Genomic Basis of Perioperative Medicine
Human biologic diversity involves interindividual variability in morphology, behavior, physiology, development, susceptibility to disease, and response to stressful stimuli and drug therapy (phenotypes) (Friede K, Mathew JP, Podgoreanu MV. Genomic basis of perioperative medicine. In: Barash PG, Cullen BF, Stoelting RK, Cahalan MK, Ortega R, Stock MC, eds. Clinical Anesthesia. Philadelphia: Lippincott Williams & Wilkins; 2013: 130–155). Phenotypic variation is determined, at least in part, by differences in the specific genetic makeup (genotype) of an individual.
I. Scientific Rationale for Perioperative Genomic Medicine
Genomic medicine proposes to use genomic information to assist medical decision making and tailor health care to the individual patient. Dramatic improvements in sequencing technologies and cost reductions are the stimuli to pursue creation of personalized medicine research.
Many common diseases, such as atherosclerosis, coronary artery disease, hypertension, diabetes, cancer, and asthma, and many individual responses to injury, drugs, and nonpharmacologic therapies are genetically complex, characteristically involving an interplay of many genetic variations in molecular and biochemical pathways.
The perioperative period represents a unique and extreme example of gene–environment interaction.
A hallmark of perioperative physiology is the striking variability in patient responses to the perturbations induced by events occurring in the operative period.
This translates into substantial interindividual variability in immediate perioperative adverse events (e.g., mortality, incidence, or severity of organ dysfunction), as well as long-term outcomes (Table 6-1).
Genetic variation is partly responsible for the observed variability in outcomes.
With increasing evidence suggesting that genetic variation can significantly modulate the risk of adverse perioperative events, the emerging field of perioperative genomics aims to apply
functional genomic approaches to discover underlying biologic mechanisms.
These approaches explain why similar patients have such dramatically different outcomes after surgery. These outcomes are determined by a unique combination of environmental insults and postoperative phenotypes that characterize surgical and critically ill patient populations.
To integrate this new generation of genetic results into clinical practice, perioperative physicians need to understand the patterns of human genome variation, the methods of population-based genetic investigation, and the principles of gene and protein expression analysis.
Table 6-1 Categories of Perioperative Phenotypes | ||||
|---|---|---|---|---|
|
II. Overview of Human Genetic Variation
Although the human DNA sequence is 99.9% identical among individuals, the variations may greatly affect a person’s disease susceptibility.
Rare genetic variants (mutations) are responsible for more than 1,500 monogenic disorders (e.g., hypertrophic cardiomyopathy, long-QT syndrome, sickle cell anemia, cystic fibrosis, familial hypercholesterolemia).
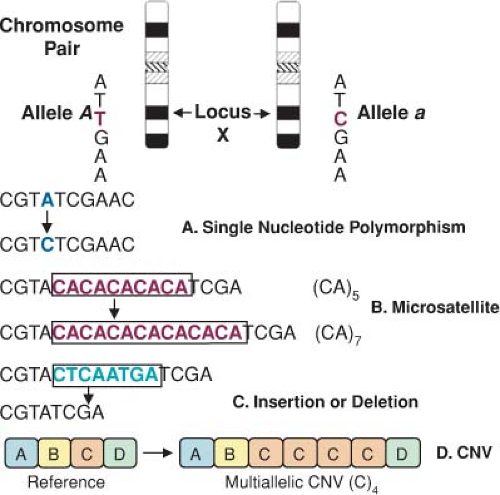
Most of the genetic diversity in the population is attributable to more widespread DNA sequence variations (polymorphisms), typically single nucleotide base substitutions (single nucleotide polymorphisms [SNPs]) (Fig. 6-1).
About 15 million SNPs are estimated to exist in the human genome, approximately once every 300 base pairs, located in genes as well as in the surrounding regions of the genome.
Polymorphisms may directly alter the amino acid sequence and therefore potentially alter protein function or alter regulatory DNA sequences that modulate protein expression.
Sets of nearby SNPs on a chromosome are inherited in blocks, referred to as haplotypes.
The year 2007 was marked by the realization that DNA differs from person to person much more than previously suspected.
III. Methodologic Approaches to Studying the Genetic Architecture of Common Complex Diseases
Most ongoing research on complex disorders focuses on identifying genetic polymorphisms that enhance susceptibility to given conditions (e.g., candidate gene and genome scans used to identify polymorphisms affecting common diseases).
Linkage analysis is used identify the chromosomal location of gene variants related to a given disease by studying the distribution of disease alleles in affected individuals throughout a pedigree. The nature of most complex diseases (especially for perioperative adverse events) precludes the study of extended multigenerational family pedigrees.
Genetic association studies examine the frequency of specific genetic polymorphisms in a population-based sample of unrelated diseased individuals and appropriately matched unaffected control participants. The fact that these studies do not require family-based sample collections is the main advantage of this approach over linkage analysis.
Accumulating evidence from candidate gene association studies also suggests that specific genotypes are associated
with a variety of organ-specific perioperative adverse outcomes (myocardial infarction [MI], neurocognitive dysfunction, renal compromise, vein graft restenosis, postoperative thrombosis, vascular reactivity, severe sepsis, transplant rejection, death).
Replication of findings across different populations or related phenotypes remains the most reliable method of validating a true relationship between genetic polymorphisms and disease.
The year 2007 marked the publication of adequately powered and successfully replicated genome-wide association studies that identified significant genetic contributors to the risk for common polygenic diseases (coronary artery disease, MI, types I and II diabetes, atrial fibrillation, obesity, asthma, common cancers, rheumatoid arthritis, Crohn’s disease).
Variants in or near CDKN2A/B (cyclin-dependent kinase inhibitor 2 A/B) have been shown to confer increased risk for both type II diabetes and MI, which may lead to a mechanistic explanation for the link between the two disorders.
IV. Large-Scale Gene and Protein Expression Profiling: Static Versus Dynamic Genomic Markers of Perioperative Outcomes
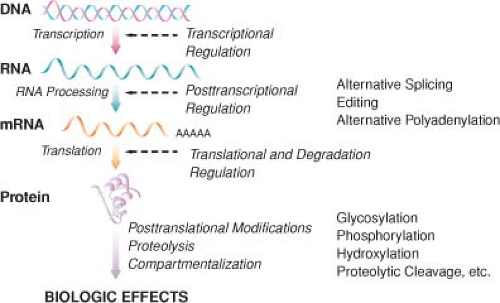
Genomic approaches are anchored in the concept of transcription of messenger RNA (mRNA) from a DNA template followed by translation of RNA into protein (Fig. 6-2).
Transcription is a key regulatory step that may eventually signal many other cascades of events.
Although the human genome contains only about 25,000 genes, functional variability at the protein level is far more diverse, resulting from extensive posttranscriptional, translational, and posttranslational modifications.
It is believed that there are approximately 200,000 distinct proteins in humans, which are further modified posttranslationally by phosphorylation, glycosylation, oxidation, and disulfide structures.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree