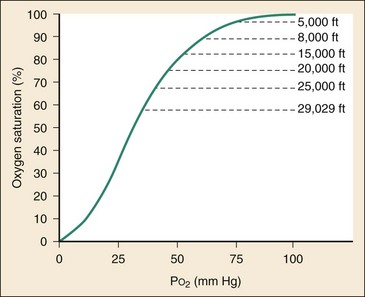
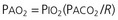
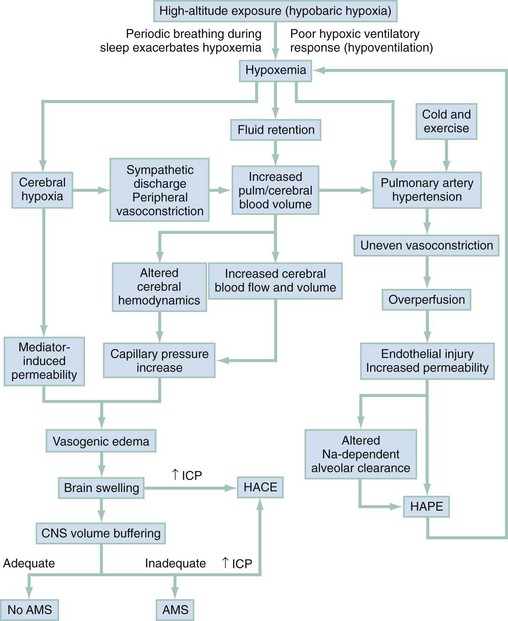
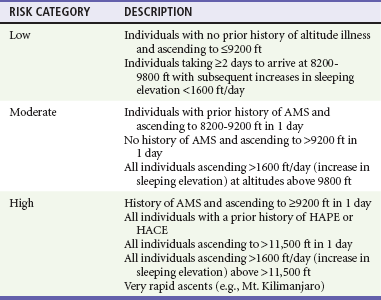
Chapter 144 Worldwide, it is estimated that approximately 40 million individuals live above 8000 feet, and 25 million live above 10,000 feet.1 Rather than these high-altitude residents, the groups at risk for acute altitude illnesses are those who ascend into mountainous regions. Mountain sports activities and tourism are attracting increasing numbers of participants each year. This, combined with the rapid ascent, made possible by air transportation results in more unacclimatized individuals at risk for high-altitude illness. More than 1 million visitors travel annually to the remote high mountain ranges of Asia, Africa, and South America.1 Approximately 35 million visitors travel annually to high-altitude recreation areas in the western United States.1 The incidence of high-altitude illness depends on many variables, including the rate of ascent, previous altitude exposure, and individual genetic susceptibility.2,3 Sleeping altitude, final altitude reached, and duration of stay at altitude are also risk factors for AMS development.4 AMS is common (67% incidence) among mountain climbers on Mt. Rainier who ascend quickly (1 or 2 days) to 14,410 feet.5 Trekkers who fly into the Khumbu region to explore the Mt. Everest area have a higher incidence of AMS (47%) compared with those who walk (23%).6 Skiers who visit resorts in the western United States from sea level generally fly or drive to the region but sleep at relatively lower altitudes than the other groups mentioned. Among this population, AMS occurs in approximately 25%.7 Given the large number of visitors (approximately 25 million) in Colorado each year, this is not a trivial matter. The incidence of HAPE varies from 0.01 to 2% in most studies but has reached 15.5% among soldiers flown directly to 14,500 feet without a chance to acclimatize at a lower altitude.6,8 The incidence of HACE is lower, and although it frequently occurs with HAPE, it can be seen as an isolated entity. Both HAPE and HACE are more common with a longer duration of visit and higher sleeping altitude. Age may be a relative risk factor. Most studies of children suggest that they have the same incidence of AMS as adults do.9–12 One small study of tourists in Chile evaluated children 4 to 48 months old and found higher AMS scores and lower oxygen saturations compared with those of their parents.13 Younger individuals (<20 years old) are more likely to have HAPE, although HAPE is extremely rare in children younger than 2 years. Gender does not affect the incidence of AMS2; however, women may have less risk for development of HAPE.6,7,14,15 No relationship appears to exist between AMS development and the menstrual cycle.16 The number of older travelers visiting mountain resorts is increasing. Many of these individuals have underlying health problems, including lung disease (10%), heart disease (25%), and hypertension (30%). Despite these conditions, the risk for AMS development in adults older than 50 years may be less than in younger age groups.2,17 One study found no difference in the incidence or severity of AMS in climbers older than 50 years compared with a matched cohort of younger climbers.18 Nevertheless, there are indications that elders may not react well to acute high-altitude exposure. Pulmonary vital capacity decreases almost one third in elders ascending from sea level to 14,000 feet for 1 week, producing a large decrease in both oxygen saturation and maximal oxygen uptake during exercise. High altitude is between 10,000 and 18,000 feet. Most serious altitude illness occurs at these levels. The pathophysiologic effects of high altitude begin when the oxygen saturation of the arterial blood begins to fall below the 90% level. The sigmoidal shape of the oxyhemoglobin dissociation curve prevents a significant fall of arterial oxygen saturation (SaO2) in most individuals until an altitude of approximately 12,000 feet. At this altitude, the steep portion of the curve is encountered, and marked oxygen desaturation may occur with relatively small increases in altitude (Fig. 144-1). Some predisposed individuals may desaturate to less than 90% at altitudes as low as 8000 feet. Barometric pressure decreases logarithmically as the altitude rises. The partial pressure of oxygen (PO2) in the atmosphere also decreases as altitude rises, but it remains a constant 20.93% of the barometric pressure. The shape of the earth is slightly flat at the poles and bulging at the equator. The atmospheric envelope that surrounds the earth has a similar shape; therefore, the barometric pressure is lower at higher latitudes than it is at the equator. For example, it has been calculated that it would be impossible for a climber to reach the summit of Mt. Everest without supplemental oxygen if the mountain happened to be in a more northern latitude.19 Acclimatization begins at the altitude that causes the oxygen saturation of arterial blood to fall below sea-level values. The altitude at which this occurs depends on the rate of ascent, the duration of exposure, and the individual’s physiology. People with preexisting conditions that reduce oxygen saturation or content may have a decreased altitude tolerance. Of particular importance are both acute and chronic cardiac and respiratory illnesses. Most healthy, unacclimatized visitors to high altitude will not desaturate significantly (to less than 90%) until they reach elevations higher than 8000 feet.1 The risk of high-altitude illness also depends on an individual’s inherent ability to acclimatize. Some people acclimatize easily without having any clinical symptoms. Others may transiently have AMS during acclimatization, and a few have marked reactions to altitude exposure, developing severe altitude illness. This variability involves many genetic and epigenetic factors that moderate the process of acclimatization.3,20 Previous successful acclimatization may be predictive of future responses for adults in similar conditions, but this may not be the case for children.21 One of the most important physiologic changes that occurs during acclimatization is an increase in minute ventilation, causing a decrease in the partial pressure of carbon dioxide (PACO2). The alveolar gas equation states that as the PACO2 decreases, a corresponding increase in PAO2 occurs, thereby increasing arterial oxygenation (Box 144-1). Thus the level of ventilation determines alveolar oxygen for a given inspired oxygen tension. When a person arrives at high altitude, the peripheral chemoreceptors in the carotid bodies respond to a decrease in PAO2 and signal the respiratory control center in the medulla to increase ventilation. This increase in ventilation is known as the hypoxic ventilatory response (HVR), which may be inhibited or stimulated by numerous factors, including ethanol, sleep medications, caffeine, cocoa, prochlorperazine, and progesterone. The magnitude of the HVR varies among individuals and may be genetically predetermined.22 As ventilation increases, a respiratory alkalosis occurs that acts as a negative feedback system on the central respiratory center, limiting any further increase in ventilation. Within 24 to 48 hours of ascent, the kidneys excrete bicarbonate in an effort to compensate for the alkalosis. As the pH normalizes, ventilation rises slowly, reaching a maximum after 6 to 8 days. This process is enhanced by acetazolamide. The ability to achieve an adequate HVR varies and is related to the ability to acclimatize. A low HVR and relative hypoventilation are implicated in the pathogenesis of both AMS and HAPE.23 For the majority of people with intermediate HVRs, however, ventilatory drive probably has no predictive value for AMS development.24 The release of catecholamines on ascent stimulates the circulatory system to increase cardiac output. This is manifested by an elevation in heart rate, blood pressure, cardiac output, and venous tone.25 Except at extreme altitudes, acclimatization results in the gradual return of the resting heart rate to near sea-level values. Resting relative tachycardia is evidence of poor acclimatization. As the altitude increases, a decrease in maximal heart rate capacity occurs, and at the limits of acclimatization, maximal and resting heart rates converge. The hematopoietic response to high-altitude acclimatization consists of an increase in both hemoglobin and the number of red blood cells. An early increase of up to 15% occurs in mean corpuscular hemoglobin concentration after rapid ascent to high altitude. This is primarily a result of a fluid shift into the extravascular space. Long-term acclimatization leads to an increase in plasma volume and total blood volume. Erythropoietin is secreted in response to hypoxemia within hours of ascent, which in turn stimulates the production of red blood cells, leading to new circulatory red blood cells in 4 or 5 days.26 During the next 2 months, red blood cell mass increases in proportion to the degree of hypoxemia.27 Hypoxemia also results in an increase in 2,3-diphosphoglycerate, causing a rightward shift of the oxyhemoglobin dissociation curve, which favors a release of oxygen from the blood to the tissues. This is counteracted by the leftward shift of the oxyhemoglobin dissociation curve caused by the respiratory alkalosis from hyperventilation. The result is a net null change in the oxyhemoglobin curve and an increase in oxygen-hemoglobin binding in the lung, which raises SaO2.28,29 Some individuals with mutant hemoglobin and high oxygen-hemoglobin affinity are found to acclimatize more efficiently than their normal counterparts at moderate altitudes.30 The symptoms of AMS develop several hours after arrival at high altitude, whereas the development of HAPE and HACE generally requires several days of altitude exposure. Because hypobaric hypoxemia occurs within minutes of arrival, it cannot be the direct cause of high-altitude illness. Instead, it appears to be the initiating factor for a complex pathologic process that leads to the development of the various clinical syndromes. The proposed mechanisms for the development of AMS, HAPE, and HACE are represented schematically in Figure 144-2. The centrally mediated periodic breathing associated with high-altitude exposure may result in periods of apnea during sleep, causing severe arterial oxygen desaturation, which further exacerbates hypoxemia.31 Significant hypoxemia initiates multiple systemic responses that involve the circulatory, pulmonary, endocrine, and central nervous systems. Hypoxemia alters fluid homeostasis, resulting in a generalized fluid retention followed by the shift of fluid into the intracellular spaces. This is manifested by peripheral edema, decreased urinary output, and increased body weight in patients with AMS. Several different mechanisms may account for these fluid shifts, including arginine vasopressin levels and sympathetic stimulation that may be centrally mediated.32,33 Arginine vasopressin levels are elevated in some cases of AMS and HAPE and decreased in others.34,35 Aldosterone, plasma renin, and atrial natriuretic levels are higher in people with AMS.35–37 The hypoxemia that results from high-altitude exposure also causes an increase in pulmonary artery resistance, leading to pulmonary hypertension and elevated capillary pressures that play the cardinal role in the development of HAPE. Exercise and cold stress at altitude may increase hypoxemia and exacerbate pulmonary hypertension.38,39 Pulmonary blood volumes and pulmonary hypertension are increased by sympathetic nervous system stimulation and catecholamine release.40,41 In HAPE-susceptible individuals, pulmonary hypertension becomes severe, and an uneven distribution of pulmonary vasoconstriction results in overperfusion, increased capillary pressures, distention, and leakage in the remaining vessels.42–45 This explains the patchy nature of the infiltrate seen on a chest radiograph with HAPE (Fig. 144-3). The mechanism for the uneven vasoconstriction in HAPE may be due to decreased nitric oxide bioavailability at the pulmonary tissue level, also leading to increased endothelial leakage and extracellular edema.46–48 Overperfusion of a restricted vascular bed as the pathogenesis of HAPE is supported by the observation that people born with congenital unilateral absence of a pulmonary artery are susceptible to HAPE.49 These individuals deliver their entire cardiac output to one lung, predisposing them to overperfusion injury. The importance of the excessive rise in pulmonary artery pressure in HAPE is emphasized because lowering of the pressure during ascent prevents HAPE.50 This implicates increased vascular pressure rather than inflammation as the primary cause of the vascular leak. The resultant mechanical shear forces lead to endothelial damage and changes in membrane permeability.48 Inflammatory mediators appear to be a secondary response to the mechanical injury caused by overperfusion.44,51 Once the vascular leak occurs and alveolar fluid accumulates, a defect in transepithelial sodium transport impairs the clearance of alveolar fluid and contributes to HAPE development.52–54 Alveolar fluid clearance is upregulated by beta-adrenergic agonists, and inhaled beta-agonists may successfully prevent and treat HAPE.54,55 Preexisting inflammation may also be a risk factor for HAPE. A preexisting respiratory infection during ascent to high altitude increases susceptibility to HAPE, particularly in children.56 Inflammation may “sensitize” the pulmonary endothelium to mechanical injury and increase susceptibility to alveolar fluid accumulation and HAPE during ascent. The clinical manifestations of AMS and HACE are the result of central nervous system dysfunction. The mechanistic theories involve altered cerebral hemodynamics and inflammatory mediators.57,58 It is known that the vasodilatory response to hypoxemia causes an increase of cerebral blood flow and volume.59,60 The resulting hypoxemia leads to impaired vascular autoregulation, causing increased pressure transmission to the brain’s capillary beds.33,61,62 In addition, systemic hypertension from strenuous exercise at high altitude may overwhelm the brain vasculature, resulting in transcapillary leakage and vasogenic edema. In susceptible individuals, these hemodynamic changes are likely to contribute to clinical manifestations of AMS and HACE.63–65 Additional circumstances, however, may be necessary for the development of vasogenic edema and clinical symptoms. Inflammatory mediators may contribute to edema formation. Vascular endothelial growth factor, the inducible form of nitric oxide synthase, reactive cytokines, and free radical formation may mediate brain endothelial permeability. The roles that these play in the pathophysiologic process of altitude illness remain unclear.57,66–69 Whereas vasogenic edema has been implicated in the origin of AMS, magnetic resonance imaging (MRI) reveals signal changes present in subjects with and without clinical AMS. Thus the significance of vasogenic edema in AMS is questioned.70 In patients with HACE, MRI studies reveal white matter changes consistent with vasogenic edema that correlate with symptoms.71 Despite the unclear role of vasogenic edema, a breakdown of the blood-brain barrier remains the leading theory in AMS and HACE pathophysiology and is most likely due to a combination of mechanical factors and biochemical mediation of permeability.59,72 MRI data do reveal that cytotoxic edema is also present in severe AMS.73,74 Cytotoxic edema results from hypoxic cell damage most often associated with ischemic hypoxic insults. Failure of the adenosine triphosphate–dependent sodium pump allows sodium to accumulate within the cells, increasing intracellular water to maintain the osmotic equilibrium. Cytotoxic intracellular water accumulation may not be the primary mechanism for the development of HACE but rather the result of the increased cell ischemia initially caused by hemodynamic changes, vasogenic edema, biochemical mediators, and increased ratios of brain volume to intracranial space.71,75 Hypobaria also appears to play a role in the development of AMS. Sea-level experiments that expose subjects to hypoxia alone do not result in AMS; however, when hypoxia is combined with hypobaria, AMS does occur.76,77 Although microbubble formation and fluid retention may be a mechanism, the exact pathophysiologic role of hypobaria in altitude illness is unclear.77 These responses to hypoxia and altitude exposure occur in both susceptible individuals and those who remain free of AMS. Thus there must be an overall factor in a subject at risk for AMS that fails to compensate for the changes associated with altitude exposure. The “tight fit” hypothesis is proposed to explain AMS development and its inherent individual susceptibility.59,78 This theory suggests that the development of AMS and HACE is due to a lack of intracranial space to accommodate increasing volume from brain swelling and edema that develop at altitude.58 The adequacy of the space to buffer changes in brain and cerebrospinal fluid (CSF) volume plays a key role in determining which individuals have symptoms of altitude illness. As brain volume increases from increased cerebral blood volume, the volume-buffering capacity of the central nervous system may prevent an immediate rise of intracranial pressure. As brain volume increases, the intracranial CSF is displaced through the foramen magnum into the space available in the spinal canal. Increased absorption of CSF by the arachnoid villi and decreased CSF production also occur. Individuals with less intracranial and intraspinal CSF buffering capacity have less compliance and become more symptomatic (i.e., develop AMS) from mild brain swelling. This tight fit hypothesis is supported by lumbar puncture, MRI, and computed tomography studies.59,78–80 For the diagnosis of AMS, a patient must be in the setting of a recent gain in altitude, be at the new altitude for at least several hours, and report a headache plus at least one of the following symptoms: gastrointestinal upset (anorexia, nausea, or vomiting), general weakness or fatigue, dizziness or lightheadedness, or difficulty in sleeping (Box 144-2).81 The headache may vary from mild to severe, is generally bitemporal and throbbing in nature, and is worse during the night and on awakening or on suddenly becoming upright. Anorexia and nausea, with or without vomiting, are common, and the other symptoms described can range in severity from mild to incapacitating. The disturbance of sleep caused by periodic breathing is common in all visitors to high altitudes but is exacerbated in the setting of AMS. The symptoms of AMS develop within a few hours after arrival at high altitude and generally reach maximum severity between 24 and 48 hours, followed by a gradual resolution. Most individuals become symptom free by the third or fourth day. Those who do not resolve their symptoms should descend because they may develop more serious manifestations of altitude illness, especially if they continue to ascend. Among infants and very young children, AMS is manifested by increased fussiness, decreased playfulness, decreased appetite, and sleep disturbance.10 In most cases of AMS in very young children, all of these symptoms are present. In children, many of the symptoms manifested by AMS can also result from the disruption of normal routine. A change in environment, sleeping accommodation, or eating habits can result in a fussy, unhappy child. In addition, the occurrence of an acute illness can also mimic AMS in young children. If occult bacteremia or another serious illness is suspected in a young child, descent to lower altitude is recommended to eliminate the confounding variable of altitude illness. Ultrasonography is emerging as an early, noninvasive diagnostic tool to assess intracranial pressure.82 Studies have demonstrated that elevated intracranial pressure is associated with AMS and HACE. Increasing intracranial pressure correlates directly with optic nerve sheath diameter.83 It is possible to demonstrate that subjects with symptoms and signs of AMS or HACE have enlarged optic nerve sheath diameters, which may be a useful adjunct in the diagnosis of AMS and HACE.84,85 Treatment of headache, nausea, and insomnia can be beneficial during the course of mild AMS. Aspirin, ibuprofen, and acetaminophen are useful for the treatment of high-altitude headache. Narcotic analgesics should be avoided because of depression of the HVR and respiratory drive during sleep. For nausea and vomiting, prochlorperazine, unlike other antiemetics, stimulates the HVR.86 Periodic breathing causes insomnia, which is best treated with the respiratory stimulant acetazolamide.87 Doses of acetazolamide as low as 62.5 to 125 mg at bedtime may prevent periodic breathing and eradicate insomnia. Benzodiazepines and other sedative-hypnotics should be avoided because of their tendency to decrease ventilation during sleep. Some climbers experience unusual reactions to diazepam at high altitudes, including agitation, hallucinations, and disorientation. These reactions can occur in individuals who have previously used diazepam at lower altitudes without any difficulties.88 Some studies suggest that low doses of benzodiazepines alone or in combination with acetazolamide are safe at high altitude.89–92 Nonbenzodiazepine sleep agents (zolpidem and zaleplon) do not depress ventilation and may prove useful in AMS-related insomnia.93 Acetazolamide accelerates acclimatization and, if it is given early in the development of AMS, rapidly resolves symptoms. A dose of 250 mg of acetazolamide at the onset of symptoms and repeated twice daily is effective therapy for AMS.94,95 The treatment of AMS in children is not formally studied, but anecdotal experience supports the use of acetazolamide in children.96 The dose for children is 2.5 mg/kg/dose given twice daily to a maximum of 250 mg. Acetazolamide is a carbonic anhydrase inhibitor that induces a renal bicarbonate diuresis, causing a metabolic acidosis that increases ventilation and arterial oxygenation. This respiratory stimulation improves sleep when the hypoxemia caused by periodic breathing is eradicated by acetazolamide. The diuretic effects attenuate fluid retention common in patients with AMS. This agent also lowers CSF volume and pressure, which may play an additional role in its therapeutic and prophylactic use. Non–carbonic anhydrase inhibitory effects of acetazolamide include chemoreceptor effects on ventilatory drive, alterations of cerebral blood flow, relaxation of smooth muscles, and upregulation of fluid resorption in the lungs.97,98 The most common adverse reactions to acetazolamide are paresthesias and polyuria. Less common reactions include nausea, drowsiness, tinnitus, and transient myopia. Carbonic anhydrase inhibition at the tongue causes dysgeusia, altering the flavor of carbonated beverages, including beer. Acetazolamide is a nonantibiotic sulfa compound that carries a low risk of cross-reactivity for individuals with an allergy to sulfa antibiotics.99 Those with known sulfonamide allergy may consider administration of a trial dose of acetazolamide in a controlled environment before ascent. A history of anaphylaxis or severe skin reactions to any sulfa-containing medication makes the use of acetazolamide contraindicated. Acetazolamide should be avoided in breast-feeding mothers and pregnant women. Dexamethasone is an effective alternative treatment of AMS. An initial dose of 8 mg is followed by 4 mg every 6 hours.100 No significant adverse reactions are reported; however, symptoms can recur when the treatment is withdrawn. Although dexamethasone can resolve the symptoms of AMS, it does not play a role in acclimatization. Concurrent use with acetazolamide is advocated by some to promote acclimatization.101,102 It is known to have anti-inflammatory properties, possibly to reduce cerebral blood flow,103 and to block the action of vascular endothelial growth factor.66 Reduction of AMS symptoms with the use of dexamethasone may be the result of these or its euphoric effects. We believe that dexamethasone should generally be reserved for use in the setting of acetazolamide intolerance or in more advanced cases of AMS, especially to help facilitate descent. Most of the symptoms of mild AMS are benign and well tolerated. These symptoms, however, can be unpleasant and debilitating to the point that travel, business, or vacation plans should be interrupted. Up to 50% of individuals with AMS report a decrease in activity.7 Altitude preexposure regimens in artificially hypoxic environments have been evaluated to facilitate acclimatization. It appears that little protection from subsequent altitude exposure occurs with preexposure regimens lasting less than 8 to 12 hours.104,105 Mild to moderate exercise is thought to aid in acclimatization; however, overexertion can contribute to the development of AMS.38 Maintenance of adequate hydration is also recommended. Guidelines for adequate hydration should target relatively clear (unconcentrated) urine and normal volume of urine output. Recommendations for hyperhydration are frequently given in the lay literature, yet no evidence supports this advice.106,107 Drinking of excessive amounts of free water may lead to hyponatremia and possibly complicate altitude illness. The rate of ascent and prior history of altitude illness should be considered in the assessment of the risk for development of altitude illness and the choice of prevention strategies (Table 144-1). Individuals in low-risk situations should not need medications for prophylaxis, and ascent should be gradual to prevent illness. In some cases, such as arrival at a high-altitude airport or the immediate dispatch of rescue personnel to high altitude, a slow ascent is impossible. Mountain climbers commonly ascend at rates that are higher than recommended, and some individuals continue to suffer AMS symptoms despite gradual ascent. Individuals who have a known susceptibility to the development of AMS and those for whom slow ascent is impractical fall into the moderate- and high-risk categories and should consider prophylactic medication in addition to gradual ascent.4 Table 144-1 Risk Categories for Acute Mountain Sickness Modified from Luks AM, et al: Wilderness Medical Society consensus guidelines for the prevention and treatment of acute altitude illness. Wilderness Environ Med 21:146-155, 2010. Numerous studies demonstrate the effectiveness of acetazolamide in prevention of AMS in adults.5,6,108 Lower dosages provide prophylaxis similar to that of higher dosages with fewer adverse reactions. Many studies demonstrate that 250 mg twice daily starting 24 hours before ascent and continuing for the first 2 days at high altitude is effective. For avoidance of side effects, a dose of 125 mg given twice daily is effective.4 Although it is unstudied, the recommended dosage of acetazolamide for AMS prophylaxis for children is 2.5 mg/kg/dose up to 125 mg total given twice daily, and this weight-based approach may reduce side effects in smaller adults. Ibuprofen compared with acetazolamide is equally efficacious in preventing headache.109 Dexamethasone also prevents AMS.103 The lowest effective dosage is 2 mg every 6 hours or 4 mg every 12 hours.4,110 Some patients experience the rapid onset of AMS after dexamethasone is discontinued. Dexamethasone does not facilitate acclimatization but rather reduces nausea and enhances mood. In most cases, dexamethasone use should be reserved for treatment of AMS rather than for prophylaxis. Military or rescue personnel rapidly ascending to high altitude and individuals with acetazolamide intolerance are candidates for prophylaxis with dexamethasone. The combination of acetazolamide and dexamethasone may be more effective than either drug alone.101 Because of its antioxidant properties, Ginkgo biloba was proposed for preventive therapy of AMS. The results of several studies are mixed, with some supporting the use of ginkgo and others showing no evidence to support a role in AMS management.111,112 These contradicting findings may be due to the variability of composition among commercially available ginkgo products, and thus determination of its clinical usefulness in the prevention or treatment of AMS is difficult.113 Acetazolamide remains the compound of choice for AMS prophylaxis.
High-Altitude Medicine
Epidemiology
Definitions
Environmental Considerations
Acclimatization
Pathophysiology
Acute Mountain Sickness
Management
Prevention
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree