164 Hyperglycemia and Blood Glucose Control
 Altered Glucose Regulation in Stress
Altered Glucose Regulation in Stress
At the end of the 19th century, Claude Bernard described the link between acute trauma and the development of hyperglycemia irrespective of underlying diabetes. It was considered to be an adaptive stress response ensuring adequate glucose supply to the obligatory glucose-consuming neurons, phagocytes, and reparative cells.1,2 Stress-induced hyperglycemia is evoked by integrated hormonal, cytokine, and nervous “counter-regulatory” signals on glucose metabolic pathways. Essentially, the hyperglycemia is due to insulin resistance in the liver and skeletal muscle. Hepatic insulin resistance leads to increased hepatic gluconeogenesis and glucose output.3 Decreased glycogen synthesis and a shift from insulin-dependent to non–insulin-dependent glucose uptake characterize skeletal muscle insulin resistance.4
In the acute phase of critical illness, it is assumed that increased levels of glucagon, cortisol, and growth hormone jointly increase hepatic gluconeogenesis. In addition, the catecholamines epinephrine and norepinephrine, released in response to acute injury, promote hepatic glycogenolysis. The cytokines interleukin (IL)-1, IL-6, and tumor necrosis factor (TNF) may directly or indirectly enhance both of these hyperglycemic responses.5
The important exercise-stimulated glucose uptake in skeletal muscle totally disappears because of the immobilization of the critically ill patient. Insulin-dependent glucose uptake is hampered also through a combined inhibition of glucose transporter-4 (GLUT-4) and glycogen synthase activity.6,7 Although some studies have shown decreased glucose oxidation8 through pyruvate produced by glycolysis, others have demonstrated an opposite effect during critical illness.9 The decrease in insulin-dependent glucose uptake in skeletal muscle is completely offset by a strong increase in total body glucose uptake, of which the mononuclear phagocyte system in liver, spleen, and ileum are the main receivers.10 However, in skeletal muscle, non–insulin-dependent glucose uptake is also increased by increased expression of GLUT-1.11,12 The overall increased peripheral glucose uptake13 in light of hyperglycemia underscores the pivotal role of increased hepatic glucose production during critical illness, which cannot be suppressed by exogenous glucose.14
The position of adipose tissue in the regulation of glucose metabolism during critical illness has been neglected. Nevertheless, in diabetes mellitus, adipose tissue strongly modulates insulin resistance, as it is regarded as an insulin-dependent glucose uptake organ. Recent studies have now revealed that during critical illness, adipose tissue undergoes major changes.15 Possibly stimulated by illness-induced macrophage infiltration, adipocytes become more numerous and smaller and have an increased expression of the non–insulin-dependent glucose transporters, GLUT-1 and GLUT-3. The levels of GLUT-4 remain unaltered. As such, adipose tissue seems reprogrammed during critical illness to facilitate glucose uptake independent of circulating insulin levels.
 Hyperglycemia in Critically Ill Patients
Hyperglycemia in Critically Ill Patients
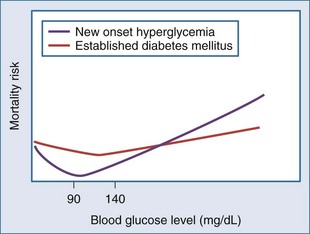
However, stress hyperglycemia is also associated with adverse outcome in several critically ill patient populations. More precisely, a large cohort study of over 66,000 critically ill patients revealed a J-curved relationship between on-admission blood glucose level and the risk of mortality, with the nadir between 100 and 150 mg/dL (5.6-8.3 mmol/L).16 In patients with an acute coronary syndrome, a similar association has been observed, with the lowest risk of mortality at blood glucose levels between 80 and 100 mg/dL (4.4-5.5 mmol/L).17–20 Importantly, in patients with established diabetes mellitus prior to critical illness or an acute coronary syndrome, the relationship between hyperglycemia and mortality is significantly blunted and somewhat shifted to the higher blood glucose17 (Figure 164-1).
Until recently, it was considered state of the art to tolerate blood glucose levels up to 220 mg/dL (12 mmol/L) in fed critically ill patients. It was even suggested that this moderate hyperglycemia in critically ill patients was beneficial for organs such as the brain and the blood cells which rely solely on glucose for their energy supply and do not require insulin for glucose uptake. Motivation for treatment of blood glucose levels higher than 12 mmol/L was primarily the occurrence of hyperglycemia-induced osmotic diuresis and fluid shifts. Also, from the diabetes literature it was known that uncontrolled and pronounced hyperglycemia predisposes to infectious complications.21 In patients with known diabetes mellitus, usually more attention was paid to blood glucose levels and consequently more strictly controlled. This approach contrasts—in hindsight—with the blunting of the J-shaped relation between glycemia and mortality risk. Observational studies have also revealed that hyperglycemia in patients with established diabetes mellitus gives an at least threefold higher risk of mortality compared to patients with known diabetes.22
 Maintenance of Normoglycemia in the Intensive Care Unit
Maintenance of Normoglycemia in the Intensive Care Unit
The Leuven Studies
In 2001, a large prospective, randomized, controlled trial (RCT) was the first to challenge the classic dogma of beneficial stress hyperglycemia.23 It examined the effect of tight glycemic control (TGC) with intensive insulin therapy on mortality and morbidity of critically ill patients. Over a 1-year period, 1548 mechanically ventilated patients admitted to the intensive care unit (ICU), predominantly after extensive or complicated surgery or trauma, were randomly allocated to either intensive insulin therapy with blood glucose levels kept tightly between 80 and 110 mg/dL (4.5-6.1 mmol/L) or the conventional approach, which recommended insulin therapy only if blood glucose levels exceeded 12 mmol/L. The intervention of TGC comprised accurate arterial blood glucose measurements by a blood gas analyzer and a reliable continuous infusion of insulin exclusively via a central venous line, using an accurate syringe-driven infusion pump. The fine insulin dose adaptations were performed by trained bedside nurses and based on a guideline which requires a high level of intuitive and anticipating decision making. In this study, patients were kept in a nonfasting state at all times. Dextrose 20% was administered on the first day (192 g glucose over 24 hours or 768 kcal/d). Thereafter, enteral nutrition was started, with the daily amount progressively increased as tolerated. When enteral nutrition was insufficient, early supplemental parenteral nutrition was given, resulting in administration on average of 1100 nonprotein kcal/d.
Intensive insulin therapy, resulting in the administration of on average 1100 nonprotein kcal/d, lowered ICU mortality from 8% to 4.6% (absolute risk reduction [ARR] 3.4%) and in-hospital mortality from 10.9% to 7.2% (ARR 3.7%). The effect occurred particularly in the population with prolonged critical illness, among whom mortality was reduced from 20.2% to 10.6%. Even patients in the conventional insulin treatment schedule with only moderate hyperglycemia (110-150 mg/dL) showed higher mortality compared with patients in the strict glycemic control schedule.24 Intensive insulin therapy also had a major effect on morbidity. It decreased the duration of ventilatory support and ICU stay, reduced the need for blood transfusions, and lowered the incidence of bloodstream infections and excessive inflammation. Even more striking, intensive insulin therapy caused a highly significant decrease in the development of critical illness polyneuropathy and acute kidney failure.
Subsequently, the effect of TGC was tested in a medical ICU setting by the same group.25 The difference in in-hospital mortality, 40.0% in the control group and 37.3% in the intervention group, was not statistically significant in an intention-to-treat analysis of the 1200 included patients. However, in patients who stayed in the ICU for 3 or more days, in-hospital mortality was reduced from 52.5% to 43.0% by TGC. Intensive insulin therapy also reduced morbidity (incidence of acute kidney failure, weaning of the ventilator, ICU/hospital stay) but not as strikingly as in the surgical study. This was in part explained by a larger fraction of patients in medical ICUs who were admitted with established organ damage, possibly reducing the opportunity of prevention by glucose lowering.26 The fact that intensive insulin therapy to normal-for-age blood glucose targets in mainly postoperative pediatric critically ill patients did reduce mortality by an ARR of 3% may further corroborate this finding.27
The Initial Repeat Studies
Two European multicenter studies designed to assess whether intensive insulin therapy exerts benefit, with mortality as the primary endpoint, failed to reproduce the Leuven findings. The VISEP (Volume substitution and Insulin therapy in severe SEPsis) (N = 537) trial was designed as a four-arm study to assess the difference between two choices of fluid resuscitation (10% pentastarch versus modified Ringer’s lactate) and the efficacy and safety of intensive insulin therapy in patients with severe sepsis and septic shock.28 In this study, blood glucose targets comparable to the Leuven studies were set out for the intervention (80-110 mg/L) and control (180-200 mg/dL) groups. Likewise, the insulin administration and blood glucose measurements had been standardized. Nevertheless, the insulin arm of the study was stopped early after 488 patients had been included, because the rate of hypoglycemia (12.1%) in the intensive insulin therapy group was considered unacceptably high and may be associated with higher mortality. Then at the first planned interim analysis, the fluid resuscitation arm of the study was also suspended because of increased risk of organ failure in the 10% pentastarch arm. The primary endpoint, 90-day mortality, was 39.7% in the intensive versus 35.4% in the conventional treatment arm.
The GLUCONTROL multicenter RCT (N=1101) investigated whether tight glycemic control (80 and 110 mg/dL) with intensive insulin therapy versus an intermediate target for blood glucose (140-180 mg/dL [7.8-10.0 mmol/L]) improves survival in a mixed population of critically ill patients.29 This study was also stopped early because the target glycemic control was not reached and the incidence of hypoglycemia was 9.8%. ICU mortality did not differ between the intensive insulin therapy group (17.2%) and the control group (15.3%).
Two single-center studies in a mixed medical/surgical ICU population, both smaller than the Leuven studies, followed and were unable to reproduce a significant mortality benefit.30,31 In contrast, a number of small RCTs in selected subpopulations, mostly focusing on morbidity as primary endpoint, as well as several larger implementation studies revealed improved outcome as did the Leuven studies.32–35
Nice-Sugar
All the described studies were in fact statistically underpowered to detect a reasonable mortality difference. To address this issue, the NICE-SUGAR (Normoglycemia in Intensive Care Evaluation and Survival Using Glucose Algorithm Regulation) included 6100 patients over 41 participating centers.36 This study compared a blood glucose target of below 108 mg/dL (<6.0 mmol/L) versus “usual care,” which meant an intermediate blood glucose target of 140 to 180 mg/dL (8 to 10 mmol/L). Owing to the results from the Leuven studies, clinicians had become aware of the negative impact of hyperglycemia, so tolerating higher glucose levels was considered unacceptable or even unethical by clinicians and investigators. The aim of NICE-SUGAR, therefore, was to assess whether further lowering blood glucose levels to less than 108 mg/dL (<6.0 mmol/L) in a broad context of clinical practice in ICUs, predominantly located in Australia and New-Zealand, and using the normal daily clinical practice tools available would exert additional benefit. Contrary to expectations, NICE-SUGAR revealed that targeting 108 mg/dL with insulin increased 90-day mortality from 24.9% to 27.5% as compared with the 140 to 180 mg/dL (8-10 mmol/L) glucose target. Excess deaths were attributed to cardiovascular causes.
Coiitss
Patients with septic shock requiring administration of glucocorticoids are faced with a high mortality risk; the severity of illness and glucocorticoid treatment make hyperglycemia common. Therefore, this would be an optimal population in whom to study whether TGC could reduce mortality. In the Corticosteroids and Intensive Insulin Therapy for Septic Shock (COIITSS) multicenter study, 509 patients were randomized to either intensive insulin therapy aiming for blood glucose levels between 80 and 110 mg/dL or to conventional insulin therapy.37 In the latter group, an intermediate target was used, as the physicians were recommended to follow the 2004 Surviving Sepsis Campaign Guidelines (blood glucose levels < 150 mg/dL [8.3 mmol/L]). Hospital mortality in the intensive insulin therapy group (45.9%) did not differ from the conventional group (42.9%). Poor separation of the blood glucose levels between the study groups and the small size of the study may have made it hard to detect any treatment effect of TGC.
Meta-Analyses
Nowadays, practice guidelines ideally are based on systematic reviews and meta-analyses. The two most recent meta-analyses showed that in critically ill adult patients, TGC did not significantly reduce hospital mortality but is associated with an increased risk of hypoglycemia.38,39 However, TGC may be beneficial to patients admitted to a surgical ICU.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree