CHAPTER 71 HAND FRACTURES
The presence of an opposable thumb separates man from other primates. The hand serves many functions, ranging from precise prehension to power gripping. This requires finely coordinated interplay among the various components of the musculoskeletal architecture of the hand. A stable and well-aligned skeletal framework, stable joints, and balance between intrinsic and extrinsic muscles and tendinous systems are all necessary for good hand function.
Most hand fractures can be treated nonoperatively by means of closed manipulation, splinting, and protected motion. Certain fracture patterns, however, are best treated by operative intervention. The goals of treatment remain the same and include accurate reduction, stabilization, wound treatment, and early mobilization. Inability to achieve or maintain reduction in the so-called safe or functional position denotes that a fracture is unstable. The fracture pattern and integrity of the periosteal sleeve and surrounding soft tissues determine fracture stability. Unopposed pull of muscles can lead to instability. Fractures involving articular surfaces demand accurate reduction to achieve good motion. Severely comminuted fractures are often best treated closed, because open reduction can lead to devitalization of small bony fragments. These fractures are well suited for closed pinning. Open fractures with loss of bone, contamination, or poor soft tissue coverage are best treated with external fixation. This permits fixation and maintenance of length while allowing for soft tissue healing and dressing changes. Definitive procedures to achieve bony union and soft tissue coverage can be carried out in a delayed fashion. Indications for operative treatment are summarized in Table 1.
Table 1 Indications for Operative Treatment in Hand Fractures
INCIDENCE
The most common upper extremity fractures are those of the metacarpals and phalanges. In a series of 4303 patients presenting to the emergency room with fractures, 19% had hand fractures.1 The phalanges were most commonly fractured. Males between the ages of 15 and 35 were most commonly injured. Fractures of the little finger ray were most common.
Hove, in a series of 1000 consecutive patients, found that metacarpals, phalanges, and carpal bones accounted for 36%, 46%, and 18% of the fractures, respectively.2 Chung and Spilson analyzed data from the 1998 National Hospital Ambulatory Medical Care Survey and estimated that in 1998, there were more than 600,000 metacarpal and phalangeal fractures in the United States.3
Fractures in children follow different patterns in various age groups because of differing mechanisms of injury. In a review of 242 hand fractures, Mahabir et al. found that 75% of injuries were in males, the mean age being 11 years.4 The incidence of fractures was very low in the very young, rose sharply at age 9, and peaked at 12 years. Forty percent were epiphyseal fractures, predominantly Salter-Harris II. The fifth metacarpal was the most frequently fractured bone.
The incidence of hand injuries in polytrauma was studied by Schaller and Geldmacher.5 They noted a 20% incidence of associated hand injuries, 75% of which were closed fractures. Ninety-three percent were involved in motor vehicle accidents.
MECHANISM OF INJURY
Chung and Spilson described the cause of injury in hand and forearm fractures.3 Forty-seven percent of injuries were due to falls, while 15% were due to being struck by a person or object. Ten percent were due to vehicular accidents. Other causes included being caught between objects, accidents involving machines or tools, injury due to another person, and nontraffic motor vehicle accidents.
De Jonge et al. studied the incidence and etiology of 6857 phalangeal fractures.6 They found that falls were responsible for most injuries in patients 70 years or older, while sports were the main cause in the age group 10–29 years. The highest incidence was in males aged 40–70 years, and the cause was machinery. Over 45% of hand fractures in children occurred either during sports or in a fight.
DIAGNOSIS
Management of hand injuries requires a good understanding of hand anatomy and biomechanics. The individual needs of the patient need to be taken into account before devising a treatment plan. A detailed history needs to be obtained. Key points to be elicited are noted in Table 2.
Table 2 History in Hand Injuries
METACARPAL FRACTURES
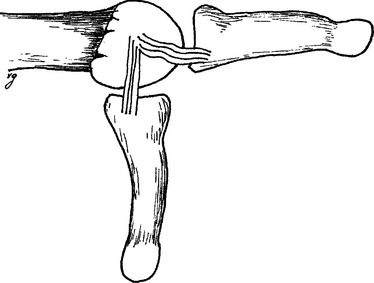
The metacarpals are structurally divided into the head, neck, shaft, and base. The metacarpal head articulates with the base of the proximal phalanx. The collateral ligaments between the metacarpal and phalanx arise in an eccentric position. Hence, these ligaments are stretched in flexion and lax in extension, and the joint is stable in flexion (Figure 1). The thumb metacarpal and fourth and fifth metacarpals are mobile. Because of its unique anatomy, thumb fractures are dealt with separately. Common metacarpal fracture patterns are illustrated in Figure 2.
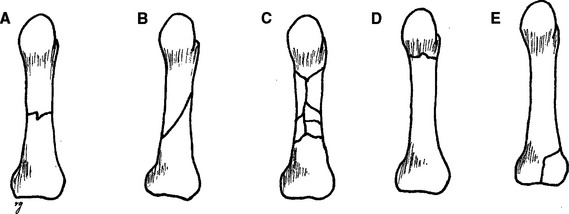
Figure 2 Common fracture patterns. (A) Transverse. (B) Spiral. (C) Comminuted. (D) Neck. (E) Intra-articular.
Metacarpal Shaft Fractures
Open reduction is indicated when the fracture is malaligned or unstable. Open fractures and those with associated soft tissue injuries are also best treated by open reduction. This permits earlier mobilization to prevent stiffness. With multiple metacarpal fractures, the stabilizing influence of the adjacent metacarpals is lost, and such fractures may need open reduction and internal fixation. Various techniques are available to stabilize fractures. Spiral or long oblique fractures can be stabilized by lag screws (Figure 3). The length of the fracture line should be at least twice the diameter of the bone. The proximal hole is overdrilled to a diameter wider than the thread of the screw. As the screw is tightened and the threads grip the distal fragment, interfragmentary compression is achieved.

Figure 3 (A) Metacarpal shaft fracture sustained in a fist fight. (B) Fixation with three lag screws.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree