179 Hydrocarbons
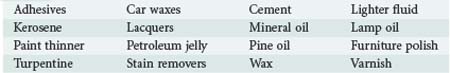
Hydrocarbons are a diverse array of chemicals composed exclusively of hydrogen and carbon atoms. Some hydrocarbon derivatives such as various halogenated hydrocarbons also contain other elements. They are ubiquitous in daily life and include plant and animal fats, alcohols, solvents, natural gas, petroleum derivates, and a host of industrial chemicals (Table 179-1). Many exist in complex mixtures. This chapter focuses on the toxicity of petroleum distillates, which represents several hundred compounds arising from crude oil.1
 Chemistry
Chemistry
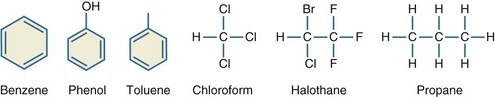
Halogenated hydrocarbons are hydrocarbons with fluorine, chlorine, bromine, or iodine substitutions. Medicinal uses for halogenated hydrocarbons include anesthetics such as halothane, propellants for inhalers, and chloral hydrate for sedation. Refrigerants such as Freon are mixtures of halogenated hydrocarbons (Figure 179-1).2
 Epidemiology
Epidemiology
The Toxic Exposures Surveillance System database maintained by the American Academy of Poison Control Centers reported 46,357 hydrocarbon exposures and 11 deaths in 2008. Eighty-seven percent of all exposures were unintentional or accidental, and 31% occurred among patients younger than 6 years of age.3 The number of hydrocarbon-related calls made by the public or healthcare providers to poison centers over the past decade are decreasing.4 This number certainly underrepresents the actual number of annual exposures.
Determining the incidence of chronic exposures is even more difficult. A 1993 World Health Organization report estimated that 238,000 U.S. workers annually were exposed to benzene.5 Petrochemical workers, rubber workers, shoe manufacturers, and printers all have workplace exposures to benzene,6 but second-hand cigarette smoke, products from gasoline combustion, and industrial emissions expose virtually everyone to benzene, at least occasionally.7,8 Because of its known tendency to promote development of hematologic malignancies, benzene has been extensively studied in terms of its toxic effects. Many other hydrocarbons are encountered in daily life, and the effects of low-level exposures to these compounds are unclear. More than 1 million workers are exposed annually to kerosene and its byproducts.9 Toluene is present in the air in most urban and suburban environments at concentrations up to 6.6 parts per billion (ppb), and it can be found in higher concentrations in soil and water.10
Intentional abuse of inhaled hydrocarbons is a particularly dangerous form of hydrocarbon exposure. In 2007, 13.3% of high school students reported inhalant abuse.11 Among delinquent youth, 38.5% reported inhalant abuse, and 28.3% of inhalant abusers met DSM-IV dependence criteria.12,13 Determining the epidemiology of inhalant abuse is difficult because of the poor reliability of self-reported data and the wide availability of inhalants.14 The use of inhalants as a “gateway drug” is concerning because of the potential for more serious drug abuse later in life.15 Among students, the highest rates of abuse occur in women, Hispanics, and people in rural communities.16
Depending on the type of chemical abused, inhalants are generally categorized as gases, nitrates, solvents, or aerosols.17 Gases are compressed hydrocarbons such as refrigerants, propane, butane, and inhalational anesthetics. Nitrates, or “poppers,” are used as smooth-muscle relaxants to heighten sexual experiences. Solvents are a diverse group of liquids with relatively high vapor pressures and include glues, fuels, paint thinners, and the liquid in felt-tip markers. Aerosols are hydrocarbon-based propellants found in spray bottles. These bottles contain both a gas propellant and a solvent, either of which may be abused. Inverting the can and activating the nozzle selectively releases the gas propellant. Once the gas is released, puncturing the can yields access to the liquid solvent.
Differing methods of inhalant abuse include sniffing, snorting, huffing, and bagging. Sniffing is the passive inhalation of gaseous fumes from a container; snorting refers to insufflation of liquid hydrocarbons into the nasal passageways; huffing is the inhalation of fumes from a rag soaked in solvent; and bagging is the inhalation of fumes from a solvent placed into a paper or plastic bag.18,19
 General Management
General Management
Management of hydrocarbon toxicity depends upon the route of exposure (Table 179-2). Hydrocarbon ingestion without aspiration typically results in mild symptoms. Hydrocarbons are gastric irritants, and 35% to 51% of patients will spontaneously vomit.20–23 Hemorrhagic gastritis following ingestion has been reported.24 If aspiration does not occur, the outcome from ingestion of a hydrocarbon is usually good, especially if respiratory symptoms are absent for 6 to 8 hours and the chest radiograph is normal.3,20–23,25,26
TABLE 179-2 Selected Hydrocarbon Toxicities
| Agent | Toxicity |
|---|---|
| Pentachlorophenol | Oxidative phosphorylation uncoupler |
| Formaldehyde | Irritant, respiratory sensitizer, allergen |
| Diisocyanates | Respiratory sensitizer, allergen |
| Perchloroethylene (PERC) | Central nervous system depression, cardiac sensitization |
| Bromomethane | Severe neurotoxicity |
| Hydrazine-containing fuel | Seizures, pyridoxine depletion |
Given that hydrocarbon toxicity primarily results from pulmonary aspiration, gastric lavage and induced emesis with ipecac should be avoided.26–28 Lavage, spontaneous emesis, and ipecac all increase the risk for hydrocarbon aspiration with subsequent pneumonitis.20,22,26,29 However, it is appropriate to perform gastric lavage or induce emesis when the ingested hydrocarbon is known to cause systemic toxicities, the volume of hydrocarbon ingested is very large, or the hydrocarbon has been ingested along with one or more other dangerous substances.28 Activated charcoal fails to adsorb most hydrocarbons, and its use is not routinely recommended.30,31 Material Safety Data Sheets (MSDS), the Micromedex database, or poison control centers can help identify hydrocarbons that warrant decontamination efforts.
 Nonspecific Symptoms of Aspiration
Nonspecific Symptoms of Aspiration
Fever and leukocytosis are common after hydrocarbon aspiration. Fever occurs in up to 73% of ingestions and 93% of intentional aspirations.20,23,27,32 Approximately 30% of patients with fever are otherwise asymptomatic.22,23 In one study, fever resolved after 24 hours in 41% of patients; 5% of patients had persistent fever lasting longer than 5 days.27 Another study found that fever resolved after an average of 1.25 days.33 Heating or burning hydrocarbons results in the production of many airborne molecules. Inhalation of these molecules can result in a prolonged fever referred to as polymer fume fever.34,35 One study of patients with hydrocarbon ingestion found leukocytosis in 75% of those with clinical pneumonia, versus only 32% in those without pneumonia. Both groups had a similar percentage of patients with a left shift on the differential white blood cell count.23
 Pulmonary Toxicity
Pulmonary Toxicity
Aspiration of hydrocarbons results in a lipoid pneumonia. Chronic ingestion of hydrocarbons among patients with gastroesophageal reflux disease can result in slowly developing symptoms.36,37 Intravenous injection of hydrocarbons can result in a lipoid pneumonia or vascular hydrocarbon emboli.38–41 A case of lipoid pneumonia due to dermal absorption of hydrocarbons in a patient with severe psoriasis was reported.42 This patient suffered from severe psoriasis and applied large amounts of petroleum jelly to her skin for 10 days prior to evidence of lipoid pneumonia. Some halogenated hydrocarbons such as trichloroethylene are mucosal irritants which can induce caustic pneumonitis.43–45 Respiratory tract sensitization and reactive airway disease can occur following repeated exposure to certain hydrocarbons.46–51 Rarely, the irritant effects of some hydrocarbons can result in upper airway injury and obstruction.52
Gastrointestinal absorption plays a minor role in toxicity. Experimental canine and primate models in which esophageal ligation was performed prior to instillation of kerosene by gastrostomy failed to demonstrate pulmonary injury in any of the animals.25,53,54 However, small doses of hydrocarbons administered intratracheally resulted in severe pulmonary toxicity.55–58
Aspiration occurs with the inhalation of a hydrocarbon that exists as a liquid under ambient conditions of temperature and pressure. The risk for pulmonary toxicity is determined in part by the physical properties of liquid hydrocarbons, including surface tension, viscosity, and volatility.59,60 Surface tension refers to the cohesion of molecules generated by van der Waals forces. Materials with low surface tension tend to spread over an area, and therefore these substances are more likely to be aspirated. Viscosity measures the resistance of a fluid to flow. Liquids with low viscosity are more likely to be aspirated.61 Volatility refers to the tendency of a liquid to vaporize into a gaseous state. Volatile hydrocarbons are more lipid soluble and more easily disrupt surfactant layers and/or cell membranes, thereby predisposing to toxicity.61,62 However, hydrocarbons that exist as gases in ambient conditions cannot be aspirated and do not cause lipoid pneumonia. An example is propane, a gas that is purchased as a compressed liquid but which volatilizes completely and rapidly upon return to normal atmospheric pressure. The clinical effects of these gases result from hypoxia and central nervous system (CNS) depression.63–65 European regulation of the allowable viscosity, volatility, and surface tension of lamp oils has not led to an appreciable decline in the incidence of patients developing lipoid pneumonia.66
Multiple mechanisms of pulmonary injury occur in hydrocarbon aspiration. Microscopic findings include thick hyaline membranes in air spaces, capillary distension, vascular thrombosis, intraalveolar hemorrhage, hyperemia, neutrophilic or lymphocytic alveolitis, and bronchial necrosis.37,67,68 The most characteristic finding is the presence of lipid-laden macrophages.67 Foreign body granulomas or “parafinomas” following aspiration have been reported.70,71 Bronchoalveolar lavage (BAL) reveals thick or greasy fluid. Oil red O staining of the fluid can confirm the presence of exogenous lipids, and polymorphonuclear exudates or hemorrhagic secretions can be present.38,72,73 Animal models reveal an early exudative phase characterized by the presence of red blood cells, macrophages, and edema fluid in alveolar airspaces along with diminished lung compliance. This early phase is followed by a secondary phase of proliferative bronchiolitis.68,74 Disruption of the pulmonary surfactant layer from hydrocarbons exacerbates ventilation/perfusion mismatching and decreases pulmonary compliance.75,76
The diagnosis of hydrocarbon aspiration is usually suggested by the history. Coughing, gagging, or choking following ingestion of hydrocarbons portends the development of pulmonary injury, although nearly a third of patients with early symptoms do not develop significant toxicity.22,23,77 Hypoxemia, respiratory distress, and physical examination evidence of pneumonia develop rapidly, although delayed onset of these symptoms has been reported.32,78 Lung function studies reveal a restrictive or obstructive pattern.37 In cases of respiratory distress where it is unknown if hydrocarbon aspiration occurred, bronchoalveolar lavage or lung biopsy can be diagnostic. Uncommon complications of aspiration include the development of pneumatoceles, cavitary lesions, abscesses, lung necrosis, bronchopleural fistula, pneumothorax or empyema.23,71,79–82
Radiographic findings are variable. Ninety percent of patients with pulmonary symptoms have abnormal radiographs on arrival, and nearly all develop abnormalities by 6 hours.22 Interestingly, chest radiograph abnormalities in the absence of respiratory symptoms are common. Fifty percent of asymptomatic patients have abnormal chest radiographs, and of these patients with abnormal roentgenographic findings, only 5% go on to develop significant toxicity.22,27 Chest radiographs can reveal areas of consolidation, atelectasis, fibrosis, ground-glass opacities, or pleural effusions.23,37,83 Bibasilar interstitial or right lobar findings are the most common and can develop within an hour of aspiration.20,23,27 Computerized tomography (CT) reveals airspace consolidation with areas of low attenuation and air bronchograms. Ground-glass opacities, airspace nodules, and/or crazed paving patterns can be seen.84,85 Areas of fat attenuation within pulmonary opacities can be diagnostic, although inflammatory infiltrates can mask this finding.37,83 Magnetic resonance imaging (MRI) reveals T1 hyperintensities consistent with, though not specific for, lipid content.86,87 Chemical shift MR with opposed-phase imaging is sensitive for detecting lipids and can provide a specific test for lipoid pneumonia if available.88 Positron emission tomography (PET) scanning of a patient suspected to have a malignancy but later found to have exogenous lipoid pneumonia revealed a high standard uptake value.89
There are limited data on outcomes following hydrocarbon aspiration. A follow-up of 17 children 8 to 14 years after exposure found that 82% had one or more pulmonary function abnormalities.90 A separate study found normal pulmonary function in 3 children exposed 8 to 10 years earlier.91 A retrospective review of 44 adult patients with chronic lipoid pneumonia found that 21% developed complications including pulmonary fibrosis, recurrent infections in the region of injury, and Aspergillus-related diseases.37
Management of Pulmonary Toxicity
Management of hydrocarbon aspiration focuses on respiratory support. β-Adrenergic agonists are indicated for treatment of bronchospasm.67 Ventilation with high levels of positive end-expiratory pressure and recruitment maneuvers can improve gas exchange.38 High-frequency percussive ventilation resulted in significant clinical improvement in a patient who deteriorated after multiple modes of ventilation had failed, and mobilized a large amount of thick oily secretions.92 Clinical improvement has been reported with high-frequency oscillation or high-frequency jet ventilation93–95 and extracorporeal membrane oxygenation.96
Therapy with corticosteroids remains controversial because human data are limited. A double-blind placebo-controlled trial of 71 children with hydrocarbon poisoning did not reveal any difference between treatment groups.33 There are many case reports with variable outcomes following both oral and inhaled corticosteroid use.37,68,72,97–99 Various animal models have shown no difference in outcome100–102 or worsened outcome due to increased infectious complications.103
Aspiration and the subsequent presence of pneumonia, fever, radiographic findings, and leukocytosis make antibiotic use common, but no controlled human data demonstrate the value of antibiotics. Various animal models have shown no difference in rates of infection when prophylactic antibiotics were given.100,101,103 Given the limitations in data, the authors feel that routine administration of antibiotics is not supported by the literature. We recommend antibiotics only for patients with persistent fever lasting longer than 24 hours, patients with peripheral white blood cell count higher than 20,000 cells/µL, or patients with deteriorating clinical status after 24 hours.
Many additional therapies have been used for lipoid pneumonia. Surfactant therapy for acute respiratory distress syndrome (ARDS) is controversial, but there are reports of successful use of this strategy in cases of hydrocarbon aspiration.75,104,105 An ovine hydrocarbon aspiration model found 100% survival with surfactant therapy versus 25% survival with saline, although all animals were sacrificed at 6 hours.106 A patient with prolonged respiratory compromise underwent lung lavage on hospital day 49. Polysorbate 80 in Ringer’s lactate was used until the effluent was clear of lipid, followed by surfactant instillation. This resulted in clinical and lung aeration improvements.107 Nitric oxide along with high-frequency oscillatory ventilation was used successfully in a pediatric patient.94 A rabbit model using partial liquid ventilation and inhaled nitric oxide showed improvements in gas exchange.108 Animal models of hyperbaric oxygen demonstrated transient improvement in oxygenation followed by rapid decline.100
 Nervous System Toxicity
Nervous System Toxicity
CNS effects vary depending on the route and intent of exposure. Among those with hydrocarbon aspiration secondary to ingestion, one-third have signs of CNS toxicity ranging from drowsiness to stupor and seizures. In this setting, the presence of CNS symptoms correlates strongly with the development of fever, hypoxemia, and pneumonitis.23 Intentional hydrocarbon inhalation produces euphoric effects that mimic ethanol inebriation. Symptoms include mydriasis, nystagmus, hallucinations, increased libido, and delirium. Severe or prolonged exposures can result in tremors, seizures, and hypoxic encephalopathy.109–112 These effects usually resolve within a few hours, although prolonged symptoms can occur in some cases.113
The neurophysiologic effects of inhalants are not completely understood. Inhalation leads to CNS depression via enhanced γ-aminobutyric acid (GABA)-mediated neurotransmission, antagonism of N-methyl-D-aspartic acid receptors, inhibition of normal cell-cell signaling, and enhanced serotonergic transmission.115–119 The release of dopamine reinforces abuse patterns.120 Chronic abusers develop tolerance to these effects and may increase the amount inhaled to compensate.111,121 Because of physical dependence, chronic users can develop inhalant withdrawal symptoms such as craving, irritability, and insomnia.122 Baclofen and lamotrigine have been advocated as treatments for inhalant withdrawal syndromes.123,124
Chronic exposure to solvents, whether intentional or unintentional, can cause a broad spectrum of CNS disorders. Initial symptoms are nonspecific and include memory difficulties, fatigue, loss of concentration, and personality changes that can be reversible.114,125–127 Continued exposure leads to an irreversible leukoencephalopathy that can present as cerebellar ataxia, parkinsonism, encephalopathy, convulsions, and/or deficits in higher functioning.112,128,129 MRI reveals changes in the basal ganglia and thalamus along with cortical and cerebellar atrophy.112,128,130,131 Single photon emission computerized tomography (SPECT) findings have demonstrated prominent abnormalities with areas of hypoperfusion and hyperperfusion.132 Many hydrocarbons are associated with the development of peripheral neuropathy, most notably n-hexane and methyl-n-butyl ketone.126,133–135
 Cardiac Toxicity
Cardiac Toxicity
Sudden sniffing death refers to cardiac arrest following the inhalation of volatile hydrocarbons, especially halogenated derivatives.63,64,136,137 Ingestion or inhalation of halogenated hydrocarbons can cause dysrhythmias that persist for days.138 Sixty-four percent of inhalant-related deaths result from arrhythmias, and most of the remainder result from hypoxia and/or hypercapnia.65,139 Toluene has been shown to prolong the QT interval and inhibit cardiac sodium currents.140,141 Electrophysiologic studies on animals identified concentration-dependent suppression of spontaneous pacemaker activity, resulting in asystole, though some animals developed ventricular tachydysrhythmias. Cardiotoxicity worsens in the setting of acidosis or hypoxemia,142–144 and toxicity persists for hours after exposure.144 Autopsy findings are usually nonspecific,65 although myocardial fibrosis induced by hydrocarbon abuse can increase the risk of dysrhythmias.145 Coronary artery spasm and infarction contribute to toxicity.146,147 The myocardium may be sensitized to catecholamines following inhalant abuse, and thus sudden excitation or exercise can trigger ventricular dysrhythmias.148,149 Administration of epinephrine worsened inhalant-induced cardiotoxicity in a canine model.150 Therefore the management of cases of hydrocarbon-induced toxicity should eschew the use of epinephrine or other adrenergic agonists.137 β-Adrenergic blockers can blunt myocardial sensitization and have been used successfully in the treatment of ventricular dysrhythmias secondary to hydrocarbon toxicity.138 Amiodarone and lidocaine also have been used successfully to terminate ventricular arrhythmias.137,151