CHAPTER 56 GYNECOLOGIC INJURIES
TRAUMA IN PREGNANCY
In recent years, trauma has been recognized as the leading cause of death during pregnancy. As unsuspected pregnancy is relatively common in the reproductive years, this possibility must be considered when evaluating female trauma victims. Pregnancy produces significant physiologic and anatomic changes that must be recognized and understood by all health care providers treating pregnant trauma patients (Table 1).
Table 1 Changes in Maternal Physiology during Pregnancy
| Change | Consequence |
|---|---|
| Cardiac output and blood volume increase | Shock after >40% of blood lost |
| Expansion of plasma volume | Physiologic anemia |
| Decline in arterial and venous pressure | Vital signs are not reflective of hemodynamic status |
| Increase of resting pulse | |
| Chest enlargement | Change in anatomic landmarks |
| Caution during thoracic procedures (e.g., thoracostomy) | |
| Diaphragm rise | |
| Substernal angle increase | |
| Decrease in functional residual capacity | Rapid decline in PO2 during apnea or airway obstruction |
| Increase in oxygen consumption | |
| Airway closure when supine | |
| Increase in tidal volume and minute ventilation | Fall in PCO2 and bicarbonates |
| Decrease in anesthetic requirements | Need for adjustment of sedative doses |
| Decreased gastric motility | Risk of aspiration |
| Relaxation of gastroesophageal sphincter |
Diagnosis
Prehospital Care
As a result of significant changes in maternal physiology (see Table 1), supplemental oxygen should be administered to prevent maternal and fetal hypoxia during transport and in the resuscitation room. Fluid resuscitation should be initiated even in the absence of signs of hypovolemia and shock. To avoid supine hypotension associated with the uterine compression of the inferior vena cava (IVC), patients in the second or third trimester of pregnancy should be transported on a backboard tilted to the left, with special attention to immobilization of the cervical spine. If the patient is kept in a supine position, the right hip should be elevated 4–6 inches, and the uterus should be displaced manually to the left. This maneuver increases cardiac output by 30% and restores circulating blood volume. Although only about 10% of pregnant patients at term develop symptoms of shock in the supine position, fetal distress may be present even in normotensive mothers; therefore, right hip elevation should be maintained at all times including during operative procedures.
Hospital Care
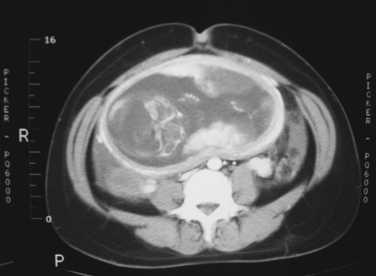
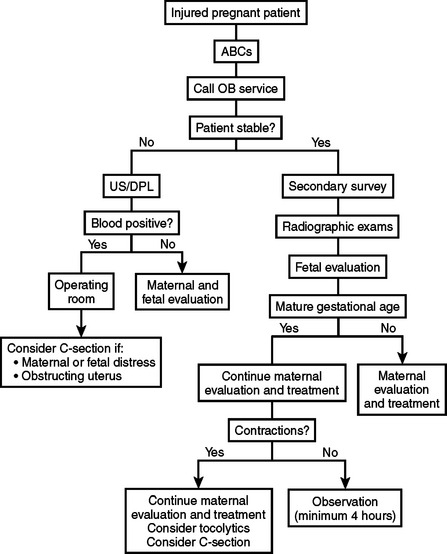
Determination of gestational age is particularly important because this will guide the decision for a premature delivery if indicated. Most institutions will accept a 24–26 week pregnancy as viable, with a probability of survival ranging from 20%–70%. Radiographic estimation of gestational age is bound to an error of 1–2 weeks. Unless the date of the conception is known exactly, gestational age is particularly difficult to determine. A good rule of thumb is to consider patients with a uterus halfway between the umbilicus and the costal margin as having a viable pregnancy (Figure 1). An algorithm for initial maternal and fetal assessment is presented in Figure 2.
Bulging perineum
This is caused most commonly by pressure from extrauterine location of fetal parts.
Abnormal fetal heart rate and rhythm
An abnormal fetal heart rate may be the first indication of a major disruption in fetal homeostasis. During trauma resuscitation, evaluation of the fetus should begin with auscultation of heart tones and continuous electronic fetal heart rate monitoring (EFM). Any viable fetus of 24 or more weeks gestation requires monitoring after trauma. Cardiotocographic monitoring should be started in the resuscitation room and continued for a minimum of 4 hours; a minimum of 24 hours is recommended for patients with frequent uterine activity (more than six contractions per hour), abdominal or uterine tenderness, ruptured membranes, vaginal bleeding, or hypotension.
Radiographic Examination
Although there is existing concern about radiation exposure during pregnancy, in most instances the benefits outweigh the risks. It is generally believed that exposure of the fetus to less than 5–10 rad causes no significant increase in the risk of congenital malformations, intrauterine growth retardation, or miscarriage. Radiation doses from common imaging studies are shown in Table 2. All indicated radiographic studies should be performed, as for nonpregnant patients (Figure 3). It is obvious that unnecessary duplication of studies should be avoided.
Table 2 Radiation Doses from Plain Radiographs and CT
| Plain anteroposterior chest x-ray | <0.005 rad |
| Pelvic x-ray | <0.4 rad |
| CT scan of head (1-cm cuts) | 0.05 rad |
| CT scan of upper abdomen (20 1-cm cuts) | 3.0 rad |
| CT scan of lower abdomen (10 1-cm cuts) | 3.0–9.0 rad |
CT, Computed tomography.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree