Heart Failure
Felipe Urdaneta
Charles T. Klodell
Emilio B. Lobato
CASE SUMMARY
A 63-year-old patient is scheduled to undergo a transurethral resection of the prostate. His medical history is pertinent for diabetes mellitus, hypertension, hypercholesterolemia, and heart failure. His medications include furosemide, metoprolol, enalapril, and digitalis.
Currently, he has dyspnea on moderate exertion, twopillow orthopnea, and mild ankle edema. On physical examination, his blood pressure is 144/85 mmHg, heart rate 64 bpm, and respiratory rate of 18. There is no jugular venous distension or gallop, but faint bibasilar rales are heard in both lung bases. His electrocardiogram (ECG) reveals nonspecific ST-T changes. A recent transthoracic echocardiogram reports an ejection fraction of 30% and mild impaired ventricular filling. A cardiologist recommends increasing the dose of diuretic, and places him at intermediate risk for perioperative cardiac events.
The patient undergoes the procedure a couple of days later under spinal anesthesia. There are no intraoperative complications, but he receives a total of 3 L of Ringer’s lactate. In addition, 10 L of glycine is used for irrigation, followed by intravenous furosemide. In the postanesthesia care unit, the patient is dyspneic, restless, and his Spo2 is 94% on 4 L of oxygen per minute. His heart rate is 100 bpm, and his blood pressure is 170/100 mm Hg. Rales are heard in both midlung fields. A chest radiograph shows redistribution of the vasculature and interstitial pulmonary edema. Supplemental oxygen is increased, and topical nitroglycerin and additional intravenous furosemide are administered, followed by brisk diuresis. He is then admitted to the intensive care unit (ICU). There are no electrocardiographic changes, and biomarkers for acute myocardial infarction are negative. The patient improves, and he is discharged from the ICU 24 hours later, following reinstitution of his chronic medications.
INTRODUCTION
Cardiovascular disease is currently the number one killer of men and women, claiming more lives than the next four leading causes of death combined.1 The epidemiologic and economic impact of cardiovascular diseases is further influenced by the current demographics and aging of our population, suboptimal implementation of disease-prevention strategies, and increase in the prevalence of risk factors for cardiac disease.
While the morbidity and mortality of patients with some acquired cardiovascular conditions, specifically post acute myocardial infarction, has declined, more patients are actually presenting in the endstages of their diseases with ventricular dysfunction and heart failure.
Heart failure is the final common pathway for all cardiac diseases, and represents one of the biggest epidemiologic challenges facing industrialized countries today.
In the perioperative period, heart failure has significant implications, both as a risk factor for adverse cardiac events following cardiac and noncardiac surgery,2,3 and as a complication from other processes such as ischemia, hypoxia, and fluid overload. There is a general belief that perioperative decompensated heart failure carries a poor prognosis.
What Is the Epidemiologic Impact of Heart Failure?
Improvements in the knowledge and care of conditions such as coronary artery disease (CAD), high blood pressure, diabetes mellitus, and alarming increasing rates of obesity have led to an increase in the prevalence of chronic heart failure (CHF).4 For example, there is an estimated 70% increase in heart failure due to CAD during the first decade of this century.5 In the past, the term “congestive” has been widely used to describe the syndrome, but current trends have recommended deleting such terminology because not all patients with heart failure exhibit signs and/or symptoms of volume overload.
In the United States and Europe, respectively, 5 and 10 million people carry a diagnosis of heart failure. Therefore, heart failure is one of the most common
conditions encountered in clinical medicine and a great public health care problem in developed countries.6,7 The precise epidemiology of CHF is elusive because the term “heart failure” has been used to describe a wide spectrum of clinical and pathophysiologic conditions, ranging from asymptomatic systolic and diastolic dysfunction to life-threatening acute pulmonary edema and cardiogenic shock.8
conditions encountered in clinical medicine and a great public health care problem in developed countries.6,7 The precise epidemiology of CHF is elusive because the term “heart failure” has been used to describe a wide spectrum of clinical and pathophysiologic conditions, ranging from asymptomatic systolic and diastolic dysfunction to life-threatening acute pulmonary edema and cardiogenic shock.8
CHF is not a primary condition but rather a multifactorial clinical syndrome, resulting from a structural or functional disorder that leads to poor myocardial performance. In the United States, CHF occurs as a complication from diseases such as coronary atherothrombosis, hypertension, and valvular heart disease, and less commonly from primary structural conditions such as cardiomyopathies.
CHF is predominately a condition of the elderly; with a prevalence estimated at 0.8% in the sixth decade, increasing dramatically to 10% in octogenarians.9 Approximately one half million new cases are diagnosed each year; these numbers are expected to rise due to the current trends of aging in our population and improvement in the treatment of other cardiovascular diseases.10 After age 40, the lifetime risk of developing heart failure is one in five for both men and women.1 Therefore, even if one estimates that only a small percentage of such patients will require surgery, it becomes clear that this represents a formidable epidemiologic challenge for perioperative physicians.
National guidelines in the United States for the diagnosis and management of CHF have been established and published. A new classification system was created in 2001, emphasizing risk factors and previous conditions that lead to heart failure, and the importance of early intervention before the clinical syndrome becomes manifest. This new classification scheme identifies four stages:11,12
STAGE A: Patients at risk for heart failure but without structural heart disease or signs or symptoms
STAGE B: Structural disease (e.g., old myocardial infarction, left ventricular hypertrophy) but no clinical signs/symptoms of heart failure
STAGE C: Structural disease with previous or current signs or symptoms of heart failure
STAGE D: Presence of end-stage heart failure that requires specialized interventions
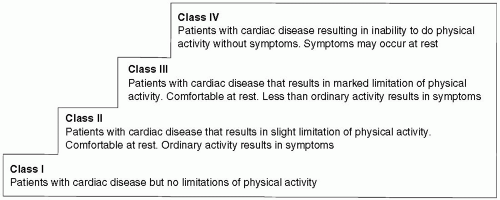
This classification is intended to complement the New York Heart Association (NYHA) functional capacity. The latter was initially proposed in 1928 to classify patients with heart disease based on severity of clinical symptoms, but suffers from several limitations such as being subjective, changing frequently over time, and not including patients in presymptomatic stages13,14 (see Fig. 16.1).
What Is the Importance and Impact of Acute Decompensated Heart Failure?
Current available information on acute decompensated heart failure (ADHF) is derived from a variety of sources and includes data on patients participating in clinical trials or registries and patients admitted to cardiology wards and ICUs; therefore, it should be interpreted with caution. Because ADHF encompasses a broad spectrum of clinical presentations and conditions, the term acute heart failure syndromes is occasionally used to describe the condition; a key factor to emphasize is the heterogeneity of the condition and its varied clinical, pathophysiologic, and prognostic implication. Although the terms, “acute” and “decompensated,” have been used to describe AHF, it is apparent that both are not the same. More descriptive terms found in the literature include new onset (de novo heart failure) and acutely exacerbated heart failure.15
For our purpose and simplicity of terms, we will consider ADHF as part of the overall syndrome of AHF. Literature on the syndrome of perioperative ADHF is rather scarce, and many issues remain unresolved. For example, it is currently unknown if ADHF in the setting
of noncardiac surgery actually has the same diagnostic, prognostic, and pathophysiologic implications as ADHF in the nonoperative setting. Additionally, in contrast with other conditions such as breast, prostate and colon cancer, there are currently no national screening efforts to detect ADHF at earlier stages.
of noncardiac surgery actually has the same diagnostic, prognostic, and pathophysiologic implications as ADHF in the nonoperative setting. Additionally, in contrast with other conditions such as breast, prostate and colon cancer, there are currently no national screening efforts to detect ADHF at earlier stages.
Overall, the information on ADHF is derived mainly from data in emergency departments and cardiology wards. In the United States, ADHF is one of the most significant causes for hospitalization. In the acute decompensated heart failure registry (ADHERE), the largest data base of heart failure cases in the United States, 78% of the patients enrolled come from the emergency department; the rest are from inpatient wards. It is clear that perioperative patients are underrepresented.16
Acute decompensated heart failure results from a rapid decrease in ventricular performance, tissue hypoperfusion, and, frequently, congestive symptoms. It is the primary cause of more than 1 million hospitalizations in the United States each year, and the most common reason for emergency department visits among the elderly.17,18 It is associated with significant mortality, 5% to 9.6% within the same hospital admission and 30% during the first year after the first hospitalization. Despite advances in therapy, it continues to be associated with a frequent need for hospital readmission. Readmission rates up to 50% after the first 6 months of hospital discharges have been documented.16
Although there is no universal definition on the condition, many classification systems are available in the literature.19,20,21,22 A rather simple and useful classification is provided by the European Society of Cardiology and is shown in Table 16.1. Despite the high prevalence of ADHF, the resulting economic burden, and associated high mortality, there are no published national guidelines for the diagnosis and management of ADHF.11 The outcome of ADHF is variable. Patients presenting with hypertension and pulmonary edema have a substantially better prognosis than those presenting in cardiogenic shock.23 In addition, asystolic blood pressure <115 mmHg, serum BUN >43 mg per dL, and creatinine >2.75 mg appear to be the best predictors of poor outcome.24
TABLE 16.1 Classification of Acute Heart Failure | |||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||
What Is the Epidemiologic Impact of Perioperative Heart Failure?
The epidemiology of ADHF in the perioperative setting remains poorly studied. The problem is compounded by arbitrary definitions of what constitutes acute perioperative heart failure. For example, Kumar et al. considered pulmonary edema a “severe” perioperative cardiac event, whereas worsening of heart failure and/or heart failure exacerbation without florid pulmonary edema were labeled “serious” events.25 Presently, it is unclear whether all cases of pulmonary edema carry the same prognostic implications, or if it is indeed worse to have pulmonary edema with rapid resolution versus a more protracted course of postoperative heart failure exacerbation without pulmonary edema.23,26
For the last three decades, it has been determined that CHF is a major risk factor for noncardiac and cardiac surgery.27,28 Despite the widespread notion that decompensated heart failure is considered a major clinical predictor, whereas compensated heart failure is considered an intermediate one, little is known about the fate of the patient with heart failure undergoing noncardiac surgery.29
Heart failure is not only a risk factor and predictor of other perioperative cardiac complications (e.g., myocardial infarction or arrhythmias), but the syndrome of heart failure by itself is considered a major complication.27,30,31,32,33,34,35 This is an important issue, because the number of patients with heart failure is increasing at an accelerated rate.
Preoperative guidelines are geared mainly for the evaluation and management of patients with CAD, but offer little or no guidance for clinicians to deal with patients at risk for perioperative heart failure.30,34,35 In fact, there is little evidence regarding the adequate evaluation, management, and outcome of patients with CHF undergoing noncardiac surgery. Hernandez et al. reported a statistically significant increase in the incidence of death and rehospitalization rate in a group of CHF patients undergoing noncardiac surgery when compared to a cohort of similar patients with CAD and another group of control patients. In his study, the reported operative mortality was 11.7% in heart failure cohort compared to 6.6% in the CAD group and 6.2% in the control group. Emphasizing the magnitude and the importance of the diagnosis of heart failure in the perioperative setting, once the patient had this diagnosis, the primary condition that led to ventricular dysfunction became less important than the diagnosis of heart failure.36
What Is the Overall Prognosis of Chronic Heart Failure?
Despite advances in the diagnosis and therapy of CHF, the prognosis remains poor. Currently, the prognosis
of CHF is worse than that of most cancers.37 Mortality remains high, with some studies reporting an overall 50% reduction of life expectancy in elderly patients with CHF compared with individuals without the condition.38 Data from the Framingham study reveals that survival of CHF patients at 5 years is only 25% for men and 38% for women; an overall one year survival was 57% in men and 64% in women, regardless of the etiology.39,40 The overall prognosis depends mainly on the underlying condition that leads to CHF in the presence of treatable precipitating factors and the response to therapy.
of CHF is worse than that of most cancers.37 Mortality remains high, with some studies reporting an overall 50% reduction of life expectancy in elderly patients with CHF compared with individuals without the condition.38 Data from the Framingham study reveals that survival of CHF patients at 5 years is only 25% for men and 38% for women; an overall one year survival was 57% in men and 64% in women, regardless of the etiology.39,40 The overall prognosis depends mainly on the underlying condition that leads to CHF in the presence of treatable precipitating factors and the response to therapy.
What Is the Pathophysiology of Chronic Heart Failure?
A simple working definition considers heart failure as a multisystem disorder with abnormalities of cardiac, skeletal muscle, and renal dysfunction.41 Early conception regarded heart failure as a syndrome caused by an abnormal “pump” mechanism unable to meet the metabolic requirements of the body (hemodynamic model) or as a syndrome with abnormal salt and water retention (cardio renal model).42 These concepts were subsequently expanded; it is now accepted that heart failure is a complex blend of structural, functional, neuroendocrine changes and compensatory responses that lead to abnormal ejection of blood (systolic dysfunction) or a predominant alteration in the filling of the heart (diastolic dysfunction). This results in a progressive clinical syndrome of fatigue, dyspnea, fluid retention, peripheral edema, and, in severe cases, pulmonary edema and hemodynamic shock. The underlying condition and predisposing factors may be cardiac or extracardiac, transient or permanent.
A key concept behind the current working theories on the pathophysiology of heart failure is that before this becomes clinically manifest, three main conditions must be met:
Intrinsic myocardial damage secondary to an insult or index event such as myocardial infarction or volume overload from valvular dysfunction
Activation of compensatory mechanisms in an attempt to correct the molecular, structural, and hemodynamic alterations
Myocardial remodeling, which modifies ventricular size, shape, and function.43
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree