Chapter 73 Hypertension in the Pediatric Intensive Care Unit
When confronted with a child with abnormally “high” blood pressure (BP) in the medical setting, the pediatrician is immediately confronted with two vexing issues. One is whether this abnormality will lead to immediate organ- or life-threatening consequences, and the second is whether the potential intervention itself will result in a worse outcome. Systemic hypertension (HTN) is a major lifelong condition that begins in childhood and is one of the leading causes of premature death in developed countries and developing nations.1 The current obesity epidemic along with other lifestyle choices have likely led to the increasing numbers of children now being diagnosed with HTN.2 Current estimates suggest that up to 5% of children have HTN compared with estimates of approximately 1% just a decade ago, while another 10% to 25% have prehypertension.3–13 If untreated, HTN is associated with a 10-year survival rate of about 50% in adults depending on the degree of retinal changes and/or level of diastolic pressure.14,15
Definition of Terms
The most recent recommendations for diagnosing HTN in children were published in 2004 by the National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents (Task Force) and were designed to mirror recommendations for diagnosing HTN and pre-HTN in adults according to the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. However, unlike adult definitions that are based on the observations reported by Volhard and Fahr in 1914 as well as epidemiologic studies showing a clear risk for cardiovascular morbidity and mortality with BPs at a certain level, pediatric definitions are based on epidemiological thresholds generated from a population of more than 60,000 children and adolescents across the United States.16,17 Therefore in children systemic hypertension is defined as an average systolic BP (SBP) and/or diastolic BP (DBP) that is ≥95th percentile for gender, age, and height on three or more separate occasions16,18 (see Appendix at www.expertconsult.com). In addition, children with an average SBP and/or DBP that is at the 90th percentile or higher (or ≥120/80 mm/Hg when a patient’s 90th percentile exceeds this value) should be considered prehypertensive.16 This classification of prehypertension is not meant to be considered a definitive diagnosis such as with HTN. Rather, the goal of classifying children as prehypertensive is to identify those who may be at risk for developing HTN in the near future in the hopes that interventions may prevent its establishment. Note that these definitions refer to threshold BPs measured in a resting, nonstressed child; elevations in BP are commonly associated with a patient’s stress response, which will normalize when the stress is eliminated. Nevertheless, the health care community has performed poorly in managing patients who have already been diagnosed with HTN, and vigilance must be practiced across all age groups.19–21
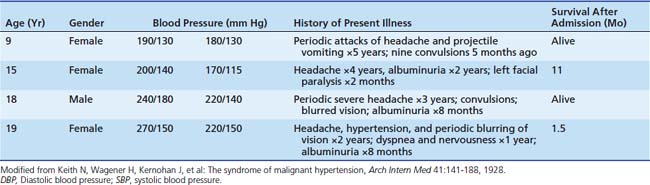
The clinical state of a “malignant sclerosis” or “bösartig hypertension” was first reported by Volhard and Fahr in 1914 in patients with mainly HTN and “hypernephrosclerosis.”17 In 1928, Keith et al: described 81 cases of what was termed “the malignant hypertension syndrome” that was a diagnosis made before end-stage damage of retinal, cerebral, cardiac or renal function occurred.22,23 It was also the first description of pediatric patients with significantly uncontrolled hypertension (Table 73-1). The term “hypertensive crisis or emergency” is defined as a rapid and elevated level of either systolic or diastolic BP that is associated with end-organ damage (Box 73-1).24–26 The terms “hypertensive crisis” and “hypertensive emergency” have been used interchangeably in the literature; “hypertensive emergency” is used in this chapter. Organs commonly affected include the central nervous system (CNS) (hypertensive encephalopathy, retinal vasculopathy-induced visual changes, cerebral infarction, and hemorrhage); the cardiovascular system (congestive heart failure, myocardial ischemia, aortic dissection); and the kidneys (proteinuria, hematuria, and acute renal insufficiency). The term “hypertensive urgency” is reserved for the condition where end-organ damage has not yet occurred despite an increase in BP.25,26 Historically, a patient with a hypertensive urgency could be managed with oral medications and the BP corrected over a 24-hour period.27 In contrast, a patient with a hypertensive emergency requires parenteral therapy and continuous BP monitoring.27
Etiology and Evaluation
Hypertension may be either primary (essential) or secondary to another underlying medical condition. While primary HTN is unusual in the PICU, its frequency is increasing with the current epidemic of obesity, although hypertensive urgency and emergency are almost always secondary to another condition.16 Children with primary HTN are frequently overweight and have positive family histories for HTN and cardiovascular disease. The prevalence of HTN increases progressively with a rise in body mass index, with approximately 30% of overweight children (body mass index >95th percentile) exhibiting hypertension.28 Being overweight and hypertensive are signs of the insulin-resistance syndrome or metabolic syndrome, a condition associated with multiple metabolic risk factors for cardiovascular disease as well as type 2 diabetes.29
Secondary causes of HTN can be both transient and sustained. The most common reasons for elevated BP in a critical care unit are inadequately treated pain and agitation. Without a high degree of suspicion, this can be difficult to detect, particularly if neuromuscular blockade is administered. Tachycardia as well as eye tearing with noxious interventions are two useful clues to this condition. Drug-induced HTN is also common in the critical care setting, especially when high-dose corticosteroids are used in patients with organ transplantation and other immunologic conditions. A number of other drugs associated with elevated BP are listed in Box 73-2. A review of all medications taken by the patient, as well as considering illicit drug use, is indicated for all patients with an elevated BP. A patient’s fluid balance for several days also should be reviewed when HTN develops while in the ICU. Apparently innocuous discrepancies between input and output for a single day can cumulatively produce significant fluid overload after several days, although this alone is not typically enough to cause HTN in the absence of other renal, cardiovascular, or CNS problems that raise systemic vascular resistance (SVR), cardiac output (CO), or both. Finally, postoperative HTN is common in the ICU setting, occurring in up to 75% of patients. Initially, factors such as hypoxia, hypercarbia (through its sympathomimetic effects), and pain should be promptly and adequately addressed.30 Afterward, pharmacotherapy is indicated if HTN is refractory or sustained despite adequate ventilation, sedation, and analgesia.
Box 73–2 Causes of Hypertension in Children
Box 73-2 shows a list of other potential causes of transient and sustained HTN in children. Evaluation should be targeted at both identifying the etiology as well as any potential signs of injury to the cardiovascular, neurologic, renal, or ocular systems. A detailed history and thorough examination should be obtained for all patients, with special care paid to findings suggestive of an underlying hypertensive disorder or end-organ damage (Table 73-2). Signs and symptoms are often reflective of the severity and rapidity of onset of HTN. Chronic HTN is more commonly asymptomatic or characterized by low-grade generalized symptoms such as fatigue and recurrent headaches. Neurologic symptoms, however, are the most common presenting complaints in children with hypertensive emergency; congestive heart failure and renal insufficiency also are reported.16 Hypertensive encephalopathy typically manifests as a severe headache with dizziness and changes in mental status ultimately culminating as seizures; other reported symptoms include facial palsies and visual changes that may lead to blindness and coma.31–33 An abrupt presentation of chest or back pain along with HTN should trigger the consideration of aortic dissection.34 Rarely, children can present with abdominal pain or vomiting as the only symptoms of a hypertensive emergency.35
Table 73–2 History and Physical Examination Findings in HTN
| Finding | Possible Significance |
|---|---|
| HISTORICAL FINDINGS | |
| Complaint/Review of Systems | |
| Headaches, dizziness, epistaxis, visual changes | Nonspecific with respect to etiology of HTN |
| Abdominal/flank pain with hematuria | Renal artery or vein thrombosis |
| Hematuria, swelling, decreased urine output | Acute glomerulonephritis |
| Dysuria, frequency, urgency, nocturia, enuresis | Underlying renal disease |
| Joint pains/swelling, edema, rashes | Autoimmune mediated disease/glomerulonephritis |
| Weight loss, sweating, flushing, palpitations | Pheochromocytoma or hyperthyroidism |
| Muscle cramps, weakness, constipation | Hypokalemia associated with hyperaldosteronism |
| Delayed puberty | Congenital adrenal hyperplasia |
| Snoring | Sleep apnea |
| Prescription, over-the-counter, or illicit drug use | Drug-induced HTN |
| Medical History | |
| Umbilical artery catheterization | Renal artery thrombosis/renal embolus |
| Previous urinary tract infections | Renal scarring |
| Thyroid cancer, neurofibromatosis, von-Hippel Lindau disease | Pheochromocytoma |
| Family History | |
| HTN | Inherited forms of hypertension (AME, Gordon syndrome, Liddle syndrome, GRA), essential HTN |
| Renal disease | Polycystic kidney disease, Alport syndrome |
| Tumors | Familial pheochromocytoma, multiple endocrine neoplasia type II |
| PHYSICAL EXAMINATION FINDINGS | |
| Vital Signs | |
| Tachycardia | Hyperthyroidism, pheochromocytoma, neuroblastoma, primary HTN |
| Bradycardia | Increased intracranial pressure (tumor, hydrocephalus) |
| Drop in blood pressure from upper to lower extremities | Coarctation of aorta |
| General | |
| Growth retardation | Chronic kidney disease |
| Truncal obesity | Cushing disease, insulin resistance |
| Head and Neck | |
| Moon facies | Cushing disease |
| Elfin facies | Williams syndrome |
| Proptosis/goiter | Hyperthyroidism |
| Web neck | Turner syndrome |
| Adenotonsillar hypertrophy | Sleep disorders |
| Fundal changes | Chronic or severe HTN |
| Cardiovascular | |
| Friction rub | Systemic lupus erythematosus, collagen vascular disease, uremia |
| Apical heave | Left ventricular hypertrophy |
| Disparity in pulses | Coarctation |
| Lungs | |
| Crackles/rales | Heart failure |
| Abdomen | |
| Masses | Obstructive nephropathy, Wilms tumor, neuroblastoma, pheochromocytoma, polycystic kidney disease |
| Hepatomegaly | Heart failure |
| Bruit | Renal artery stenosis, abdominal coarctation |
| Genitalia | |
| Ambiguous, viralized | Congenital adrenal hyperplasia |
| Extremities | |
| Edema | Underlying kidney disease |
| Joint swelling | Autoimmune disease |
| Rickettsial changes | Chronic kidney disease |
| Dermatologic | |
| Neurofibromas | Neurofibromatosis |
| Tubers, ash leaf spots, adenoma sebaceum | Tuberous sclerosis |
| Bronzed skin | Excessive adrenocorticotropic hormone |
| Acanthosis nigricans | Insulin resistance/metabolic syndrome |
| Striae, acne | Cushing disease |
| Rashes | Vasculitis/nephritis |
| Needle tracks | Drug-induced HTN |
| Neurologic | |
| Mental status changes | Severe HTN |
| Cranial nerve palsy | Severe HTN |
AME, Apparent mineralocorticoid excess; GRA, glucocorticold-remediable aldosteronism.
Initial laboratory studies for all patients should include electrolytes, blood urea nitrogen, creatinine, complete blood cell count with peripheral smear, and urinalysis. Renal disease is the most common cause of secondary HTN in children, and both chronic and acute renal conditions may present with severe HTN. Anemia associated with chronic disease or a microangiopathic anemia resulting from disseminated activation of the coagulation system or hemolytic uremic syndrome may be seen as well. Finally, a hypokalemic metabolic alkalosis may develop with volume depletion and secondary hyperaldosteronism. This condition also may be seen in children with inherited monogenic forms of HTN.36
Renal ultrasonography is indicated for most patients to evaluate for renal parenchymal lesions such as small scarred kidneys, polycystic kidney disease, or other structural anomalies. Doppler evaluation of blood flow to the kidneys also should be performed, although this evaluation is less sensitive than in adults at identifying subtle renal artery stenosis in smaller children. Although both computed tomography (CT) and magnetic resonance angiography have shown some promise as a screening tool for renal artery stenosis, angiography remains the gold standard for identifying this lesion.37–39 Further imaging such as a dimethylsuccinic acid (DMSA) scan may be indicated in children who are suspected of having renal scarring; plasma renin and aldosterone levels also may help discern the etiology of HTN, although typically they are not rapidly available.
A chest radiograph and electrocardiogram should be done at presentation to look for signs of heart failure and electrocardiographic evidence of ventricular hypertrophy, strain, or both. An echocardiogram is now recommended for all children with HTN to assess for congenital anomalies such as a coarctation of the aorta as well as for left ventricular hypertrophy, a common finding in children with long-standing HTN that correlates with blood pressure severity.40–42 An echocardiogram may not need to be performed emergently if the child has no other signs of heart failure.
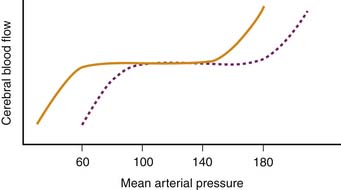
A head CT scan should be done in patients with concern for increased ICP. In children with cerebral edema or increased ICP, increased BP may develop as a strategy to preserve cerebral perfusion due to the increased resistance to cerebral blood flow. Initially, a child with traumatic brain injury will often maintain sufficient cerebral blood flow over a range of BPs because of the brain’s capacity for autoregulation, as depicted in Figure 73-1.43 However, if the resistance to cerebral blood flow increases, such as when ICP rises from swelling, then the patient may compensate through cerebral vasodilation or increased CO to meet the metabolic needs of the brain. Cerebral vasodilation, however, will only increase ICP further. To attempt to maintain adequate cerebral blood flow, the perfusion pressure must increase as noted in the following mathematical relationship: Cerebral perfusion pressure = Mean arterial pressure (MAP) − ICP. In such situations, it is prudent to undertake measures to control brain edema through hyperosmolar therapy, judicious sedation/analgesia, and minimizing the noxiousness of laryngoscopy while securing the airway to control oxygenation and ventilation. Efforts to directly lower systemic BP can undermine the patient’s ability to support injured but viable cerebral tissue.
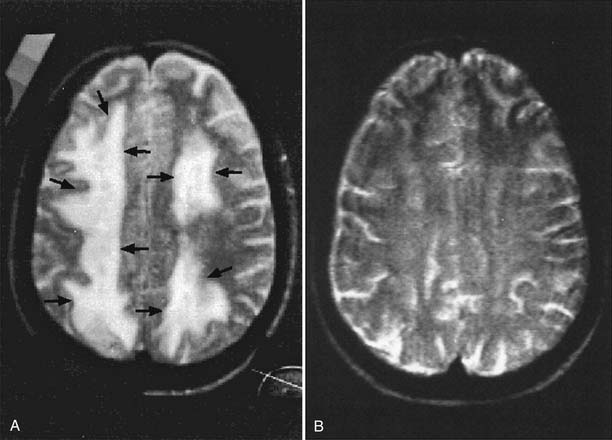
A magnetic resonance image also may be considered for patients with other neurologic symptoms. The most common brain-associated finding in children with a hypertensive emergency is posterior reversible encephalopathy syndrome (PRES). PRES is a syndrome characterized by the sudden onset of HTN, headaches, altered mental status, seizures, visual loss, and even cortical blindness.156 Neuroimaging studies during PRES typically demonstrate cerebral edema affecting the white matter in a parieto-occipital distribution.157 PRES is associated with immunosuppressive therapy (especially cyclosporine and tacrolimus), acute glomerulonephritis, eclampsia of pregnancy, and hypertensive encephalopathy (Figure 73-2).44 Hypertensive emergencies and tonic-clonic seizures were presenting features in 59% of renal transplant patients who were found to have PRES on further work-up.45 In addition, nearly half of the patients with PRES had no history of uncontrolled chronic HTN.45 This constellation of symptoms and pathology, which has also been called reversible posterior leukoencephalopathy by other authors,46 typically resolves once the HTN is treated, but it may take weeks to months for the imaging abnormalities to normalize.45
Pregnancy associated with preeclampsia also must be considered in patients experiencing a hypertensive emergency. Preeclampsia is a state of hypertensive proteinuria in a pregnant woman who is at greater than 20 weeks’ gestation.47 Clinically, the classic triad of preeclampsia consists of HTN, proteinuria, and edema, although now it is accepted that edema should no longer be considered a prerequisite for making the diagnosis of preeclampsia.47 Under these circumstances, an elevated BP separated by a minimum of 4 hours (maximum 7 days) is considered adequate for making a diagnosis for HTN (>140/90 mm Hg) or severe HTN (>160/100 mm Hg). Proteinuria is considered significant when two random urine samples collected at least 4 hours (but <7 days) apart have a level of 30 mg/dL or higher (1+) or 300 mg or more of protein are present in a 24-hour urine collection.47 In the absence of proteinuria, pregnancy-induced HTN, gestational HTN, or chronic HTN must be considered. The goal of managing preeclampsia is to meticulously control the blood pressure in order to protect the fetus from insufficient placenta-utero blood flow (via overly aggressive antihypertensive therapy) and to avoid eclampsia (the condition characterized by tonic-clonic seizure activity culminating in coma).
Pathophysiology
A hypertensive emergency can occur in patients with essential HTN, secondary HTN, or without any history of HTN.24 The mechanisms responsible for generating and maintaining a hypertensive crisis continue to be elucidated. What seems plausible is that there is a triggering event that precipitates a dramatic increase in BP over a short period in a patient who is hypertensive at baseline. This event then leads to further arteriolar damage that prolongs the hypertensive state. The foundation for understanding this process can be drawn from knowledge regarding the existence of arteriolar damage caused by the mechanical stresses of long-standing HTN.48 In the presence of systemic HTN, endothelial cell damage occurs, encouraging platelet activation, aggregation, and fibrin deposition followed by intravascular hemolysis.48 Over time, the arterioles exhibit fibrinoid necrosis with fine subendothelial lipid inclusions and hyaline thrombi formation with little evidence of an inflammatory infiltrate.49
Endothelial Homeostasis
Endothelial health plays a central role in the HTN continuum. The endothelium is on the receiving end of the excessive pressures and shear stress generated from high blood flows along with concomitant increased resistance imparted by the vascular architectural scaffolding and surrounding smooth muscle cells. Aside from structural trauma, endothelial cell function is also affected. For instance, the stressed endothelial cell increases intracellular levels of nuclear factor-κB (NF-κB).50 In turn, NF-κB results in expression of vascular cell adhesion molecule-1 that binds to monocytes and T-lymphocytes (facilitating invasion through the vascular wall that normally does not occur) and contributes to the inflammatory state.50,51 The proinflammatory mediators interleukin-1β and tumor necrosis factor-α also induce vascular cell adhesion molecule-1 expression in endothelial cells through the NF-κB pathway.50 In addition to vasoconstrictor mediators, the coagulation system also has been implicated in the HTN story; injured endothelial cells locally activate the coagulation cascade and promote platelet aggregation that leads to a prothrombotic surface.24,50,52,53
Adults with essential HTN who experienced a hypertensive emergency demonstrated a significant decline in BP when given L-arginine (a precursor of nitric oxide [NO]) compared with patients who also had essential HTN but had not experienced a hypertensive emergency event. This observation underscores the importance of the endothelium in the pathogenesis of a hypertensive emergency because an intact functional endothelial cell surface is necessary to respond to L-arginine.54 Von Willebrand factor (a surface marker of endothelium), P-selectin (platelet activation), and fibrinogen serum levels were all increased in hypertensive adult patients with a hypertensive emergency compared with control subjects with HTN, suggesting that alterations in the homeostasis of the endothelial and/or the coagulation system occur during a hypertensive emergency.55
< div class='tao-gold-member'>