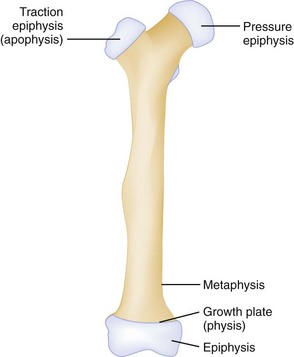
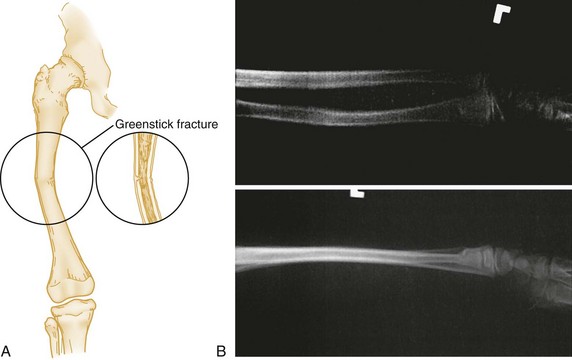
Chapter 49 1. Most orthopedic injuries can be predicted by understanding the chief complaint, the age of the patient, the mechanism of injury, and an estimate of the amount of energy delivered. 2. A careful history and physical examination predict radiographic findings with a high degree of accuracy. A presumptive diagnosis before a radiographic study may prompt the physician to order special views necessary to correctly diagnose an injury. Many fractures were accurately described before the advent of roentgenology (Table 49-1). Table 49-1 Common Fracture Names and Their Origins 3. If a fracture is suggested clinically, but radiographic films appear negative, the patient should initially be treated with immobilization as though a fracture were present. 4. Criteria for adequate radiographic studies exist; inadequate studies should not be accepted. 5. Radiographic studies should be performed before most reductions are attempted, except when a delay could be potentially harmful to the patient or in some field situations. 6. Neurovascular competence should be checked and recorded before and after all reductions and after application of immobilization. 7. Patients must be checked for the ability to safely ambulate before discharge from the ED and should not be discharged unless this can be established. 8. Patients should receive explicit aftercare instructions before leaving the ED, covering such areas as monitoring for signs of neurovascular compromise or increasing compartment pressure, cast care, weightbearing, crutch use, and an explicit plan and timing for follow-up. 9. In a patient with multiple trauma, noncritical orthopedic injuries should be diagnosed and treated only after more threatening injuries have been addressed. 10. All orthopedic injuries should be described precisely and according to established conventions. When communicating with an orthopedic consultant, this may affect decisions regarding disposition of a patient and operative versus nonoperative management. Describing orthopedic injuries with precise language according to established convention enables accurate, clear communication with other parties. Terms commonly used to describe a fracture are listed in Box 49-1. A fracture is a break in the continuity of bone or cartilage. Clinically, a history of loss of function, pain, tenderness, swelling, abnormal motion, and deformity suggests a fracture. Radiographic studies are the mainstay of diagnosis and are usually, although not always, confirmatory. At times, use of special views, radionuclide bone scans, computed tomography (CT), or magnetic resonance imaging (MRI) is necessary to confirm a clinical impression. These studies should be considered when the clinical evidence is at odds with the findings of routine radiography. An additional modifier describes the direction of the fracture line in relation to the long axis of the bone in question. A transverse fracture occurs at a right angle to the long axis of the bone (Fig. 49-1A), whereas an oblique fracture runs oblique to the long axis of the bone (Fig. 49-1B). A spiral fracture results from a rotational force and encircles the shaft of a long bone in a spiral fashion (Fig. 49-1C). A fracture with more than two fragments is termed comminuted (Fig. 49-1D). The position and alignment of the fracture fragments (i.e., their relationship to one another) should be described. Fragments are described relative to their normal position, and any deviation from normal is termed displacement. By convention, the position of the distal fragment is described relative to the proximal one. Displacement may be described as a quantitative measurement (i.e., in millimeters) or as a percentage of the bone width. Figure 49-2 shows a dorsal displacement of the fractured radius, and Figure 49-3 shows lateral, or valgus, displacement of the distal tibia and fibula. The terms valgus and varus are sometimes confusing. Valgus denotes a deformity in which the described part is angled away from the midline of the body. Conversely, varus denotes a deformity in which the angulation of the part is toward the midline. Alignment refers to the relationship of the longitudinal axis of one fragment to another; deviation from the normal alignment is termed angulation. The direction of angulation is determined by the direction of the apex of an angle formed by the two fracture fragments (Fig. 49-4). This angle is opposite to the direction of displacement of the distal fragment. The relative position or angulation of the distal fragment of a fracture may also be described with terms such as radial or ulnar, dorsal or volar, anterior or posterior, and lateral or medial. One should also be aware of rotational deformity, present when the distal fragment of a fracture is rotated to some degree along the axis of the bone itself. Especially in the digits of the hand, radial or ulnar deviation of a flexed finger can occur, and radiographs often underestimate the degree of clinical deformity and rotation present. Avulsion fracture refers to a bone fragment that is pulled away from its normal position by either the forceful contraction of a muscle (Fig. 49-5A) or the resistance of a tendon or ligament to a force in the opposite direction (Fig. 49-5B). Impaction refers to the forceful collapse of one fragment of bone into or onto another. In the proximal humerus, this collapse typically occurs in a telescoping manner, particularly in elderly patients, whose bones are soft and brittle. In the tibial plateau, impaction occurs frequently in the form of a depression (Fig. 49-6A and B), and in the vertebral bodies, impaction frequently occurs in the form of compression (Fig. 49-6C). A fracture that occurs through abnormal bone is termed pathologic. A pathologic fracture is suggested whenever a fracture occurs from seemingly trivial trauma. Diseases that cause structural weakness predisposing to injury include primary or metastatic malignancies, cysts, enchondromata, and giant-cell tumors. In addition, osteomalacia, osteogenesis imperfecta, scurvy, rickets, and Paget’s disease all weaken bones, making them susceptible to fracture. The term pathologic also is applied to fractures through osteoporotic bone when the demineralization is a result of disease, as in polio. Fractures through osteoporotic bone of the elderly usually are not described as pathologic. When fractures occur in normal bones and a history of “trivial trauma” is elicited, violence or battering should be suspected. Repeated low-intensity forces may lead to resorption of normal bone, resulting in a stress fracture. Other names for this condition are fatigue fracture and march fracture (see Table 49-1). Most stress fractures occur in the lower extremities and commonly affect individuals involved in activities such as running, basketball, aerobics, and dancing. Extrinsic factors such as training regimens, type of equipment used, and nutrition habits, as well as intrinsic factors such as anatomic variation, muscle endurance, and hormonal factors have all been associated with stress fractures. These injuries may not be recognizable on initial plain films; therefore management should be based on clinical diagnosis.1 The tibia, fibula, metatarsals, navicular, cuneiform, calcaneus, femoral neck, or femoral shaft may be involved.2,3 Many fractures were described before the advent of radiography and are described by an eponym rather than the exact bony injury. These eponyms reflect the rich history of orthopedic care and, despite the objections of some, are still commonly used to describe orthopedic injuries (see Table 49-1). Certain features of children’s bones distinguish pediatric fractures from adult fractures. Bones of children are necessarily soft and resilient and sustain numerous incomplete fractures. Greenstick fractures are incomplete angulated fractures of long bones. The resultant bowing of the bone causes an appearance resembling a moist, immature branch that breaks in a similar fashion when bent (Fig. 49-7A). A torus fracture is another form of incomplete fracture, characterized by a wrinkling or buckling of the cortex. In Greek architecture a torus is a bump at the base of a column, and these fractures, occurring at the end of long bones, take on such an appearance. These fractures may be extremely subtle on radiographs (Fig. 49-7B). Figure 49-7 A, Greenstick fracture of midshaft of femur. B, Torus fracture of distal third of radius. Another feature of growing long bones that is a frequent source of trouble and confusion is the presence of epiphyses, cartilaginous centers at or near the ends of bone that give rise to growth of the bone. Figure 49-8 is a schematic review of the anatomy of a growing bone. Because cartilage is radiolucent, the cartilaginous portion of an epiphysis is not visualized on radiographs. A tendency exists to consider only the ossified nucleus and to ignore the cartilaginous structure that bridges to the metaphysis. Cartilage is present even before an ossified nucleus is seen. Because the epiphyseal growth plate is represented by a radiolucent line, confusion may exist as to whether a fracture line is present. These complexities in interpreting radiographs in children sometimes, but not always, require comparison radiographic views of the uninjured side. Injuries to the epiphyses may result from either compressive or shearing forces. These injuries are relatively common during childhood as opposed to sprains or shaft fractures and should be considered in children with a “sprained ankle” because of the relative weakness of the cartilaginous growth zone, which separates before stronger ligaments and bones are torn or broken. Epiphyseal injuries should be described according to the Salter-Harris classification (Table 49-2). Type II injuries are similar to type I injuries, with a fracture extending into the metaphysis. The triangular metaphyseal fragment sometimes is referred to as the Thurston Holland sign (see Table 49-1). Type II injuries account for approximately three fourths of all epiphyseal fractures. Because the germinal layer is not involved, growth disturbance usually does not occur with type I and II injuries. These injuries are amenable to closed reduction and immobilization without internal fixation. Type V fractures are crush injuries of the epiphyseal plate, usually produced by a compressive force.3 This type of injury usually occurs in joints that move in one plane, most commonly the knee and ankle. Because this injury occurs in a radiolucent area, the injury may be difficult to diagnose on radiograph, but it is suggested by mechanism of injury and pain over the epiphysis. The diagnosis can be established by MRI if hemorrhage or a hematoma is identified within the growth plate immediately after injury.3–5 Also reported is loss of MRI signal from the cartilage.6 Rarely are type V injuries diagnosed acutely, and growth arrest manifested by shortening or angulation is the rule with this injury. Physeal injuries occur twice as often in boys as in girls and are most common in boys aged 12 to 15 years and in girls aged 9 to 12 years.7 Distal physes are injured more often than proximal physes, and the most common anatomic locations include the distal radius, phalanges, and distal tibia. Distal radius fractures account for two thirds of fractures in pediatric patients in the ED.8 The incidence of these fractures has increased by 40% over the past three decades, possibly because of a change in recreational activities, such as increased skiing and skating among boys and increased basketball, soccer, and skating among girls.9 Most distal radius type I and II fractures can be treated through closed reduction, though this may be more technically difficult with completely displaced both-bone fractures. Similar practice has been applied to distal tibia type I and II fractures, though the incidence of premature physeal closure was shown to be 3.5 times higher if the residual fracture displacement was greater than 3 mm in postreduction radiographs.10 Growth arrest as a complication of physeal fracture is most likely to be seen at the distal femur, distal and proximal tibia, and distal radius.7 Stress views of joints are used in some instances to evaluate the degree of ligamentous injury. Some authors argue against the use of stress views, citing a risk of further injuring an already traumatized structure, additional radiation exposure to the patient and the technologist, and the possibility that pain may not allow sufficient stress to be applied. For these reasons, stress views should be used judiciously in circumstances when other methods of evaluating ligamentous injuries are not available. Comparison views are useful in selected situations but should not routinely be performed in all pediatric examinations.11 If a fracture is definitely present on the affected side, the comparison view exposes the child to radiation and adds expense with no benefit. Similarly, an experienced physician generally is able to read a normal film with reasonable certainty. It is reasonable to use comparison views in instances when radiographs are inconclusive and when the confusion arises specifically out of the need to distinguish between a possible fracture and normal developmental anatomy. Obtaining a wide field of the affected extremity is more useful than routine comparison views for a young child because the child often does not localize the pain well; this is especially true with regard to complaints of knee pain in cases of hip injury or wrist complaints in forearm and elbow injury. Comparison views sometimes are helpful in adults when a question of accessory ossicles or nonfused bones (e.g., bipartite patella) exists because these anomalies are usually bilateral. The bleeding that inevitably accompanies fractures may produce soft tissue swelling, which may impinge on or obliterate overlying muscle planes. Fat pads, such as in the elbow, may be displaced. Another useful sign is the fat-fluid level, which may accompany fractures extending into the knee joint. The fat-fluid level is visible, however, only if the cross-table technique is used. The bones themselves should be examined systematically. Normal adult bones possess a smooth unbroken contour. A distinct angle is highly suggestive of a fracture. In an adult the typical fracture is represented by a lucent line that interrupts the smooth contour and usually extends to the opposite side. Nutrient arteries may be confused with fractures but have different radiographic characteristics: They are fine, are sharply marginated, extend obliquely through the cortex, and are less radiolucent than fractures. Pseudofractures can be created by soft tissue folds, bandages or other overlying material, or a radiographic artifact called the Mach effect. If lucencies extend beyond the bones, the line is highly unlikely to represent a fracture. Anomalous bones and calcified soft tissue likewise may be mistaken for fractures. Avulsions and small fracture fragments have an irregular surface that lacks well-corticated margins and a defect in the adjacent bone is present, whereas anomalous ossification centers (accessory ossicles) and sesamoids are characterized by smooth cortical margins. Reference texts are useful in identifying and confirming these anomalies because they tend to occur in predictable locations.12 Compression fractures are represented by increased density rather than a lucency. Finally, the most commonly missed fracture is the second fracture. One should be diligent in searching for additional fractures after discovering the first fracture on a study. In particular, certain paired fractures, such as the distal tibia and proximal fibula, should be sought out. Radionuclide Bone Scanning.: In the past, radionuclide bone scanning was used to detect skeletal abnormalities not radiographically evident in children and adults.13 Occult lesions, especially stress fractures, acute osteomyelitis, and tumors, can be detected on these scans, although there are problems with specificity and sensitivity. This modality has been largely supplanted by CT and MRI and now is seldom used. Computed Tomography.: Computed (digital) radiography is now in widespread use. Although conventional radiography remains the initial imaging study of choice for skeletal trauma, CT offers a more detailed and diagnostically sensitive evaluation of bones and joints. With improved resolution and speed, multidetector-row CT captures large volumetric data sets from which two- and three-dimensional images can be created.14,15 Workstation postprocessing has become an integral part of the examination. Two-dimensional multiplanar reconstruction in any chosen plane, and three-dimensional surface rendering techniques provide images with unprecedented quality, even in the presence of metallic implants or fixation devices.16 CT is used to confirm possible fractures or to better define displacement, alignment, or fragmentation of fractures. It is also useful in trauma to rule out cervical spine fracture when plain films are equivocal and in noncompressive vertebral fractures to assess the number of fragments and their spatial relationship to the spinal canal. CT is used frequently to define the integrity of articular surfaces in the acetabulum, knee, wrist, or ankle and in Salter-Harris type IV fractures.4 In the multiple trauma patient requiring thoracic, abdominal, and pelvic CT imaging to rule out visceral injury, the soft tissue protocols may be adapted to acquire diagnostic bone images, as well.17 During imaging of the chest, abdomen, or pelvis, data sets are created from which the thoracolumbar spine and bony pelvis can be derived. Magnetic Resonance Imaging.: MRI constitutes the most advanced noninvasive examination of orthopedic structures, delineating lesions of bone, cartilage, ligaments, and other structures, such as menisci, disks, and epiphyseal structures. MRI is expensive and time-consuming and should be reserved for instances in which the diagnosis is in doubt and specific findings would alter the treatment. Ultrasound Imaging.: Point-of-care ultrasound may be an effective tool for the diagnosis of fractures when conventional radiography is unavailable. Through use of bedside ultrasonography, fractures are visualized as an interruption of the linear bony cortex and may be clinically correlated during the physical examination of the affected area. Ultrasound can be effective in the diagnosis of long bone fractures, orbital floor fractures, rib fractures, and occult fractures of the foot and ankle.18 Ultrasound can be used in “real-time” during fracture reduction to confirm proper reduction and alignment of bony fragments.19 Any fracture communicating with the surface of the skin is termed an open fracture. Open fractures are treated as true orthopedic emergencies because of the risk of infection; the dreadful nature of the complication of osteomyelitis dictates that no time should be wasted in initiating therapy (Box 49-2). Wounds should be irrigated of gross debris and covered with a sterile dressing, and parenteral antibiotics should be instituted as early as possible.20 Currently, suggested therapy includes a first-generation cephalosporin, such as cefazolin, for all open fractures, with the addition of an aminoglycoside for grade II or III fractures.21,22 Early versus delayed treatment of open fractures and its subsequent effect on rates of infection has been a source of debate. Historic guidelines recommending débridement of open fracture wounds within 6 hours of injury were based on animal experiments conducted in the 1890s.23 Current human studies suggest no clear advantage to performing surgical débridement within 6 hours of injury. The timing of débridement—less than 6 hours versus more than 6 hours after injury—had no effect on clinical or functional outcome in a prospective multicenter study of severe lower-extremity fractures.24 Other retrospective studies and literature reviews advocate early débridement and irrigation of the wound within the first 24 hours of injury to prevent infection. Certain open fractures of the finger present a notable exception to the previous recommendation. Such injuries, especially an open distal tuft fracture, are common when the phalanx of a finger is subject to crush injury (e.g., by a door) and there exists a skin defect overlying a fractured bone. In a prospective randomized, placebo-controlled study of 193 patients with open fracture of the finger, flucloxacillin or placebo was administered to randomized patients with open phalangeal fractures, and both groups were treated with aggressive surgical irrigation and débridement. No significant difference was found in the infection rate between the groups, and no patient developed osteomyelitis. The data suggest that vigorous irrigation and débridement are adequate primary treatment for open phalangeal fractures in fingers with intact digital arteries.25 Such injuries might be repaired by the emergency physician without consultation. Because of the rich blood supply to the skeleton, fractures can result in large amounts of blood loss, shock, and death from exsanguination. In particular, certain pelvic fractures can cause great blood loss as adequate tamponade is not possible. In adults, blood loss can range from 100 mL from a forearm fracture to 3 L from a pelvic fracture (Table 49-3). Table 49-3 Blood Loss Associated with Fracture in Adults
General Principles of Orthopedic Injuries
Management Principles
FRACTURE EPONYM OR NAME
DESCRIPTION
COMMENT
Aviator’s
Vertical fracture of the neck of the talus with subtalar dislocation and backward displacement of the body.
First described in flyers during World War I. Arises from forced dorsiflexion of the foot in flying accidents and in traffic accidents after a head-on collision.
Barton’s
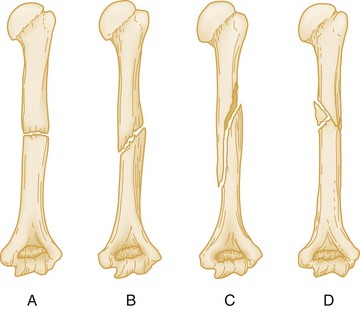
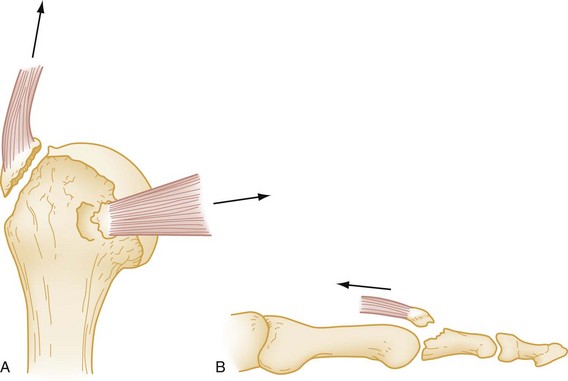
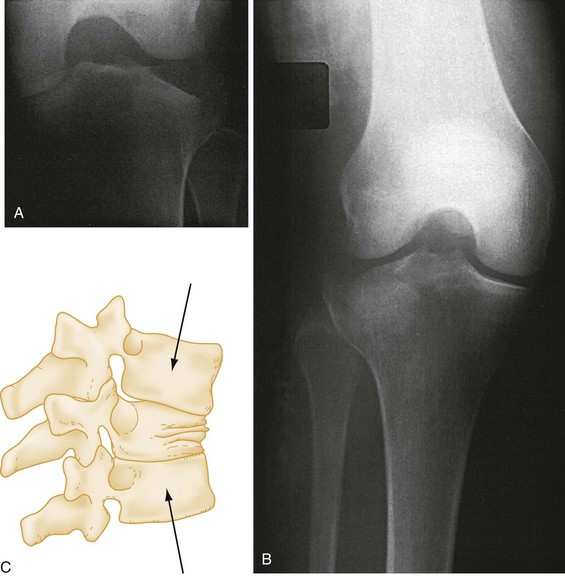
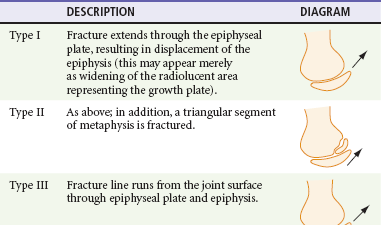
Intra-articular fracture-dislocation of the wrist.
Considered complicated and unstable. Requires surgical reduction in most cases. Described by Barton in 1838 before the advent of radiography.
Dorsal Barton’s
Oblique intra-articular fracture of the dorsal rim of the distal radius with displacement of the carpus along with the fracture fragment.
Results from high-velocity impact across the articular surface of the radiocarpal joint, with the wrist in dorsiflexion at the moment of impact.
Volar Barton’s
Wedge-shaped articular fragment sheared off the volar surface of the radius (volar rim fracture), displaced volarly along with the carpus.
Similar mechanism as dorsal Barton’s but with wrist in volar flexion at time of injury. Also referred to as reverse Barton’s fracture. Much rarer than dorsal Barton’s fracture.
Bennett’s
Oblique fracture through base of the first metacarpal with dislocation of the radial portion of the articular surface.
Usually produced by direct force applied to the end of the metacarpal. Dorsal capsular structures disrupted by the dislocation. Marked tenderness along medial base of thumb.
Bosworth
Fracture-dislocation of the ankle resulting in the fibula being entrapped behind the tibia.
Rare injury, produced by a severe external rotation force applied to the foot. Physical examination reveals foot severely externally rotated in relation to the tibia.
Boxer’s
Fracture of the neck of the fourth or fifth metacarpal.
Results from striking a clenched fist into an unyielding object, usually during an altercation, or against a wall, out of frustration or anger.
Chance’s
Vertebral fracture, usually lumbar, involving the posterior spinous process, pedicles, and vertebral body.
Caused by simultaneous flexion and distraction forces on the spinal column, usually associated with use of lap seat belts. Anterior column fails in tension along with the middle and posterior columns. May be misdiagnosed as a compression fracture.
Chauffeur’s
Solitary fracture of radial styloid.
Occurs from tension forces sustained during ulnar deviation and supination of the wrist. Name derives from occurrence in chauffeurs who suffered violent, direct blows to the radius incurred while turning the crank on a car, only to have it snap back, during previous eras.
Clay shoveler’s
Fracture of the tip of the spinous process of the sixth or seventh cervical vertebra.
First described in Australian clay shovelers who sustained a fracture of the spinous process by traction as they lifted heavy loads of clay.
Colles’
Fracture of the distal radius with dorsal displacement and volar angulation, with or without an ulnar styloid fracture.
Most common wrist fracture in adults, especially in the elderly. Results from fall on an outstretched hand. Also known as silver fork deformity, which accurately describes the gross appearance in the lateral view. First described by Colles in 1814, before the advent of radiography.
Cotton’s
Trimalleolar fracture.
Fracture of the lateral malleolus, fracture of the posterior malleolus, and either a fracture of the medial malleolus or a disruption of the deltoid ligament with visible widening of the mortise on ankle radiograph.
Dashboard fracture
Fracture of the posterior rim of the acetabulum.
Named for mechanism of injury: a seated passenger striking the knee on a dashboard, driving the head of the femur into the acetabulum.
Dupuytren’s
Fracture-dislocation of the ankle.
Results from a similar mechanism as the better known Maisonneuve fracture (i.e., external rotation of the ankle), resulting in either deltoid ligament rupture or medial malleolus fracture, diastasis of the inferior tibiofibular joint, and indirect fracture of the fibular shaft. Maisonneuve was the student of Dupuytren.
Essex-Lopresti
Fracture of radial head with dislocation of distal radioulnar joint.
Results from longitudinal (axial) compression of the forearm.
Galeazzi’s
Fracture of the shaft of the radius with dislocation of the distal radioulnar joint. Ligaments of inferior radioulnar joint are ruptured and head of ulna displaced from ulnar notch of the radius.
Results from fall on outstretched hand, with the wrist in extension and the forearm forcibly pronated. Inherently unstable with tendency to redisplace after reduction.
Hangman’s
Fracture-dislocation of atlas and axis, specifically of pars interarticularis of C2 and disruption of C2-3 junction. Separation occurs between second and third vertebral bodies from anterior to posterior side.
Results from extreme hyperextension during abrupt deceleration. Most common cause is the forehead striking the windshield of a car during a collision. A bit of a misnomer in that hanging usually produces death by strangulation rather than cord damage.
Hume’s
Fracture of the proximal ulna associated with forward dislocation of the head of the radius.
Essentially high Monteggia’s injury.
Jefferson’s
Burst fracture of ring of C1, or atlas.
Axial loading results in a shattering of the ring of the atlas. Decompressive type of injury. Associated with disruption of transverse ligament; an unstable injury.
Jones
Transverse fracture of the metatarsal base, occurring at least 15 mm distal to the proximal end of the bone, distal to the insertion of the peroneus brevis.
Should not be confused with the more common avulsion fracture of fifth metatarsal styloid, produced by avulsion at the insertion of the peroneus brevis. Jones described the fracture that bears his name in 1902, after sustaining the injury himself while dancing.
Le Fort
Maxillary fracture.
Types I, II, and III (see Chapter 42).
Le Fort-Wagstaffe
Avulsion fracture of the anterior cortex of the lateral malleolus.
Rare pull-off injury of the fibular attachment of the anterior tibiofibular ligament.
Lisfranc’s
Fracture located around the tarsometatarsal (Lisfranc’s) joint, usually associated with dislocation of this joint.
Lisfranc, a field surgeon in Napoleon’s army, described an amputation performed through the tarsometatarsal joint in a soldier who caught his foot in a stirrup when he fell off his horse. Since then, the joint has borne his name.
Maisonneuve
Fracture of proximal third of fibula associated with rupture of the deltoid ligament or fracture of the medial malleolus and disruption of the syndesmosis.
Results from external rotation of the ankle with transmission of forces through syndesmosis; proximally the force is relieved by fracture of the fibula. Described experimentally in 1840, before radiography.
Malgaigne’s
Fracture of the ilium near the sacroiliac joint with displacement of the symphysis, or a dislocation of the sacroiliac joint with fracture of both ipsilateral pubic rami.
Resultant pelvic injury is unstable. Described by Malgaigne, based on clinical findings, in 1847.
March
Fatigue, or stress, fracture of the metatarsal.
Arises from long marches or other repetitive use trauma (e.g., marathon running) or less commonly from single stumbling movements.
Monteggia’s
Fracture of the junction of the proximal and middle thirds of the ulna associated with anterior dislocation of the radial head.
Usually caused by fall on outstretched hand along with forced pronation of forearm or by a direct blow on the posterior aspect of the ulna. Reported by Monteggia in 1814.
Nightstick
Fracture of either ulna or radius, or both.
Name derived from a citizen’s attempt to protect himself from a police officer’s baton or “nightstick” by offering the forearm.
Piedmont
Closed fracture of the radius at the middle third–distal third junction, without associated ulnar fracture.
Named for a series of cases presented at the Piedmont Orthopaedic Society of Durham, North Carolina.
Pott’s
Definitions vary (see comment); most commonly a bimalleolar fracture or a fracture of the distal fibula, 4-7 cm above the lateral malleolus.
The exact fracture Pott described in 1769 is uncertain; clearly it referred to a fracture of the lower fibula, usually associated with other fractures or dislocations about the ankle.
Rolando’s
Intra-articular fracture at base of metacarpal. Frequently Y– or T-shaped, or may be severely comminuted.
Produced by an axial load with the metacarpal in partial flexion. Worse prognosis than a Bennett’s fracture and, fortunately, rarer.
Salter-Harris
An epiphyseal fracture occurring in children or adolescents.
Graded I-V, depending on degree of involvement and/or displacement of epiphysis and metaphysis (see text dealing with Salter-Harris fractures and also Figure 46-1).
Smith’s
Extra-articular fracture of the distal radius with volar displacement of distal fragment.
Reverse of the Colles’ fracture but much more uncommon. Sometimes referred to as a “garden spade” deformity. Usually results from fall with force to back of hand. First described by Smith in 1847.
Stener
Avulsion of the ulnar corner of the base of the proximal phalanx of the thumb.
Bony equivalent of rupture of the ulnar collateral ligament, or “gamekeeper’s thumb.”
Teardrop
Wedge-shaped fracture of the anteroinferior portion of the vertebral body, displaced anteriorly.
Commonly involves a ligamentous injury and may produce neurologic injury.
Thurston Holland’s fragment
Triangular metaphyseal fragment that accompanies the epiphysis in Salter-Harris type II fractures.
Described by Thurston Holland in 1929. The name is commonly hyphenated, although technically it should not be.
Tillaux
Isolated avulsion fracture of the anterolateral aspect of the distal tibial epiphysis.
Occurs in older adolescents (12-15 years) after the medial parts of the epiphyseal plates close but before the lateral part closes. External rotation force places stress on anterior talofibular ligament. Described by Tillaux in 1872.
Fractures
General Descriptors
Descriptive Modifiers
Fracture Eponyms
Fractures in Children
Diagnostic Modalities for Fracture Diagnosis
Special Imaging Techniques
Complications of Fractures
Hemorrhage
FRACTURE SITE
AMOUNT OF BLOOD LOSS (mL)
Radius and ulna
150-250
Humerus
250
Tibia and fibula
500
Femur
1000
Pelvis
1500-3000 ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


General Principles of Orthopedic Injuries
Only gold members can continue reading. Log In or Register to continue