Ultrasound-guided regional anesthesia (transversus abdominis plane block)
Intracranial pressure measurement (optic nerve sheath diameter)
KEYPOINTS | |
1.Applications of point of care ultrasound are rapidly expanding in obstetric management. 2.Focused cardiac ultrasound can be used as a powerful extension of the physical examination to evaluate a variety of clinical conditions including hypotension, dyspnea, and cardiac arrest. 3.Pulmonary ultrasound can serve as a rapid and more sensitive measure of lung water and pneumothorax than radiography, which can be used to guide management. 4.Ultrasound-guided neuraxial blockade may improve efficiency of block placement and has applications for training. 5.Gastric ultrasound can be used to qualitatively assess gastric volume and content, which may inform timing of decisions for nonelective obstetric procedures. | |
I.Introduction
A. The application of ultrasound technology is rapidly changing the practice of medicine in providing a safe, noninvasive tool to aid in diagnosis, guide therapy, and assist with procedures.
B. Reduced costs and increased portability have led to increased point of care applications of ultrasound.
C. Ultrasound has a long track record of safe use including in the first trimester of pregnancy.1
D. The two principal skills required for point of care ultrasound are image acquisition and interpretation. There is general agreement that point of care ultrasound is valuable for qualitative assessment for the purpose of rapidly narrowing differential diagnoses. There is more debate about the appropriateness of quantitative assessment in the domain of point of care ultrasound.
E. Ultrasound measurements have generally been demonstrated to be accurate and reproducible.2 Point of care ultrasound is often performed in less than ideal conditions (dynamic clinical environment, patient movement, less training, and oversight) that may compromise some quantitative validity.
F. With expansion of the use of ultrasound, there are challenges in providing training to a broader group of users while ensuring adequate quality of application.
G. Elements of a quality point of care ultrasound program include using a structured approach to examination, documenting findings in the medical record, storing images and videos, and maintaining a quality assurance process.3
H. Most ultrasound machines have standard features to adjust gain, scan depth, freeze images, and conduct basic measurements. Additional available features include time-motion imaging (M-mode), color Doppler, and cardiac calculations.
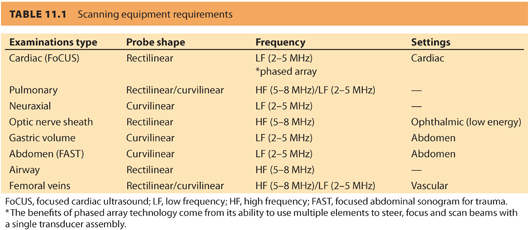
I. In selecting ultrasound probes, it is important to understand the relationship between frequency and image granularity/depth of penetration. Deeper structures (>6 cm depth, e.g., abdomen and chest) require low frequency ultrasound (2 to 5 MHz); however, some imaging quality is sacrificed. Superficial structures (<6 cm depth, e.g., pleura, peripheral nerves) can be imaged with higher frequency ultrasound (5 to 8 MHz), resulting in sharp imaging.4 Choose an ultrasound probe based on intended structures to be imaged (see Table 11.1).
II. Focused cardiac ultrasound
A. Introduction
1. Hemodynamic monitoring of the parturient, particularly those with comorbidities or who are critically ill, is evolving rapidly.
2. Changes in available technology, as well as perceptions of complications and limited benefits with regard to outcomes using invasive monitoring,5 have led to the growth of ultrasound technology for hemodynamic monitoring.6
3. Cardiac ultrasonography as a diagnostic tool is particularly well-suited to the pregnant woman.
a. Women are generally comfortable with ultrasound examinations of their fetus throughout pregnancy.
b. The maternal anatomic changes of pregnancy are also favorable for cardiac ultrasound, with the gravid uterus displacing the heart cephalad and laterally, bringing the heart closer to the chest wall.
c. Parturients are often optimally positioned in left uterine displacement or left lateral position, facilitating parasternal and apical views.
d. Additionally, parturients are usually conscious and mobile, making invasive monitoring less desirable.
4. Focused cardiac ultrasound (FoCUS) refers to the use of ultrasound as an adjunct to physical examination to answer specific clinical questions.7
5. FoCUS is unique among hemodynamic monitoring modalities available to the clinician at bedside in providing comprehensive anatomic and physiologic information that can be obtained in real time and repeated to observe changes in hemodynamics and responses to therapy.
6. FoCUS methodology involves point of care image acquisition and interpretation by a physician with specific training, in contrast to comprehensive echocardiography examination in which image acquisition is obtained by an ultrasonographer (i.e., technician) and interpretation performed by an echocardiographer (i.e., specialist physician).
7. FoCUS combines image acquisition and interpretation skills at the bedside, albeit with more limited expertise in both domains. Anesthesiologists are particularly well suited to adopt this technology given prevalent ultrasound skills in the domains of vascular access and peripheral nerve blockade as well as the cardiac image acquisition and interpretation skills used for transesophageal echocardiography.
CLINICAL PEARLFoCUS provides real-time comprehensive anatomic and physiologic information. It can be repeated to observe changes in hemodynamics and responses to therapy.
B. Techniques
1. Basic FoCUS examination views. FoCUS incorporates examination views commonly used in comprehensive transthoracic echocardiography (TTE). Each of these views provides different challenges and diagnostic advantages in the parturient (see Fig. 11.1).
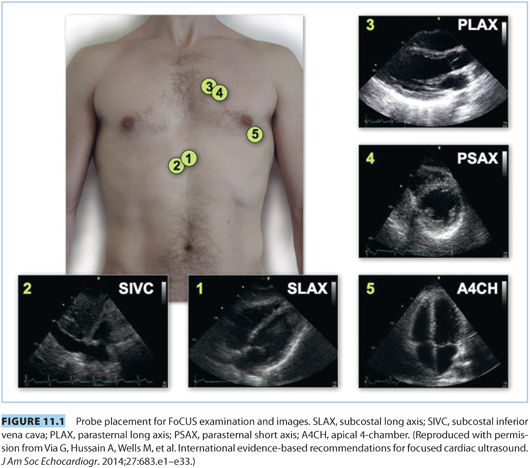
a. Subcostal long axis (SLAX)
b. Subcostal inferior vena cava (SIVC)
c. Parasternal long axis (PLAX)
d. Parasternal short axis (PSAX)
e. Apical 4-chamber (A4CH)
2. Intravascular volume
a. Intravascular volume assessment is a core application of FoCUS.
b. Left ventricular end-diastolic diameter and/or area can easily be measured and compared using the basic FoCUS views, including PSAX, PLAX, and A4CH to demonstrate cardiac filling volumes or preload.
c. Normal values for left ventricular end-diastolic diameter have been reported in pregnancy (3.0 to 5.6 cm).8
d. The SIVC view has also been shown to approximate intravascular volume status.
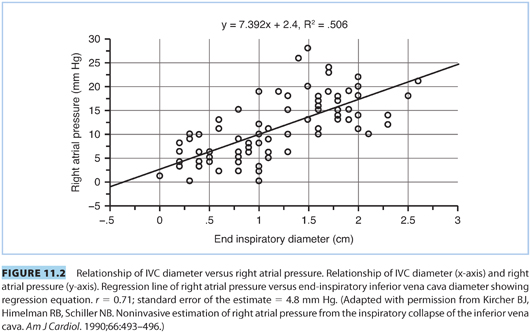
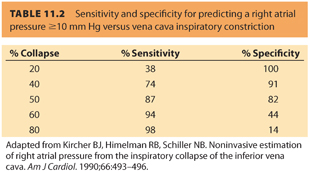
e. Qualitatively, hypovolemia is associated with a progressive narrowing of the IVC diameter and ultimately collapse of >50% during inspiration with spontaneous ventilation (see Fig. 11.2 and Table 11.2).
f. Obtaining the SIVC view can be challenging at term due to uterine fundal height. This approach may be more reliable in the postpartum setting.
g. Regardless of the selected approach, the ability to rapidly estimate volume status in the acute management of a variety of clinical situations can be very valuable in directing care.
h. Qualitative assessment of high or low intracardiac volumes can guide the clinician in fluid management, transfusion, or diuresis, whereas serial examinations can serve to assess the response to treatment.
i. Estimations of right ventricular volume can be conducted qualitatively using any cardiac view.
j. The A4CH provides the best perspective to compare right and left ventricular size side by side.
k. In pathologic situations (acute embolism, pulmonary hypertension, right heart failure), left and right ventricle chamber sizes may equalize, the cardiac apex may become shared, and the normal left to right interventricular septal bowing may flatten.
CLINICAL PEARLFoCUS can be used to rapidly estimate volume status in the acute management of a variety of clinical situations and be very valuable in directing care.
3. Contractility
a. Biventricular systolic function can be determined qualitatively using any cardiac view, but the parasternal views are the most accessible in the pregnant patient.
b. Using the PSAX view, contractility of the concentric left ventricle can be qualitatively assessed rapidly.
c. The PLAX provides another option for assessing contractility including opportunities for more quantitative measurements using ejection fraction calculations.
4. FoCUS protocols
a. A systematic approach to the FoCUS examination has been advocated to increase its accuracy and improve its diagnostic capability.3
b. Several specific protocols and algorithms have been developed for the peripartum patient, although no individual protocol has been demonstrated to be diagnostically superior or associated with improved clinical outcomes.
c. Two commonly referenced protocols are the FoCUS assessed transthoracic echocardiography (FATE)9 and rapid obstetric screening echocardiography (ROSE).10
d. FATE was originally developed for critical care application but has been adapted to a wide range of clinical situations.9
e. The FATE examination includes the following steps: (1) rule out obvious pathology, (2) assess wall thickness and dimension of cardiac chamber, (3) assess contractility, (4) assess pleura, and (5) relate these findings to the clinical situation.9,11
f. Four basic views are utilized for FATE: SLAX, A4CH, PSAX, and PLSX, with a basic pleural examination, making FATE relatively simple and easy to learn.9,11
g. The ROSE scan was the first published FoCUS protocol adapted to pregnant women.
h. The ROSE protocol incorporates qualitative and quantitative evaluations using PSAX, PLAX, A4CH, and A5CH views. The apical 5-chamber view (not shown in Fig. 11.1) is a more anterior 4-chamber scan that includes the left ventricular outflow tract.
i. The ROSE protocol also includes more advanced quantitative elements of echocardiography such as cardiac output, ventricular regional wall motion, valve interrogation, and diastolic function that have been deemed outside of the scope of basic FoCUS.3
C. Clinical applications
1. Hypotension
a. Unexplained hypotension is common in obstetric anesthetic practice, and diagnosis can be difficult considering the prevalence of both neuraxial anesthesia and hemorrhage.
b. In other clinical domains, the use of FoCUS has been shown to rapidly narrow broad differential diagnoses12 and reduce inappropriate therapy (e.g., fluid administration in congestive heart failure [CHF])13 in patients who are hypotensive.
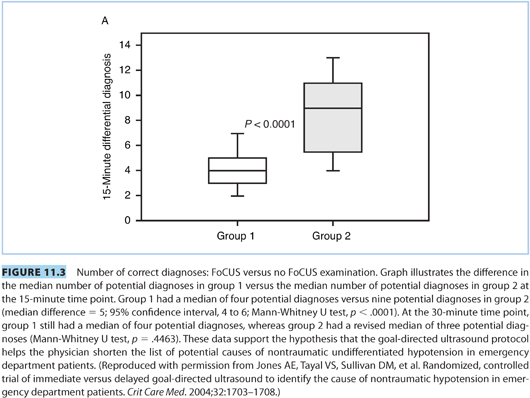
c. One study of 184 patients presenting with nontraumatic, undifferentiated hypotension were randomized to receive early versus delayed “goal-directed cardiac ultrasound” (i.e., FoCUS). Physicians who utilized FoCUS were able to significantly narrow their differential diagnoses (see Fig. 11.3) and were also more likely to choose the correct final diagnosis as “most likely” on the differential list.12
d. In another randomized controlled trial, 240 hypotensive or tachycardic individuals were randomized to receive either FoCUS in their primary trauma survey or standard initial management (no FoCUS examination) in the emergency department.13 They demonstrated reduced intravenous fluid administration, shorter interval to the operating room, and increased intensive care unit (ICU) admission rate (80% vs. 67%, P = 0.04) in the group that incorporated FoCUS into management.
e. In the parturient, the differential diagnosis for hypotension is broad, ranging from hemorrhage to aortocaval compression to embolic events. The unique hemodynamics of the peripartum period also result in an increased risk of rarer cardiovascular diseases such as cardiomyopathy, myocardial infarction, and aortic dissection.8
CLINICAL PEARLIn some clinical domains, the use of FoCUS has been shown to rapidly narrow broad differential diagnoses and reduce inappropriate therapy (e.g., fluid administration in CHF) in patients who are hypotensive.
2. Dyspnea
a. Symptoms of shortness of breath, tachypnea, oxygen desaturation, or auscultative findings, alone or in combination, are common in pregnancy or immediately postpartum. FoCUS, preferably in combination with lung ultrasound, may assist diagnosis and management.
b. FoCUS has been recommended as a first-line diagnostic intervention for the pregnant patient with shortness of breath or pulmonary edema.14
c. Differentiating pulmonary from cardiogenic pathology may be of particular value. Qualitative, side-by-side evaluation of left- and right-sided cardiac systolic function and filling volumes in this setting is useful to rule out some diagnoses related to volume overload or cardiac failure or diminish the likelihood of others such as embolism.
CLINICAL PEARLFoCUS has been recommended as a first-line diagnostic intervention for the pregnant patient with shortness of breath or pulmonary edema.
3. Chest pain
a. There may be a limited role for FoCUS in the setting of chest pain in pregnancy. As an adjunct to physical examination, FoCUS can provide a rapid screening tool to identify some rare, life-threatening causes such as myocardial ischemia or infarction, pleural or pericardial effusions, right ventricular strain associated with pulmonary embolism, or aortic dissection.15
b. Comprehensive echocardiography is an American Society of Echocardiography class I recommendation to evaluate chest pain when electrocardiograms (the diagnostic gold standard) are inconclusive.16 However, assessment of segmental wall motion abnormalities is an advanced echocardiographic skill and probably falls outside the scope of FoCUS.3
CLINICAL PEARLEchocardiography is recommended to evaluate chest pain when electrocardiograms (the diagnostic gold standard) are inconclusive.
4. Cardiac arrest
a. Cardiac arrest in pregnancy occurs at a rate of approximately 1 in 12,000 admissions,17 with the most common etiologies being hemorrhage, heart failure, embolism, and sepsis.
b. FoCUS offers potential diagnostic and therapeutic advantages in managing some of these conditions.
c. There is also evidence suggesting that FoCUS may aid resuscitation management post-arrest in nonpregnant patients by detecting potentially reversible mechanical causes of cardiac arrest (e.g., profound hypovolemia, embolism, tension pneumothorax, or tamponade) as well as confirming cardiac standstill.
d. The subcostal 4-chamber view can be initiated during advanced cardiac life support (ACLS) chest compressions, with higher quality images acquired during brief pauses to confirm pulses.
e. The use of FoCUS during cardiac arrest changes management, is more accurate than physical examination or electrocardiography in determining mechanical cardiac function, and may facilitate better outcomes; however, its use has not yet been shown to actually improve outcomes.3
CLINICAL PEARL The use of FoCUS during cardiac arrest changes management, is more accurate than physical examination or electrocardiography in determining mechanical cardiac function, and may facilitate better outcomes; however, its use has not yet been shown to actually improve outcomes.
5. Preeclampsia and other potential future applications of FoCUS
a. The use of FoCUS in obstetrics is still in a development phase. Published reports have followed a pattern of proof of feasibility,10 case reports of applications that redirected care,8 and observational trials in high-risk patients such as those with preeclampsia.18
b. The greatest opportunity in obstetrics and other domains where FoCUS is being employed will be to link applications to improved clinical outcomes.
c. Preeclampsia is an area with promise for potential application of FoCUS. Hypertensive disorders of pregnancy are important causes of maternal and fetal morbidity and mortality affecting up to 10% of pregnancies worldwide.19 The incidence has increased by up to 30% over the past decade20 due to advanced maternal age, increased use of alternative reproductive techniques, along with prepregnancy comorbidities such as obesity, diabetes, metabolic syndrome, and chronic hypertension.21
d. The majority of maternal deaths from hypertensive disorders are thought to be preventable,22 and multidisciplinary groups have called for coordinated efforts to improve outcomes.23
e. Reported hemodynamic observations have been conflicting in women with preeclampsia, likely due to the heterogeneity in the disease itself, as well as varied research study designs, patient characteristics, and presence or absence of therapeutic interventions.
f. Due to the heterogeneity of observed cardiovascular dynamics of preeclampsia, the role of FoCUS in this population may be best suited for early screening and serial examination throughout the peripartum period.
g. Pulmonary edema, a major cause of ICU admission and death in preeclampsia,24 could perhaps be reduced with careful monitoring using FoCUS and timely therapeutic interventions.
h. Diastolic dysfunction along with low colloid osmotic pressure and increased intravascular hydrostatic pressure are likely etiologies for pulmonary edema in preeclampsia.24
i. Although pushing the boundaries of the scope of FoCUS, risk-stratifying patients by presence of diastolic dysfunction may redirect management in high-risk patients.
j. An important additional part of this evaluation includes the use of pulmonary ultrasound to determine the presence and degree of lung water (see “Dyspnea” section). By employing this relatively simple lung ultrasound technique in addition to FoCUS, clinicians can further tailor intra- or postpartum fluid management before the onset of acute hypoxia from pulmonary edema.25
D. FoCUS training, certification, and program maintenance
It is unclear what optimal FoCUS skills training encompasses, and this is an evolving field. The American Society of Echocardiography has outlined optimal elements of this training, which should include didactic training, hands-on imaging in humans, and image interpretation experience.7 Many practitioners are acquiring the skill set by taking one of the many established courses in combination with local mentoring and guided practice. The skill is likely best developed in an environment of multidisciplinary collaboration and an established quality assurance program. At the time of this publication, there is no board certification process for FoCUS.
CLINICAL PEARLThe majority of maternal deaths from hypertensive disorders are thought to be preventable, and multidisciplinary groups have called for coordinated efforts to improve outcomes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








