
Hip and Femur Injuries
Carl A. Germann and Megan L. Fix
Hip injuries are common and associated with notable morbidity and mortality, especially in older patient populations. It is predicted that by the year 2050, 6.3 million hip fractures will occur yearly worldwide (1). Causes of hip fracture are primarily pathologic (from osteopenia) and falls, whereas motor vehicle collisions account for the majority of hip dislocations.
Anatomically, the hip is an articulation between the femoral head and the acetabulum. The femoral head is firmly seated in the acetabulum, which is reinforced by labral cartilage, capsule, overlying ligaments, and proximal musculature of the lower extremity (Fig. 43.1). It is a very stable articulation, requiring violent injury to fracture or dislocate. The femur is the longest and strongest bone in the human body and is often subjected to substantial forces produced during powerful muscle contraction, weight transmission, or trauma. The length, angle, and narrow circumference of the femoral neck allow substantial range of motion at the hip, but these same characteristics subject the neck to incredible shearing forces.
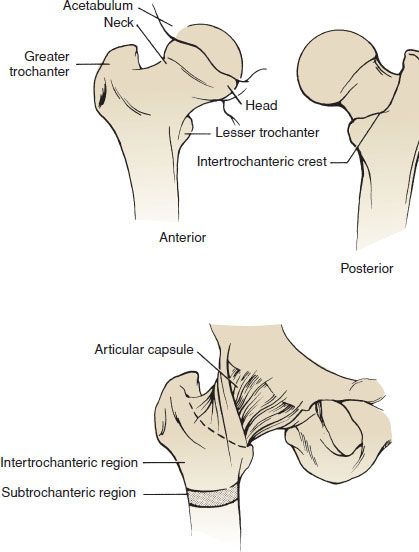
FIGURE 43.1 Anatomy of the hip. Anterior and posterior views of the femur (top) and division of the proximal femur (bottom).
Primary sources of blood flow for the femoral head are the retinacular branches of the circumflex femoral artery. These arteries enter the femur in the region of the femoral neck; fractures proximal to their entry can result in disruption of blood flow and cause avascular necrosis (AVN) of the femoral head.
ED EVALUATION
During the initial evaluation, details of the mechanism of injury as well as a thorough physical examination and search for associated neurovascular injuries are imperative. The initial radiographic studies in patients with suspected hip and femur injuries are the anteroposterior (AP) and lateral views. When analyzing the AP view of the hip, there are two important radiographic lines that help identify femur fractures and slipped capital femoral epiphysis (SCFE): Shenton and Klein lines. The Shenton line is a gentle arc seen on the AP view that runs along the inferior border of the femoral neck and extends to the inferior border of the superior pubic ramus (eFig. 43.1). The Shenton line will have a step or discontinuity in subtle cases of femoral neck and head fractures. The line may also appear disrupted in the radiograph of a normal hip, if it is not a true AP view. Klein line runs along the superior border of the femoral neck and intersects the superior portion of the femoral head (eFig. 43.2). The Klein line will project superior to a subtle fracture of the femoral head. The Klein line will also project superior to the epiphysis in a subtle case of SCFE.

FIGURE 43.2 Posterior hip dislocation.
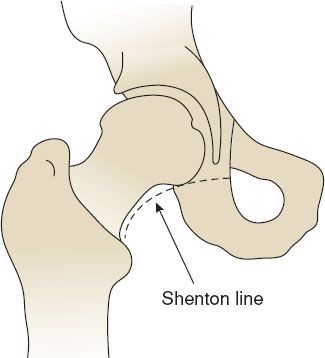
eFIGURE 43.1 The Shenton line. (From Gruber JE, Gibbs MA, Ferrera PC, et al. Trauma Management: An Emergency Medicine Approach. St. Louis, MO: Mosby; 2001:398 (Figure 26–2), with permission.)
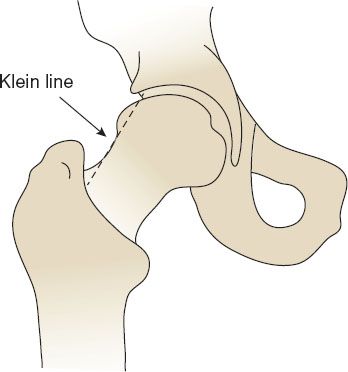
eFIGURE 43.2 The Klein line. (From Gruber JE, Gibbs MA, Ferrara PC, et al. Trauma Management: An Emergency Medicine Approach. St. Louis, MO: Mosby; 2001:398 (Figure 26–3), with permission.)
Approximately 2% to 10% of all hip fractures are radiographically “occult” on plain films (2). Therefore, if clinical suspicion remains and plain radiographs are negative, magnetic resonance imaging (MRI) is indicated. Although computed tomography (CT) scan can be used, small studies suggest that it is inferior to MRI (2,3). CT does seem to have merit when the patient does not have significant osteoporosis or in the setting of significant trauma (3). MRI is the imaging modality of choice with a sensitivity and specificity approaching 100%. In studies of patients with suspicion of hip fracture and normal plain radiographs, MRI showed occult fracture in 37% to 55% of patients (4).
KEY TESTING
• The initial radiographic studies in patients with suspected hip and femur injuries are the AP and lateral views.
• If clinical suspicion remains high and plain radiographs are negative, MRI is recommended to evaluate for occult fracture.
• Failure to detect these injuries results in increased mortality, risk of subsequent displacement, and a higher incidence of complications such as AVN.
ED MANAGEMENT
Hip Dislocations
The relationship of the femoral head to the acetabulum is used to classify dislocations into posterior, anterior, inferior, and central. Posterior dislocations account for 80% to 90% of cases. Anterior dislocations are seen in 10% to 15% of patients. Inferior dislocation (luxatio erecta) of the hip is very rare and occurs almost exclusively in children younger than 7 years of age. Central dislocation is often used to describe the translocation of the hip joint causing a comminuted fracture of the acetabulum.
The neurovascular examination after a hip dislocation should focus on the sciatic nerve and femoral nerve and vessels. Sciatic nerve palsy is more likely to occur in conditions such as traumatic dislocation of a nonprosthetic hip or during the total hip arthroplasty (THA) procedure itself. Sciatic palsies may be present in approximately 10% of patients who experience traumatic hip dislocation. The sciatic neuropathy may produce paralysis of the peroneal muscles. The femoral artery and its branches are the most likely vessels to be injured, particularly after an anterior dislocation. The development of AVN of the femoral head caused by arterial injury has been reported in 1% to 17% of dislocations (5). Risk factors for the development of AVN include the total dislocation time, severity of the injury, number of reduction attempts, and presence of comorbid conditions. The incidence of AVN, traumatic arthritis, permanent sciatic nerve palsy, and joint instability logarithmically increases with the length of time for which the hip remains dislocated (6). Of course, prosthetic femoral heads are not at risk for developing AVN.
Posterior Hip Dislocations
Posterior hip dislocations are the most common type of hip dislocation and result from force applied to a flexed knee and hip. These injuries usually occur as a result of motor vehicle crashes where a seated occupant typically has the hip adducted, flexed, and internally rotated at the time of impact. This injury may be prevented by the use of a lap belt.
In posterior hip dislocations, the limb is often found flexed, adducted, internally rotated, and shortened. The knee of the affected extremity often rests on the opposite thigh. The greater trochanter may be unusually prominent. Likewise, the femoral head can often be palpated in the buttocks region (Fig. 43.2 and eFig. 43.3). Examination of the leg should ensure vascular function (rarely compromised) and include neurologic evaluation for possible sciatic nerve injury. Up to 50% of dislocations are associated with acetabular or femoral head fractures.

FIGURE 43.3 Slipped capital femoral epiphysis. A 13-year-old boy with a severe left-sided SCFE. (From Swiontkowski MF, Stovitz SD. Manual of Orthopaedics. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006.)
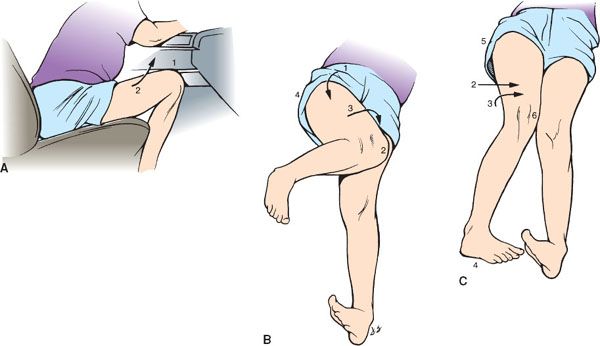
eFIGURE 43.3 Posterior dislocation of the hip. A: Mechanism of injury: The knee (1) strikes the dashboard. The thigh (2) is forced into flexion and adduction, and the femoral head is driven backward out of the acetabulum. B: Ischial dislocation: The hip (1) is flexed. The hip is markedly adducted, so that the knee (2) of the affected limb lies on the opposite thigh. The limb (3) is in extreme internal rotation. The greater trochanter and buttock (4) on the affected side are unusually prominent. C: Iliac dislocation: As in (B), the hip is flexed and is adducted (2).
Optimally, posterior dislocations should be reduced within 6 hours to minimize the risk for AVN (7). Therefore, this procedure should be attempted in the emergency department (ED) (eFig. 43.4). Adequate analgesia and muscle relaxation must be obtained using appropriate agents (e.g., a short-acting opioid and a short-acting benzodiazepine or propofol) and monitoring.
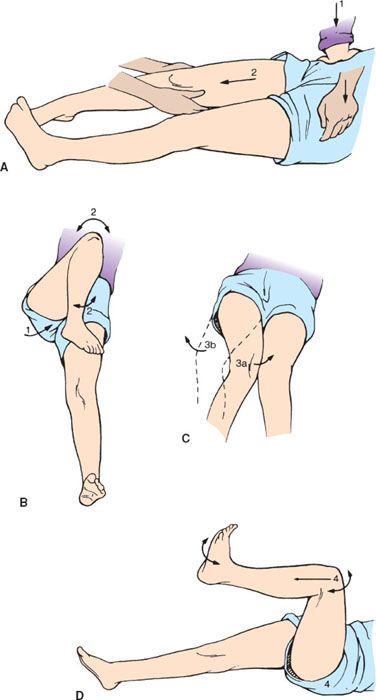
eFIGURE 43.4 Posterior dislocation of the hip: method of manipulative reduction. A: The assistant holds downward pressure (1) on the anterior superior iliac spine. With the knee flexed (2), the operator pulls on the limb in the line of deformity. B: The assistant slowly brings the thigh (1) to 90 degrees of flexion. The assistant gently rotates the thigh internally and externally and rocks the thigh (2) backward and forward to disengage the head from the external rotator muscles and the posterior capsule. C: The assistant relocates the femoral head by further internal rotation and extension of the thigh (3a) or external rotation and extension of the thigh (3b). D: The assistant pushes firmly on the trochanter to direct the femoral head into the acetabulum while the limb is rotated and extended (4). Forceful rotation should be avoided, because it can fracture the femoral neck. If the reduction is not accomplished with two adequate attempts, open reduction is indicated.
Among the several techniques described in the literature, the Allis technique is commonly used to relocate posterior hip dislocations. After the patient is adequately sedated, the hip is flexed and an upward traction is applied to the supine patient. An assistant may apply pressure to the iliac crests, stabilizing the pelvis from lifting off the bed. To apply constant traction to the leg, it is often necessary to stand on the bed and straddle the patient. Upward traction and continued longitudinal force is applied with gentle internal and external rotation. Successful reduction is often felt by a dull click. After reduction, the extremity should be placed in extension and neurovascular function of the extremity should be reassessed. Postreduction radiographs should be obtained to identify the proper location of the femoral head. General anesthesia is occasionally necessary if procedural sedation is unsuccessful.
Anterior Hip Dislocations
Anterior hip dislocations occur most commonly from a direct blow to the abducted hip. A distally applied force causes the femoral head to tear through the anterior capsule and lever out of the acetabular cup. The mechanism of injury is most often an MVC during which the occupant has the hip abducted and externally rotated at the time of impact or a fall or sports injury causing forced hyperextension. Anterior dislocations are classified as obturator, iliac, and pubic (eFig. 43.5).
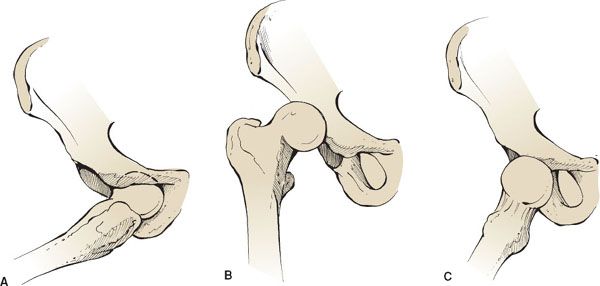
eFIGURE 43.5 Anterior hip dislocations. Anterior obturator hip dislocation (A), anterior iliac hip dislocation (B), and anterior pubic hip dislocation (C).









