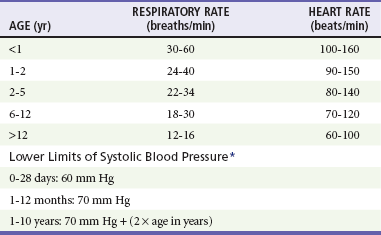
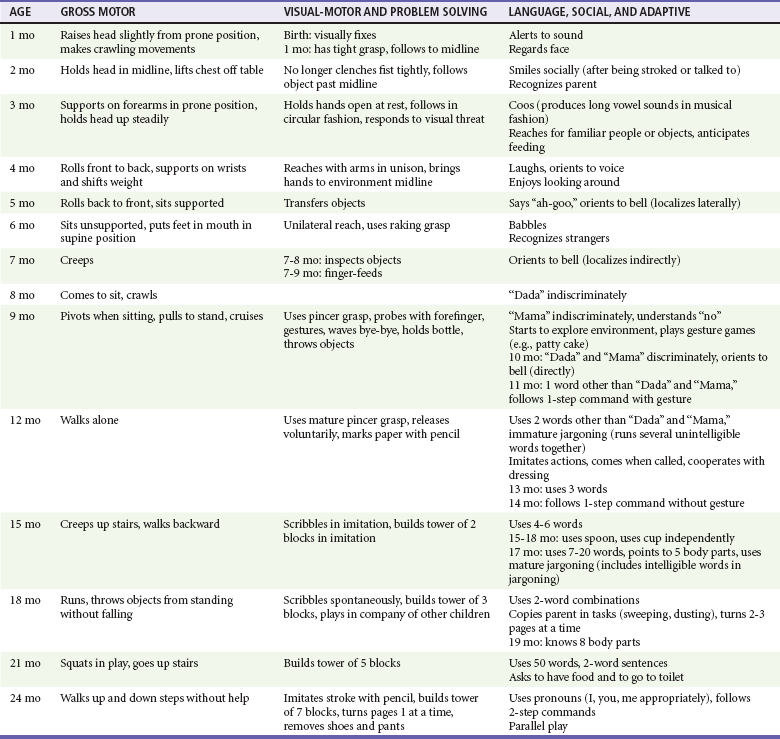
Chapter 166 Emergency medicine providers should be comfortable assessing and treating pediatric patients from the newly born through adolescence. Of the 124 million annual U.S. emergency visits, 23 million are for children younger than 15 years.1 Twenty percent of children have at least one emergency department visit per year.2 The age group with the highest emergency department use per capita is infants, with 85.5 visits per 100 infants.1 Although some hospitals have separate pediatric emergency departments, most pediatric patients are seen in general emergency departments. Several recent surveys found that more than 80% of pediatric patients are seen in general emergency departments.3,4 Therefore, all emergency providers need to be prepared to provide definitive treatment for many pediatric illnesses and injuries and to provide initial stabilization and treatment to critically ill and injured pediatric patients. In most patients, the first step in assessment is a review of vital signs. Normal ranges for vital signs vary significantly by age. Early recognition of abnormal vital signs will help the emergency provider detect physiologic decompensation in its earliest stages. Normal vital signs by age are listed in Table 166-1. Abnormal vital signs should be repeated, and persistently abnormal vital signs should not be ignored. Table 166-1 *From American Heart Association Emergency Cardiovascular Care (ECC) Guidelines, 2000. From Dieckmann R, Brownstein D, Gausche-Hill M (eds): Pediatric Education for Prehospital Professionals. Sudbury, Mass, Jones & Bartlett, 2000, pp 43-45. The pediatric airway differs in a number of ways from an adult airway.5 Numerous characteristics of the pediatric airway predispose to obstruction. Infants and young children have relatively large tongues, which may lead to airway obstruction during seizures or periods of altered mental status. Use of nasopharyngeal airways can be helpful in bypassing obstruction due to a relatively large tongue. The small airways of children are more easily obstructed with secretions. In addition, young infants preferentially breathe through their noses and can have significant respiratory distress from nasal secretions. For these reasons, airway suctioning can dramatically diminish an infant’s work of breathing. Infants and young children also have large occiputs, causing neck flexion and potential airway obstruction in the supine position. A shoulder roll can be used to properly position young patients; it may significantly decrease respiratory distress and improve intubating conditions (Fig. 166-1). Young infants are at increased risk of serious bacterial infections because of their immature immune system. Febrile infants younger than 1 month are an especially high-risk group and have an approximately 10% rate of serious bacterial infection.6 For this reason, the evaluation of infants with fever differs from the evaluation of older children and adults, and the workup varies by the age and vaccination status of the infant. Pediatric patients are particularly prone to medication errors for multiple reasons, including the fact that medications for children are calculated using weight-based dosing with attention to the adult maximum medication dose.7 Most calculation-based dosing errors occur in pediatric patients.7 Suggested safeguards include pharmacy review of medication orders, computerized order entry and use of templated order forms, resuscitation calculators, and length-based resuscitation tapes. One easily remedied potential error is the inadvertent calculation of a drug dose on the basis of weight in pounds, not kilograms, leading to a more than twofold overdose. For this reason, emergency department scales should be programmed to report weight in kilograms, not pounds, and weight in pounds should not be written in the medical chart. Assessment of pediatric patients requires some understanding of normal developmental milestones. Table 166-2 lists basic developmental milestones in the first 2 years of life. There will be variation in the rate at which children develop. Therefore, the parent’s report of the child’s developmental history and normal behavior is extremely important. Table 166-2 Developmental Milestones in Children Younger Than 2 Years Modified from Gunn KL, Nechyba C (eds): The Harriet Lane Handbook, 16th ed. St Louis, CV Mosby, 2003. Triage systems with pediatric modifications include the Emergency Severity Index, the pediatric Canadian Triage and Acuity Scale, the Manchester Triage System, and the Australasian Triage Scale.8 All of these systems are five-level triage systems. In five-level triage systems, level 1 patients require immediate intervention. Level 2 patients are emergent and should be seen within 10 to 15 minutes. Level 3 patients are considered urgent and should be seen within 30 to 60 minutes, depending on the triage system. Level 4 and level 5 are thought to be stable patients. The Emergency Severity Index classifies patients by acuity and number of resources expected to be required.9 A flowchart specific to pediatric patients with fever has been added. In the Canadian Triage and Acuity Scale, specific criteria for various presenting complaints are used to assign triage levels.10 The pediatric modification includes pediatric-specific presenting complaints and determination of acuity by use of pediatric-specific vital signs. The Manchester Triage System contains flowcharts based on presenting complaint, with some pediatric-specific flowcharts.11 The Australasian Triage Scale is mostly a general triage scale but has several pediatric-specific criteria.12 No triage system is clearly demonstrated to be superior, and data on reliability and validity are limited for all triage systems. The Emergency Severity Index, the Manchester Triage System, and the pediatric Canadian Triage and Acuity Scale have been demonstrated to be valid in pediatric patients.8,13,14 Reliability is good for the Manchester Triage System and moderate for the Emergency Severity Index and pediatric Canadian Triage and Acuity Scale.8,14 The Australasian Triage Scale appears to have lower reliability than the other triage systems.8 In critically ill or injured patients, the SAMPLE history can be used as a way to quickly obtain a focused history (Box 166-1). The SAMPLE history reminds providers to ask for Signs and symptoms, Allergies, Medications, Past medical history, Last meal, and Events surrounding the illness or injury.
General Approach to the Pediatric Patient
Perspective
Distinguishing Principles of Disease
Airway
Immunologic
Pharmacologic
Developmental
Evaluation
History
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


General Approach to the Pediatric Patient
Only gold members can continue reading. Log In or Register to continue





