124 Gynecologic Pain and Vaginal Bleeding
• The possibility of pregnancy should be considered in every patient with a chief complaint of vaginal bleeding or pelvic pain.
• Ectopic pregnancy, acute appendicitis, and ovarian torsion must be considered in female patients with acute pelvic pain.
• Up to 50% of patients with ovarian torsion have normal findings on ultrasound.
• Malignancy should be considered in postmenopausal women with new-onset vaginal bleeding.
• With the exception of physiologic withdrawal bleeding in the neonate, vaginal bleeding in a prepubescent girl is always abnormal.
Vaginal Bleeding
Epidemiology
Dysfunctional Uterine Bleeding
DUB affects an estimated 30% of women in the United States, is most common at the extremes of the reproductive years, and has no predilection for race. DUB rarely causes mortality but is accountable for two thirds of all hysterectomies and the majority of endoscopic endometrial destructive surgery.1
Uterine Leiomyomas (Fibroids)
Uterine leiomyomas (fibroids) are the most common pelvic tumor in women and have been noted on pathologic examination in approximately 80% of surgically excised uteri.2 Risk factors include African American race, early menarche (<10 years of age), nulliparity, and family history. Several studies have shown more subtle correlations with obesity and diet.3,4
Endometrial Cancer
Endometrial cancer is the fourth most common cancer in women and occurs in approximately 25 per 100,000 women.5,6 This malignant disease develops during the reproductive and menopausal years, with most patients being 50 to 59 years of age. About 5% of women younger than 40 have adenocarcinoma, and it is diagnosed in a quarter of patients before menopause. Many cases of endometrial cancer go undetected given that Papanicolaou smears detect only 50% of cases and the diagnosis is rarely considered in perimenopausal women despite the aforementioned statistics.
Cervical Cancer
Cervical cancer is the second most common malignancy in women worldwide. Approximately 11,000 new cases are diagnosed annually in the United States, and it accounts for around 4000 deaths per year. Minority populations are more commonly affected. The peak incidence of cervical cancer occurs in women 45 to 54 years of age; however, there is a surge in prevalence in women in their 20s and 30s as human papillomavirus (HPV) rates have increased.5,6
Pathophysiology
Common terminology and definitions for vaginal bleeding are listed in Box 124.1. An understanding of the normal female reproductive cycle is useful when caring for patients with vaginal bleeding and pelvic pain. The normal reproductive cycle is 28 days, with a range of 21 to 35 days, and the average age at menarche is approximately 12.5 years. The complex hormonal feedback mechanism that governs the female reproductive cycle is controlled by the hypothalamic-pituitary-ovarian (HPO) axis. Days 1 to 14 are known as the follicular or proliferative phase and are dominated by the release of gonadotropin-releasing hormone (GnRH) from the hypothalamus; GnRH in turn stimulates pituitary release of follicle-stimulating hormone (FSH). During this phase a dominant ovarian follicle matures and produces estrogen, which causes the endometrium to thicken and prepare for possible embryo implantation. Positive feedback of estrogen to the pituitary gland induces a surge in luteinizing hormone (LH) on day 14 of the cycle, which results in ovulation. Days 14 to 28 are known as the luteal or secretory phase; this phase is predominated by progesterone production from the corpus luteum, which induces maturation of the endometrium. If conception and implantation do not occur, the corpus luteum involutes, estrogen and progesterone levels fall, and menstruation occurs.
Disruption at any point in this feedback loop may cause pelvic pain or abnormal vaginal bleeding.
Dysfunctional Uterine Bleeding
DUB is the most common cause of menorrhagia in menstruating females and is defined as abnormal uterine bleeding in the absence of organic disease. DUB can be ovulatory or anovulatory. Ovulatory DUB is hallmarked by regular intervals of increased menstrual flow. The root cause is an abnormality in uterine hemostasis secondary to cytokine and prostaglandin production. More commonly (accounting for 90% of cases of DUB), anovulatory DUB is hallmarked by irregular intervals of alternating heavy and light flow. This can be caused by primary ovarian disorders or a disruption in the HPO axis.7
Uterine Leiomyomas (Fibroids)
The disease process just described generally occurs in the fourth decade of life and usually abates after menopause. Approximately 10% to 40% of fibroids will regress over a period of 6 months to 3 years, and almost all symptomatology will abate at the time of menopause because these uterine tumors are estrogen sensitive. With the use of postmenopausal hormone replacement therapy, however, symptoms may continue past the cessation of menses.8,9
Cervical Cancer
Risk factors for cervical cancer are strongly correlated with sexual activity and include multiple sexual partners, early age at first coitus, early pregnancy, and previous history of sexually transmitted diseases. All these risk factors increase exposure to HPVs, which have been implicated as a major risk factor for the development of cervical cancer and high-risk lesions.10
Presenting Signs and Symptoms
Differential Diagnosis and Medical Decision Making
The most common causes of abnormal vaginal bleeding in nonpregnant patients are DUB and uterine leiomyomas. Tables 124.1 and 124.2 list the differential diagnosis of vaginal bleeding in nonpregnant females. Figure 124.1 details an approach to patients seen in the emergency department (ED) with the complaint of vaginal bleeding.
Table 124.1 Common Terminology and Definitions
| TERMINOLOGY | DEFINITION |
|---|---|
| Amenorrhea | Cessation of menses for >6 mo |
| Dysmenorrhea | Pain associated with menses |
| Hypomenorrhea | Menstrual volumes < 20 mL/cycle |
| Menorrhagia | Menses > 80 mL/cycle or occurring for >7 days |
| Metrorrhagia | Vaginal bleeding between menstrual cycles or irregular cycles |
| Menometrorrhagia | Prolonged or heavy bleeding at irregular intervals |
| Oligomenorrhea | Decreased frequency of cycles (>35 days per cycle) |
| Polymenorrhea | Increased frequency of cycles (<21 days per cycle) |
| Postmenopausal bleeding | Bleeding 6-12 mo after menopause |
Table 124.2 Systemic Causes of Abnormal Vaginal Bleeding
| CAUSE | MECHANISM |
|---|---|
| Weight loss Stress Excessive exercise | Hypothalamic suppression of GnRH |
| Polycystic ovarian disease | Excessive estrogen effects on the endometrium Anovulatory cycles |
| Hypothyroidism | Anovulatory cycles |
| Hyperthyroidism | Changes in androgen and estrogen production |
| Hyperprolactinemia (prolactinoma) | Mass effect on the pituitary stalk reduces GnRH secretion |
| Liver failure | Decreased production of vitamin K–dependent clotting factors Increased estrogen levels secondary to decreased metabolism |
| Renal failure | Inherent platelet dysfunction |
| Platelet dysfunction | |
| Cushing disease | Mass effect on the pituitary stalk reduces GnRH secretion Decreased LH, FSH function |
FSH, Follicle-stimulating hormone; GnRH, gonadotropin-releasing hormone; LH, luteinizing hormone.
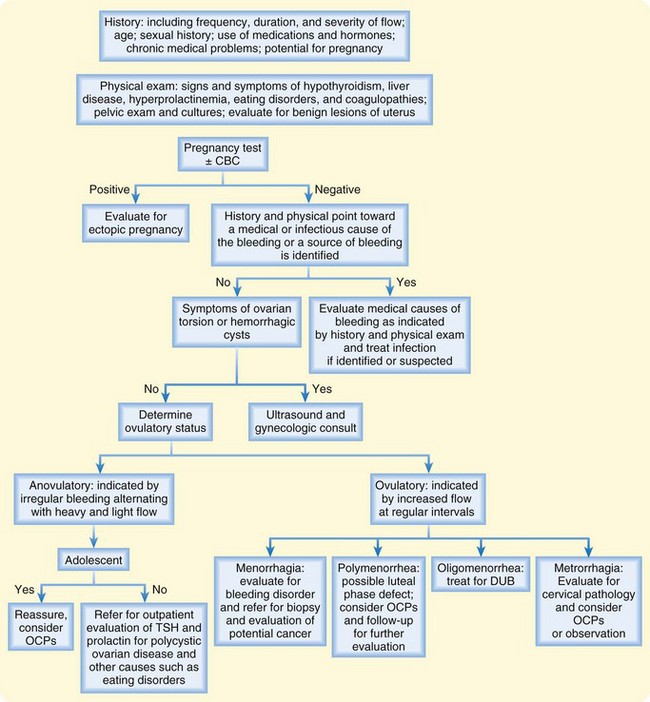
Fig. 124.1 Algorithm outlining an approach to patients with abnormal vaginal bleeding.
CBC, Complete blood count; OCPs, oral contraceptive pills; TSH, thyroid-stimulating hormone.







