some have suggested that succinylcholine should always be avoided in these patients, and that nondepolarizing muscle relaxants should be used to facilitate laryngoscopy and intubation, if necessary.16
D. Spina bifida
Spina bifida results from failure of the vertebrae to fuse completely around the neural tube contents. There are two major categories:
1. Spina bifida occulta describes failed fusion of the arch without herniation of the meninges or spinal cord. Failure at a single level (usually L5 or S1) is common and occurs in up to one-third of the population. It is considered to be a normal variant by some.17 There is a wide range of presentations, from asymptomatic radiographic findings to chronic back pain with posterior disc herniation and minor neurologic problems. In patients who have superficial stigmata (e.g., tuft of hair or lipoma), there is an increased likelihood of an underlying occult spinal dysraphism (i.e., cord abnormality). Most of these are asymptomatic but there may be a higher risk for disc herniation.
a. Obstetric management is uncomplicated in patients with spina bifida occulta.
b. Anesthetic management
(1) Most patients carrying this diagnosis present little concern, but preanesthetic assessment should include examination of the back with clear documentation of neurologic status.18 The patient should also be informed that analgesia could be incomplete during delivery because the epidural space may not be continuous across the defect. There is an increased risk of dural puncture because of abnormal lamina and ligamentum flavum formation, especially when placement is attempted at the site of the lesion. This risk can be reduced by inserting the needle in a position remote from the level of the lesion. Most neuraxial anesthetics are uncomplicated because the level of the lesion is typically below most neuraxial needle placements (i.e., L5–S1). In addition, most are midline defects of the lamina that rarely interfere with needle placement.
(2) Presence of neurologic deficits or cutaneous manifestations should concern the anesthesiologist, particularly for the risk of tethered cord.19 Tethered cord results from attachment of the spinal cord to an area of the lumbar spine. Reports suggest that the incidence of tethered cord in cases of spinal bifida occulta is low, but nearly all patients with spina bifida cystica and meningomyelocele have tethering. If there are neurologic deficits or cutaneous manifestations, radiographs, preferably existing ones, should be obtained.
(3) In a patient with tethered cord who declined neuraxial analgesia, fentanyl IV PCA with an adjunct infusion of dexmedetomidine (an α2-agonist with negligible placental transfer) provided adequate analgesia without respiratory depression.20
2. Spina bifida cystica (or aperta) includes meningocele (i.e., failed closure of the neural arch with herniation of the meninges) and myelomeningocele (i.e., herniation of both meninges and neural elements through a vertebral defect). These cases are much less common (<5 per 1,000 births). Prenatal folate supplementation has further reduced the incidence by as much as 50%.21 Improved surgical and medical care has increased the likelihood that affected women will present for obstetric interventions. Numerous anomalies may coexist including Chiari II malformation (i.e., downward displacement of the medulla, fourth ventricle, and cerebellum into the cervical spinal canal), hydrocephalus with shunt placement, and tethered cord. Many of these patients develop progressive spinal deformities, including kyphoscoliosis.
a. Obstetric management
Recurrent urinary tract infections are the most common complication, resulting in preterm labor. Patients with severe kyphoscoliosis may experience respiratory compromise due to the expanding uterus. CD is reserved for obstetric indications (e.g., inadequate pelvic dimensions).
b. Anesthetic management
(1) Preanesthesia consultation. Preanesthetic consultation helps determine anesthetic options. The anesthesiologist should determine the level of the lesion and whether the patient has residual neurologic function. Most patients with these disorders have undergone imaging studies to determine the spinal abnormalities. These will facilitate anesthetic assessment.
(2) Technical concerns. Parturients with lesions above T10 are unlikely to experience labor pain, but those with higher lesions are at risk for autonomic hyperreflexia (see Section C. Spinal Cord Injury). Because neuraxial anesthesia is not contraindicated in these patients,17 such techniques should be utilized whenever possible to prevent autonomic hyperreflexia and to avoid the risk of general anesthesia. However, attempts at identifying the epidural space can result in dural puncture due to incomplete formation of the ligamentum flavum. If epidural placement is successful, one must consider that the epidural anesthetic may be inadequate due to discontinuity of the epidural space. In patients with negligible function below the lesion, concerns for cord damage are reduced and continuous spinal anesthesia should be considered.
(3) Other considerations. If a patient has a ventricular shunt, its function should be assessed. Symptoms of shunt malfunction or infection include headache, fever, drowsiness, and convulsions. Patients with severe kyphoscoliosis may also require pulmonary function testing. Patients with spina bifida who lack bladder control often self-catheterize and are at increased risk (approximately 25%) for latex sensitivity.22
CLINICAL PEARLPatients with spina bifida are at increased risk for latex sensitivity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








